A cyst is a benign neoplasm in the ovarian cortex, formed due to a disruption in the process of release of the corpus luteum of the follicle. Pregnancy after removal of an ovarian cyst is a topic that interests many women who have undergone laparoscopy or full abdominal surgery. Any functional disturbances in the functioning of the genital organs and surgical interventions in the pelvis bother women, because... theoretically reduce the chance of conception. But are ovarian cysts as dangerous for reproductive function as many women who want to have children think? This is interesting to many women: pregnant women, those who have given birth, and those who are just planning motherhood.
Could a cyst be a sign of more serious problems?
According to statistics, cysts most often go away on their own during one or several menstrual cycles, after which normal ovarian function is resumed - the maturation of follicles and the release of eggs. In this case, it is easy to understand whether it is possible to get pregnant.
But there are a number of other negative factors:
- hormonal imbalances;
- surgical interventions;
- injuries.
They negatively affect female reproductive function in general, and the functioning of the ovaries in particular. Hormonal imbalance is one of the key factors that reduces the efficiency of the ovaries and complicates a woman’s reproductive function. When the body's hormone balance changes towards androgens (testosterone), ovarian function suffers.
One of the dangerous complications that reduces the ability to conceive is polycystic ovary syndrome. In this condition, many small cysts form on the surface of the ovaries, containing eggs. When the balance of sex hormones changes towards androgens, the process of egg release slows down or stops altogether.
Treatment of infertility associated with endometriosis
Surgical treatment for infertility remains the first step for infertility associated with endometriosis.
Surgical treatment for infertility associated with endometriosis is a pragmatic approach. (Paolo Vercellini, Edgarto Somigliana, Paolo Vigano, Annalisa Abbiati). There were 14 RCTs, which clearly demonstrated that the cumulative incidence of pregnancy during laparoscopic treatment and removal of endometriosis sites from 6 to 18 months in 50% of cases, pregnancy occurs. In women with minimal to mild endometriosis (ASRM), laparoscopic intervention, compared with diagnostic laparoscopy, is an effective method of increasing pregnancy/live birth rates. (Jacobson, et al. 2010). Cumulative 3-year spontaneous pregnancy rates range from 46 to 77% for mild endometriosis and 44 to 74% for severe endometriosis (Nezhat et al., 1989).
During laparoscopy, a number of indicators of the Fertility Index for endometriosis (Endometriosis fertility index (EFI), proposed by GD Adamson, are calculated. EFI has a prognostic value: it allows you to predict the time of pregnancy and use expectant management in patients with a good prognosis, or immediately begin ART procedures with an unfavorable one forecast.
In women with infertility due to endometriosis who undergo laparoscopic intervention before ART, clinicians may consider complete surgical removal of endometriotic lesions to improve live birth rates (Opoien et al., 2011).
Does surgery affect fertility?
An ovarian cyst is formed when, for some reason, a mature follicle does not rupture, releasing an egg into the fallopian tube towards the uterus, but remains in the ovary. Under the influence of hormones, the follicle begins to fill with fluid, forming a sac with a diameter of several millimeters to several centimeters. This happens under the influence of female and male sex hormones, stress, trauma and other factors.
Is it possible to get pregnant in this case? A single cyst does not always mean a serious problem. If, according to the gynecologist's indications, the cyst was removed, then the ability to conceive and bear a child is preserved. Pregnancy after an ovarian cyst is quite possible if a woman follows simple rules after surgery.
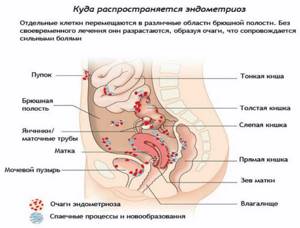
Endometriosis and infertility - problems of the modern woman
Endometriosis is one of the pressing problems of modern medicine, remaining one of the most mysterious and difficult to explain diseases.
The frequency of endometriosis, according to different researchers, varies from 12 to 50% in women of reproductive age. According to the latest data, approximately 176 million women of predominantly reproductive age suffer from endometriosis worldwide - one in ten. In Russia, GE ranks third in the structure of gynecological pathology (after inflammatory diseases and uterine leiomyoma). The frequency of detection of endometriosis during laparoscopy, including those performed to clarify the cause of infertility, is 20-55%. Among those turning to assisted reproductive technology centers for IVF, more than 30% of patients have external genital endometriosis.
