Blood test for EDS - what is it? Express diagnosis of syphilis, which is abbreviated EDS, is one of the non-treponemal serological research methods of blood analysis. This test was proposed by an immunologist from Germany A. Wasserman, and it was named after him - the Wasserman reaction, or RW. Its main advantages are low cost, simplicity, and quick results.
Blood is donated for EDS during screenings, that is, mass examinations, to determine diseases in seemingly healthy people who do not have any alarming symptoms. Currently, such a test is considered obsolete and is being replaced by others, but still, when it comes to non-treponemal detection of syphilis, the following expression is used - “donate blood for RW”.
Description of the EDS blood test and its purpose
A blood test for EDS is taken not only by those patients who suspect that they have the disease or intend to confirm an already made diagnosis, but also by blood donors and pregnant women. Treatment of syphilis can be carried out through the use of antibiotics, but an untreated disease develops into a chronic form that affects all organs of the human body, and is also characterized by constant remissions and relapses.
The test is carried out in the following cases:
- If there is a suspicion of syphilis.
- To confirm the diagnosis of latent syphilis.
- If necessary, donor verification.
- Pregnancy tests.
- Screening.
How long does it take to perform a blood test for EDS? This test is very quick. Within half an hour you can analyze the result.
Treatment
Since myelodysplastic syndrome is a collective name for various syndromes of varying severity, treatment is determined by the leading symptoms and can be highly individualized. The choice of therapy depends, in addition to the diagnosed variant of myelodysplastic syndrome, on the patient’s age, membership in a risk group, the degree of cytopenia and its dynamics, the number of blast cells in the bone marrow, the presence and severity of concomitant pathology. Also an important factor is the presence of a potential bone marrow donor, since only allogeneic bone marrow transplantation leads to a permanent and complete cure.
It is important to note that patients with low and intermediate risk and with asymptomatic cytopenia, according to current concepts, do not need early treatment; they are recommended to be actively monitored to detect further progression of the disease (for example, an increase in cytopenia, an increase in the number of blast cells).
Symptomatic therapy includes the following treatment methods:
- Replacement therapy with blood components (donor red blood cells, donor platelets, fresh frozen plasma). Red blood cell transfusion is recommended in the presence of anemic syndrome, hypoxemia and hemoglobin levels below 85-90 g/l. Platelet transfusion is carried out when their level decreases to 10 × 10 9 \l or to the level of 20 × 10 9 \ l in case of risk of life-threatening bleeding (for example, with concomitant fever).
- Chelation therapy. Treatment to eliminate excess iron that may result from frequent blood transfusions. In addition, chelation therapy is indicated in preparation for bone marrow transplantation. The drug deferasirox is used for this purpose.
- Hematopoiesis stimulants. Prescribed to patients whose own erythropoietin has a level of at least 500 IU and a hemoglobin level below 100 g/l. Drugs such as epoetin alfa can increase these patients' own hemoglobin levels and thereby reduce the need for donor red blood cell transfusions. The drug is discontinued when the target level is reached (usually it corresponds to 110-120 g/l). A combination of epoetin and colony-stimulating factors is possible.
- Systemic hemostatics. Prescribed to increase platelet levels and prevent the development of hemorrhagic syndrome.
- Antibacterial therapy. Prescribed when infectious processes occur.
One of the possible approaches to the treatment of myelodysplastic syndrome may be the use of cytostatic therapy - drugs used for chemotherapy of malignant neoplasms and aimed at stopping the growth of pathological cells. Some drugs have not only a cytotoxic, but also a differentiating effect that promotes the maturation of blasts.
Patients from high-risk groups, if standard cytotoxic therapy is ineffective, can be prescribed polychemotherapy, similar to that carried out in patients with acute leukemia. The most commonly used combination is cytarabine and anthracycline drugs. This approach to treatment can lead to complete remission in 40-60% of cases, although its duration is quite limited. Therefore, even after achieving complete remission, maintenance chemotherapy can be prescribed - the same cytarabine, but in combination with 5-mercaptopurine. Cytarabine alone can be used in elderly patients (over 65 years of age) with refractory anemia with excess blasts of both types I and II. Such therapy can be used long-term, for up to 3 years, or until significant toxicity occurs.
Another group of chemotherapeutic drugs that has found its use in the treatment of myelodysplastic syndrome are hypomethylating agents. These include azacitidine and decitabine. Their use is indicated for intermediate-2 and high-risk patients who are not candidates for intensive chemotherapy or bone marrow transplantation, or, conversely, as induction therapy before transplantation.
Some patients who belong to low and intermediate risk groups may be given immunosuppressive therapy with drugs such as cyclosporine and antithymocyte globulin. Immunosuppressive therapy is used for a long time, at least two years.
Patients with 5q myelodysplastic syndrome may be prescribed a cytotoxic drug called lenalidomide. The optimal duration of its use has not been determined, but may be 24 months.
Depending on the course of the disease, patients may be prescribed a combination of different drugs or sequential prescription of drugs from different groups during the progression or transition of one disease to another (for example, an increase in blasts in refractory anemia with an excess of blasts, which allows changing the diagnosis from RAEB-I to RAEB -II).
In some patients, removal of the spleen may be indicated. The main indication is a significant enlargement of the organ, but such an operation can also be indicated for patients with signs of hematopoietic hypoplasia, provided there is no effect of immunosuppressive therapy, for patients with signs of autoimmune anemia or thrombocytopenia. The most preferred approach is laparoscopic.
In addition to the therapeutic effect, which consists in the ability to reduce the patient’s dependence on blood transfusions, removal of the spleen can also be of a diagnostic nature, since the histological examination will allow the attending physician to obtain more information about the course of the disease.
Bone marrow transplantation, as mentioned earlier, is currently the only radical treatment for myelodysplastic syndrome. However, the possibilities of its use are significantly limited, firstly, by the elderly age of the majority of patients and the presence of concomitant diseases, and, secondly, by the absence in most cases of a suitable donor. Favorable prognostic factors for transplantation are age younger than 60 years, the absence of blast cells in the bone marrow, and the absence of unfavorable chromosomal changes. The best results were demonstrated in patients from the low-risk group. The optimal timing for transplantation is considered to be performed before the transformation of myelodysplastic syndrome into acute myeloid leukemia.
Due to the possible development of toxicity as a side effect of the treatment, patients should be prescribed certain drugs for prophylactic purposes:
- Antiemetics - to prevent nausea and vomiting,
- Allopurinol - to prevent an increase in uric acid in the blood, if the patient is undergoing therapy with cytostatic drugs,
- Antibiotics - in case of development of febrile neutropenia in order to relieve infectious complications. Antibiotics are also prescribed in combination with antifungal agents during therapy with antithymic globulin,
- Antiplatelet therapy - used in lenalidomide therapy to prevent deep vein thrombosis,
- Antihistamines - used before transfusion of blood components.
Finally, during the entire period of treatment and during remission, it is necessary to avoid sun exposure, refuse to visit saunas and baths, not undergo physiotherapeutic procedures and, when working in hazardous work, it is advisable to change working conditions. In this case, harmful working conditions include severe physical and significant neuropsychic stress, exposure to toxic agents, vibration, and work with moving mechanisms. These measures prevent not only the progression of the disease, but also the development of relapse.
Carrier
The sick patient and his body fluids act as a carrier of syphilis. Infection is possible through sexual contact, through blood, or through the use of personal hygiene items. The disease is usually caused by indiscriminate sexual intercourse. The earlier the pathology is diagnosed, the faster and easier the treatment becomes. To take the test, you can simply donate blood on an empty stomach. If no other tests other than EDS are required, then you just need to not eat food for eight hours. The day before the test, you do not need to follow a special diet. Usually blood is taken from a vein, but it is also possible from a finger, since a large amount is not needed. What is an EDS (blood test)? Let's take a closer look.

If antibodies are detected
When antibodies are detected, it is possible to judge whether the infection has penetrated the human body to a certain extent. Cardiolipin, which takes part in the test, is a substance that is extracted from bovine heart. A special cardiolipin solution is combined with a small amount of blood in glass wells. The resulting solution is assessed after half an hour for the amount of precipitate obtained.