How to avoid complications?
The main thing after surgery in the pelvic cavity is to avoid the formation of adhesions. To restore blood circulation in the reproductive organs, the woman should begin to move the next day after surgery. To avoid inflammation after surgery, antibiotics are prescribed for 5-7 days.
In gynecological practice, before an operation to remove a cyst, the gynecologist prescribes a hormonal examination to understand whether a woman can become pregnant at all. If a specialist discovers that there is an imbalance of gonadotropins (sex hormones), then after removing the cyst, the doctor prescribes hormonal medications to restore normal function of the endocrine system. Usually, complete elimination of all unfavorable factors affecting conception occurs within 2-3 months.
The possibilities of laparoscopic operations in pregnant women with surgical and gynecological pathologies are presented: cholelithiasis, appendicitis, hernias of the anterior abdominal wall, diseases of the uterine appendages, myomatous nodes. The advantages of laparoscopy, possible complications in the form of acidosis or damage to the uterus by the trocar, and their prevention are described. It has been shown that elective surgeries performed in the second trimester of pregnancy provide optimal results. Particular attention is paid to the problem of preventing uterine rupture during pregnancy after a previous conservative myomectomy.
Laparoscopic surgery and pregnancy
Possibilities of laparoscopic surgery in pregnant women with surgical and gynecological pathology are presented: with gallstones, appendicitis, hernia of the anterior abdominal wall, diseases of the uterine appendages, myomatosis nodes. The advantages of laparoscopic surgery, possible complications as acidosis or uterine trocar injuries, their prevention are described. Shown that optimal results provide planning surgeries performed in the second trimester of pregnancy. Particular attention is paid to the prevention of uterine rupture in pregnancy after undergoing before conservative myomectomy.
Complications of laparoscopy in pregnant women
Pregnancy presents a unique challenge to the surgeon when it comes to performing elective and emergency operations. And not only because we are talking about two human lives. During pregnancy, many physiological parameters undergo significant changes: cardiopulmonary, blood clotting, hemoglobin level, blood pressure. As pregnancy progresses, surgical imaging changes significantly, not to mention access. One or another operation on the abdominal organs is necessary during pregnancy for one in 150 women [1].
Traditionally, pregnancy was considered an absolute contraindication for laparoscopy, but in the last decade it has come forward in the treatment of gynecological and non-gynecological pathologies, in contrast to laparotomy. The most common surgery during pregnancy is cholecystectomy (45-48% of procedures), interventions on the uterine appendages (28-34%) and appendectomy (15-16%). Each of them gives good results in experienced hands [2].
There are several indications for gynecological surgery during pregnancy: benign ovarian cysts, torsion of the uterine appendages, cancer and, in rare cases, necrosis of the myomatous node. It is estimated that one in 81 pregnant women will have an ovarian cyst. Detection rates have increased in recent years with the widespread adoption of ultrasound. However, only one out of 600 women in the second trimester of pregnancy are diagnosed with benign ovarian cysts that require surgical treatment [3].
Most cysts detected on ultrasound are corpus luteum cysts and resolve on their own. Unfortunately, in some cases the clinical situation requires immediate intervention before expected resolution. Ovarian torsion is usually observed in the first trimester with an incidence of 1 in 5000 pregnancies [4].
Indications for surgery on the ovaries during pregnancy are dictated by two factors: the risk of malignancy of cysts, amounting to 1-8%, and the likelihood of complications in the form of torsion, rupture, bleeding with a frequency of 10-42%. The risk of premature birth after an urgent operation is much higher than after a planned one. Therefore, the risk of watchful waiting and refusal of surgery is very high [5, 6].
Advantages of laparoscopy. For the treatment of diseases that occur during pregnancy, laparoscopy has significant differences from laparotomy. Firstly, these are the same advantages as non-pregnant women: a reduction in the length of hospital days and rehabilitation periods, a reduction in the frequency of complications and the need for narcotic drugs, which is important for the life of the fetus [7, 8].