It is necessary to be aware of possible errors. A positive result does not always mean that the patient is sick. Although the test is quite effective, it still needs to be confirmed by other tests, so blood must be taken several times. This especially applies to pregnant women. In addition to determining the diagnosis, this test makes it possible to identify stages of the disease from the first to the fourth. Treatment is prescribed based on the information received.
Not everyone knows that this is a blood test for EDS.
Reasons for development
The causes of myelodysplastic syndrome are currently unknown. Only in 10-15% of cases, myelodysplastic syndrome develops in people who have previously received chemotherapy or radiation therapy for another disease. In other cases, predisposing factors may be smoking, contact with certain chemical compounds (gasoline, insecticides, pesticides, a number of organic substances). Also, one of the possible causes may be infection with parvovirus B19, since it is characterized by reproduction in the precursors of red blood cells.
The impact of damaging factors on bone marrow stem cells, which are the precursors of blood cells, leads to the formation of mutations in them, which will be reproduced as the cells divide. Further accumulation of mutations causes the transformation of myelodysplastic syndrome into acute leukemia.
Decoding the test for syphilis and normal indicators

During the EDS procedure, it is difficult to talk about a certain norm or its violations. The result in this case is either negative or positive. But in addition to this, there are also titers, which show how much antibodies are present in the blood. Each specific result must be deciphered by a specialist. There are a large number of different subtleties, and therefore there is no need to draw premature conclusions and try to decipher the analysis yourself or find the answer to the question of what it is - a blood test for EDS - using the Internet.
Forecast
Due to the development of cytopenic syndromes, especially with a decrease in the number of platelets, the disease itself can be life-threatening, but the main danger of myelodysplastic syndrome is its degeneration into acute leukemia. To assess overall life expectancy and the risk of transformation of myelodysplastic syndrome into leukemia, two scales are used - the International Prognostic Scoring System (IPSS) and the WHO scale. Both scales use a scoring system that evaluates karyotype, the presence of cytopenia (IPSS scale) or severe anemia (WHO scale), as well as the number of blasts in the bone marrow (IPSS scale) or the initial variant of myelodysplastic syndrome (WHO scale). According to the sum of points, the prognosis is assessed, and therapy and follow-up are planned.
Myelodysplastic syndrome combines several diseases, varying in severity and course; In addition, within the same disease, various manifestations with varying degrees of severity are possible. Unfortunately, myelodysplastic syndrome is currently a practically incurable disease, but timely consultation with a doctor, well-chosen therapy and careful follow-up can prevent malignant degeneration and control its course, preserving the patient a long life with minimal disruption to its quality.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Myelodysplastic syndrome. Clinical recommendations of the Association of Oncologists of Russia, 2021.
- Myelodysplastic syndrome in adults. National Society of Hematology Clinical Guidelines, 2014.
- Uss A.L. Myelodysplastic syndrome: classification, prognosis, treatment. Health and environmental problems. P.57-62.
- Kosanova A.K. et al. Refractory anemia and cytopenia as diagnostic criteria for myelodysplastic syndromes. Bulletin of KazNMU, 2015, No. 1. P. 131-133.
- Kokhno A.V. et al. Myelodysplastic syndrome. Clinical gerontology. 2009. No. 3. P. 33-46.
- Zeltser A.N. Myelodysplastic syndrome: difficulties and successes in diagnosis. Journal of Basic Medicine and Biology. 2021. No. 1. P. 27-37.
- Myelodysplastic Syndromes. NCCN Guideline version 2.2020.
Class affiliation of cells lgM or lgG
The class affiliation of the lgM or lgG cells is indicated: when treponema enters the body, the immune system begins to react violently to the penetration of foreign cells. First, antibodies such as lgM are formed. They can be detected within a week after a person becomes infected. IgG appears in the body after about a month and can remain in it for a long period, even if the disease has been successfully treated. The presence of this class may indicate that the body has developed a stable immune response to Treponema pallidum.