The previously existing opinion about the danger of laparoscopy in comparison with laparotomy for the life of the fetus has not been confirmed by numerous experiences in recent years. In a large Swedish retrospective study of 2181 laparoscopies and 1522 laparotomies performed during pregnancies over two decades, there were no differences in weight, gestation length, congenital malformations, stillbirths or neonatal deaths [9]. Two retrospective studies conducted in Israel confirmed the same [7, 10].
Theoretically, laparoscopy provides better visualization and requires less manipulation of the uterus, which subsequently prevents early labor. Laparoscopy is more effective in diagnostic terms, which is especially important for excluding acute appendicitis (OA). From 35 to 50% of cases of suspected OA in the third trimester are negative. Errors in this situation are very sad; many complications are associated with a delay in the diagnosis of inflammation of the appendix. Reduction of disease duration through diagnostic laparoscopy represents an ideal surgical model for resolving the dilemma necessarily present in a critical situation. Muench et al showed that delaying surgery for cholelithiasis increases the duration of the disease compared with timely laparoscopic treatment [11].
One possible advantage of laparoscopy over laparotomy is a reduced risk of thrombotic complications. Venous stasis and physiological factors associated with blood clotting during pregnancy increase the risk of catastrophic complications in the general population. Surgery only increases this risk. Many physicians believe that early ambulation after surgery resulting from minimally invasive surgery can significantly reduce this risk for the patient [12].
Prevention of complications. The long-standing ban on laparoscopy in pregnant women was based largely on the theoretical risks associated with insufflation and pneumoperitoneum (PP). Pregnancy, like obesity, significantly changes the patient's pulmonary ventilation mechanism. The body's metabolic demands increase and residual lung capacity decreases as pregnancy progresses. General anesthesia, increased intra-abdominal CO2 pressure, PP, supine position, and Trendlenburg position all combine to aggravate these problems. The result may be respiratory acidosis, atelectasis and hypoxemia. If these phenomena are not eliminated, embryonic acidosis and fetal hypoxemia will occur. The cardiac index decreases as anesthesia is introduced, as in non-pregnant patients. Blood pressure and systemic vascular resistance are reduced.
Fetal acidosis during insufflation 10-15 mm Hg. Art. studied in pregnant sheep. There was no hypoxemia in the embryos. Another danger of fetal acidosis is associated with an increase in intra-abdominal pressure, including a decrease in maternal venous return and cardiac output, a decrease in uterine blood flow and transperitoneal and placental absorption of CO2. These hypotheticals have been rejected by animal studies. All this did not affect the course of pregnancy in sheep; the adverse effect of PP on the condition of the fetus has not been proven [13, 14].
Another danger is damage to the pregnant uterus by the first trocar or Veress needle. The likelihood of this complication depends on the size of the uterus. Cases of pneumoamnion with fetal loss in the second trimester of gestation have been described [15]. As pregnancy progresses, safe insertion of the first trocar becomes increasingly difficult. The technique of open laparoscopy according to Hasson is shown.
After 18 weeks of pregnancy, the primary trocar is inserted significantly above the navel, along, between it and the xiphoid process of the sternum. The left upper quadrant of the abdominal wall or ultrasound guidance for needle insertion can be used [16, 17].
Elective laparoscopic surgery is ideally performed in the second trimester, when organogenesis is complete and the uterus is not yet as large as in the third trimester, although visualization of internal organs in the first trimester is naturally easier. Delaying surgery until the third trimester is undesirable due to poor visualization and the potential for preterm birth. Most authors do not routinely use tocolytics after laparoscopy, although indomethacin, ketoprofen and ritodrine give good results with increased uterine tone after laparoscopy [18].
To reduce the risk of thromboembolism, pneumatic compression stockings and early mobilization are indicated. Maternal hypoxia, tachycardia, the possibility of pleurisy, and arterial hypertension should be closely monitored after surgery [19].
Uterine rupture after laparoscopic myomectomy
This complication has been well known since the last century. Kurt Semm performed the first laparoscopic myomectomy in 1979, and in the following decade, at least 13 spontaneous uterine ruptures in the late second or early to mid-third trimester after laparoscopic myomectomy were described in the English-language literature. All of them occurred before the onset of labor [20, 21]. In general, uterine rupture after conservative myomectomy is observed in 0.33% of cases [22]. Although in some observations the frequency of this complication reaches 2.5% [23].
The main cause of the complication is inadequate suturing of the uterine wound or the leaving of “dead space,” which leads to the formation of intrauterine hematomas and impairs wound healing. It should be remembered that gynecologists are minor masters in suture technique. Monopolar electrosurgery and poor wound alignment also play a role in the risk of rupture [24–26].
Prevention . Because of the strain of the uterus during pregnancy, women planning a pregnancy after laparoscopic myomectomy should be carefully selected for this procedure. If there are more than four fibroids or if the dominant fibroid is more than 7-10 cm in diameter, laparotomy is indicated as the most effective procedure. Caution is necessary when localizing myomatous nodes along the posterior wall, since they are more difficult to suturing than formations localized in the fundus and along the anterior wall of the uterus. Suturing is especially difficult when myomatous nodes are localized along the posterior wall. An analysis of the literature shows that with such localization of fibroids, surgeons previously sutured only the serous membrane or did not do this at all. If these limitations are met, the laparoscopic approach is preferable [27, 28].
The importance of surgical technique in preventing uterine rupture cannot be overstated. However, minimizing thermal exposure to tissue during fibroid enucleation is the first important step in preventing possible complications. This is especially true for the use of monopolar energy in coagulation mode in the lower segment of the uterus, with prolonged effects on tissue. Scissors, ultrasonic scalpel, monopolar electrosurgery in cutting mode, and laser are preferable to minimize myometrial burn. Another important point is reliable hemostasis. Some surgeons recommend subserosal administration of vasopressin before uterine incision; some recommend treatment with gonadotropin-releasing hormone agonists for 1-3 months before surgery.
It is quite difficult to ensure reliable hemostasis with cold scissors or monopolar cutting. Therefore, a harmonic scalpel or laser is recommended for the initial dissection of the uterus. Simple dislocation of the node with blunt dissection is also possible. One of the advantages of endosurgery is clear visualization of the vascular pedicle; it can be treated in a bipolar mode. If bleeding continues, fulguration should be applied to a large area. The most reliable method of hemostasis is wound suturing. All layers of the uterus should be brought closer together and the dead space should be eliminated. The serosa should always be sutured, even with pedunculated fibroids and superficial subserous fibroids. Complete sealing requires 2-4 rows of sutures. In case of penetration into the uterine cavity, the endometrium must be sutured separately from the overlying myometrium. It is possible to use an interrupted or continuous suture, but the suturing must be reliable [29, 30].
The use of staplers may encounter certain difficulties in laparoscopic surgery. However, the results show the reliability of these sutures during subsequent pregnancy and childbirth. To control the tightness of the sutures, it is possible to inject methylene blue into the cervical canal. Uterine wound healing and myometrial thickness after surgery but before pregnancy can be monitored using ultrasound or MRI. The question of the duration of the pause between myomectomy and pregnancy has not been completely resolved. The strength of the myometrial scar reaches preoperative levels after 6-12 weeks. A prudent interval between surgery and pregnancy starts from three months [31, 32].
Recognition. The literature does not describe a single case of uterine rupture during childbirth after previously performed conservative laparoscopic myomectomy. Antepartum ruptures are observed from 17 to 35 weeks of gestation with a predominance of the late second or early third trimester. Any woman with a history of myomectomy, regardless of approach, with abdominal pain after 20 weeks' gestation should be considered for suspected uterine rupture. Symptoms of rupture are variable and nonspecific. Characterized by acute pain in the lower abdomen, fetal tachycardia is synchronous with the pain syndrome. The outcome for mother and child depends on the degree of blood loss and the depth of hypovolemic shock. When there is a threat of rupture, the most informative method is to determine the integrity of the myometrium using MRI [33, 34].
Treatment. Uterine rupture requires immediate caesarean section. The tear line should be sutured with a multi-row suture, as with an open myomectomy. Every woman who has undergone laparoscopic myomectomy will be faced with the question: will she survive childbirth or not? Of course, every obstetrician in such a situation carefully examines the scar and often recommends a cesarean section before labor occurs. There is no evidence that surgical delivery is safer in this situation. Successful vaginal delivery after laparoscopic myomectomy was observed in 38% of cases without a single uterine rupture [35].