If the result is negative and the titres indicated with the word IgG next to them, one can judge the secondary nature of syphilis. That is, there are antibodies to Treponema pallidum in the blood, but these are memory antibodies that can circulate in the body for a long time after the patient has recovered. Such an analysis in some cases may be positive, although in fact it is a false positive. An accurate determination requires taking into account all previous research results and monitoring the decrease in titer. All subsequent tests may continue to give positive results.

The interpretation of the blood test for EDS should be carried out by a highly qualified specialist.
Laboratory detection of the causative agent of syphilis
Treponema pallidum (the causative agent of syphilis) belongs to gram-negative bacteria of the spirochete species. In 95% of cases, infection occurs through unprotected intimacy. Contagiousness (infectiousness) is manifested by the concentration of bacteria in the secretory fluids of an infected person (sperm, vaginal secretions) and microscopic damage to the mucous membranes of the partner.
The bacterium enters the intercellular junctions of the endothelium, cells and tissues, and multiplies in the lymph nodes. The high virulence of treponema pallidum ensures the rapid spread of infection throughout the body through the blood and lymph flow.
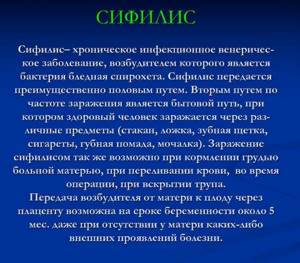
Treponema pallidum is not detected under a light microscope and does not grow on nutrient media, which excludes conventional microscopic analysis and bacteriological culture (bacteriological culture) from laboratory practice. The bacterium can only be detected in blood serum through serological tests.
RPR in the list of diagnostic methods for determining Treponema pallidum
Serological blood testing is based on the body’s immune reactions: the interaction of antigens (bacteria or viruses) that have entered the blood and Ig immunoglobulins - specific blood plasma proteins responsible for the differentiation and destruction of antigens.
Reference! Antibodies to foreign pathogens are called immunoglobulins, and serological reactions are called antigen-antibody reactions.
Treponemal and non-treponemal tests are used to diagnose syphilis. Treponemal testing is a complex and expensive method using actual Treponema pallidum antigens. They are necessary to confirm the diagnosis in case of false positive results.
The list includes reactions:
- immunofluorescence (RIF);
- immobilization of Treponema pallidum (RIBT);
- passive hemagglutination (RPHA).
Enzyme-linked immunosorbent assay (ELISA) and immunochemiluminescence (ICL) are similar. In non-treponemal tests, cheap nonspecific antigens are used for the antigen-antibody reaction and immunoglobulins are not separated by titers, but their total amount is determined. Non-treponemal studies include RPR, which is used to quickly diagnose syphilis.
How to determine the extent of damage?
It can give both positive and negative results. The more serious the defeat is, the more advantages there are in the indicators.
- weakly positive reaction - + and ++ (if plus one, then the result is doubtful);
- positive — +++;
- strongly positive - ++++.
Based on the results of the analysis, antibody titers are indicated. When conducting a therapy monitoring study, titers help determine whether the patient is recovering. As a rule, after treatment the patient is under the supervision of specialists for a year. During this period, he is tested several times. The effectiveness of therapy is also evidenced by a decrease in titers over the year by four or more times. In the absence of IgM immunoglobulins in the blood, we can talk about the absence of resumption of infection. The presence of IgG is possible for a long time after treatment, and sometimes even throughout life.

Evaluation of the effect of the treatment
The significant variety of clinical manifestations of various diseases, united under the concept of “myelodysplastic syndrome,” makes it difficult to develop a general scale according to which it is possible to evaluate the effectiveness of treatment. Currently, the IWG (International Working Group) classification is used, which includes the following options:
- Complete remission - no more than 5% or 30×10 9 /l blast cells are detected in the bone marrow, in the peripheral blood the hemoglobin level is more than 110 g/l, the number of neutrophils is 1.0×10 9 /l or more, blast cells are not detected ,
- Partial remission - in the bone marrow the number of blast cells is more than 5%, but has decreased by 50% or more from the initial value, peripheral blood indicators are similar to the criteria for complete remission,
- Bone marrow remission - in the bone marrow the number of blast cells is more than 5%, but has decreased by 50% or more from the initial value,
- Stabilization - no signs of partial remission and no signs of disease progression within 8 weeks,
- Cytogenetic remission - a complete remission is distinguished, a prerequisite for which is the disappearance of the original karyotype abnormalities and the absence of newly appeared ones. A decrease in the number of cells with chromosomal abnormalities by 50% or more is regarded as partial cytogenetic remission.
A separate condition is called hematological improvement. To establish it, the following criteria must be met and maintained for at least 8 weeks:
- Erythroid response. Initially, the hemoglobin level was less than 110 g/l; if there is a response, hemoglobin increases by 15 units or more, and the need for red blood cell transfusions decreases.
- Neutrophil response. The initial number of neutrophils is less than 1.0×10 9 /l. There is an increase in the number of neutrophils by more than 100% of the initial values, and their absolute number is more than 0.5×10 9 /l.
- Platelet response. The initial platelet count is less than 100×10 9 /l. The absolute platelet count should increase to 30×10 9 /L or more, or if the initial platelet level was less than 20, increase to 20×10 9 /L and at least double.
The progression of the disease is also determined according to certain criteria:
- reduction in the number of granulocytes or platelets by at least 50% of the maximum value for the entire course of the disease,
- decrease in hemoglobin level by 20 g/l or more,
- increase in blast cells by 50% or more,
- emergence of dependence on cell transfusions,
- worsening cytopenia with stable blast cell counts.
Transformation into acute myeloid leukemia is determined when more than 20% blast cells are detected in bone marrow or peripheral blood aspirate.
Positive EDS blood test result
What is this? It must be remembered that this method has certain disadvantages. The study is ordered to confirm suspicions, but you can’t count on a reliable result in all cases.
The Wasserman reaction can have positive indicators not only for syphilis, but also for malaria, lupus, and tuberculosis. Unfortunately, a more efficient and accurate method is still missing. Often this analysis is carried out simultaneously with others for a more complete picture. In pregnant women, the result may be positive even in the absence of any pathologies. It can also become false during menstruation. It is better to find out in advance how long a blood test for EDS is done.
Recheck the test
If you receive a positive result, you must recheck it several times. The patient has the right to take other tests and request confirmation, since EDS is not 100% reliable. If ulcers or chancres appear, but they do not hurt or bleed, we can judge that an infection has occurred. You need to immediately contact a specialist. The patient must find out all the details of therapy, the effect and composition of the prescribed drugs.

During pregnancy, preventive treatment is possible and does not need to be abandoned. If a woman was treated for syphilis before pregnancy (or in its early stages), the doctor may prescribe a preventive medication course. The patient also has the right to demand absolute anonymity. The doctor cannot talk about diagnoses and therapy.
There is no need to delay treatment, as it occurs faster in the initial stages. It is necessary to give up fatty and heavy foods, alcohol and anything that can complicate the recovery process.
We looked at the EDS - blood test. What this is is now clear.
Diagnostics
When collecting anamnesis, the doctor pays attention to the time of the first complaints, their dynamics, concomitant diseases and especially the therapy carried out for them, the presence of occupational hazards. During examination, the following manifestations of various syndromes may attract attention:
- Paleness of the skin and mucous membranes,
- Presence of signs of hemorrhagic syndrome (multiple bruises, hematomas, hemorrhages in the mucous membranes),
- Edema,
- Enlarged spleen and lymph nodes;
- Disturbances in the functioning of the central nervous system, cardiovascular, pulmonary, urinary, endocrine and osteoarticular systems, gastrointestinal tract.
The next stage of the diagnostic search is laboratory tests.
The main test to detect cytopenia is a complete blood count. Its main features are the following:
- Decrease in hemoglobin below 110 g/l,
- Decrease in the absolute number of neutrophils below 1.8 × 10 9 \l,
- Reduction of platelets below 100×10 9 \l.
Either an isolated decrease in one of the indicators or a combination of them can be observed. It is important to note that the decrease in indicators must be long-term, persistent (for at least 6 months) and have no other reasons.
All patients in whom myelodysplastic syndrome is suspected are recommended to undergo puncture and trepanobiopsy of the bone marrow, followed by histological and, if necessary, immunohistochemical studies.
Since the complaints arising from myelodysplastic syndrome are nonspecific and can be manifestations of other diseases, criteria have been developed on the basis of which the diagnosis is made. Necessary, decisive and additional criteria are identified.
Necessary criteria include stable cytopenia, caused by damage to at least one hematopoietic lineage in the bone marrow, for at least 4 months; detection of characteristic karyotype changes during cytogenetic examination of bone marrow punctate.
Decisive criteria include:
- dysplasia ≥10% of all cells of one of the hematopoietic lineages, identified during morphological examination of the bone marrow;
- ring sideroblasts in an amount of 15% or more, or 5% or more if the SF3B1 mutation is detected;
- 5–19% blast cells in the bone marrow or 2–19% blast cells in the peripheral blood;
- typical karyotype abnormalities (-7, 5q-, etc.) identified by standard cytogenetic testing or FISH.
Additional criteria are taken into account if the necessary criteria are present and the decisive criteria are absent. These include an atypical immunophenotype of bone marrow cells, bearing features characteristic of myelodysplastic syndrome, and characteristic changes in the histological picture of the bone marrow.
It should be noted that the diagnosis can also be made for less significant cytopenia (for example, hemoglobin 115 g/l, platelet count >100×10 9 /l), if a cytogenetic study of the bone marrow reveals significant changes in the karyotype.
In order to exclude other diseases and individualize treatment tactics, the following tests are also recommended:
- General urine analysis - to diagnose concomitant pathologies, as well as to assess the development of kidney toxicity during therapy;
- Biochemical blood test - to identify the presence of signs of destruction of blood cells, concomitant pathology, as well as assess side effects from the therapy;
- Study of serum indicators of iron metabolism - to assess its initial level and changes in the latter during treatment;
- Determination of the level of vitamin B12 and folic acid - to assess the content of B vitamins and prescribe appropriate therapy for their deficiency;
- Studying the level of erythropoietin in the blood is important for patients with anemic syndrome who are scheduled for red blood cell transfusion as part of the therapy;
- A blood test using flow cytometry to identify a clone of paroxysmal nocturnal hemoglobinuria cells is used if the patient has less than 5% of blast cells in the bone marrow and signs of intravascular hemolysis (destruction of blood cells) are detected. Since these cells are detected in 18–25% of patients with myelodysplastic syndrome, this necessitates correction of treatment tactics;
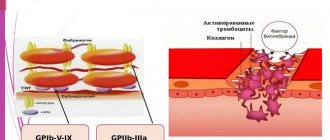
- Coagulogram - to determine the state of the blood coagulation system;
- Determination of the level of immunoglobulins - in case of development of infectious complications;
- Determination of the amount of copper, lead and zinc in peripheral blood. Indicated for identifying sideroblast cells;
- Study of markers of connective tissue inflammation (antistreptolysin-O, rheumatoid factor) - in order to exclude an autoimmune disease as a cause of cytopenia;
- Analysis of the level of thyroid hormones - to exclude hypothyroidism;
- Examination of peripheral blood and/or bone marrow aspirate for parvovirus B19, since it is one of the causes of the development of myelodysplastic syndrome and requires the appointment of special antiviral therapy. It is carried out when anemia is diagnosed and the bone marrow progenitor of red blood cells is suppressed by 10% or more.
Finally, patients can be prescribed a number of instrumental examinations aimed at identifying concomitant diseases and excluding other causes of cytopenia:
- Ultrasound of the abdominal cavity and retroperitoneal space, thyroid gland, pelvic organs for women and prostate gland for men;
- MRI of the brain,
- CT scan of the chest,
- EGDS.
It should be especially emphasized that the identified violations must be persistent and detected within the framework of two or three examinations performed within 6-12 months.
Thus, we can conclude that in case of suspected myelodysplastic syndrome, a thorough and complete examination is necessary in order to exclude all possible other diseases that can become a source of symptoms, primarily cytopenia.