I.V. Fedorov
Kazan State Medical Academy
Fedorov Igor Vladimirovich - Doctor of Medical Sciences, Professor of the Department of Endoscopy, General and Endoscopic Surgery of KSMA
Literature:
1. Lachman E., Schienfeld A., Voss E. et al. Pregnancy and laparoscopic surgery. J Am Assoc Gynecol Laparosc 1999; 6:347.
2. Reedy MB, Galan HL, Richards WE et al. Laparoscopy during pregnancy. A survey of laparoendoscopic surgeons. J Reprod Med 1997; 42:33.
3. Fatum M., Rojansky N. Laparoscopic surgery during pregnancy. Obstet Gynecol Surv 2001; 56:50.
4. Wang CJ, Yen CF, Lee CL, Soong YK Minilaparoscopic cystectomy and appendectomy in late second trimester. JSLS 2002; 6:373.
5. Stepp KJ, Tulikangas PK, Goldberg JM et al. Laparoscopy for adnexal masses in the second trimester of pregnancy. J Am Assoc Gynecol Laparosc 2003; 10:55.
6. Stepp K., Falcone T. Laparoscopy in the second trimester of pregnancy. Obstet Gynecol Clin North Am 2004; 31:485.
7. Oelsner G., Stockheim D., Soriano D. et al. Pregnancy outcome after laparoscopy or laparotomy in pregnancy. J Am Assoc Gynecol Laparosc 2003; 10:200.
8. Curet MJ, Allen D, Josloff RK et al. Laparoscopy during pregnancy. Arch Surg 1996; 131:546.
9. Reedy MB, Kallen B., Kuehl TJ Laparoscopy during pregnancy: A study of five fetal outcome parameters with use of the Swedish Health Registry. Am J Obstet Gynecol 1997; 177:673.
10. Soriano D., Yefet Y., Seidman DS et al. Laparoscopy versus laparotomy in the management of adnexal masses during pregnancy. Fertil Steril. 1999; 71:955.
11. Muench J., Albrink M., Serafini F. et al. Delay in treatment of biliary disease during pregnancy increases morbidity and can be avoided with safe laparoscopic cholecystectomy. Am Surg 2001; 67:539.
12. Carter JF, Soper DE Operative laparoscopy in pregnancy. JSLS, 2004; 8:57.
13. Chan JK, Morrow J., Manetta A. Prevention of ureteral injuries in gynecologic surgery. Am J Obstet Gynecol 2003; 188:1273.
14. Williams T J. Urologic injuries. Obstet Gynecol Annu 1975; 4: 347.
15. Berkmen R., Peker AE, Alagol H. et al. Treatment of iatrogenic ureteral injuries during various operations for malignant conditions. J Exp Clin Cancer Res 2000; 19:441.
16. Wood EC, Maher P., Pelosi MA Routine use of ureteric catheters at laparoscopic hysterectomy may cause unnecessary complications. J Am Assoc Gynecol Laparosc 1995; 3: 393.
17. Dwyer PL, Carey MP, Rosamilia A. Suture injury to the urinary tract in urethral suspension procedures for stress incontinence. Int Urogynecol J Pelvic Floor Dysfunction 1999; 10:15.
18. Fatum M., Rojansky N. Laparoscopic surgery during pregnancy. Obstet Gynecol Surv 2001; 56:50.
19. Rizzo AG Laparoscopic surgery in pregnancy: Long-term follow-up. J Laparoendosc Adv Surg Tech A 2003; 13:11.
20. Nouira Y., Oueslati H., Reziga H., Horchani A. Ureterovaginal fistulas complicating laparoscopic hysterectomy: A report of two cases. Eur J Obstet Gynecol Reprod Biol 2001; 96:132.
21. Oh B., Kwon D., Park K. et al. Late presentation of ureteral injury after laparoscopic surgery. Obstet Gynecol 2000; 95:337.
22. Nezhat C., Nezhat F. Laparoscopic repair of ureter resected during operative laparoscopy. Obstet Gynecol 1992; 80:542.
23. Liu CY, Kim JH, Bryant JF Laparoscopic ureteroureteral anastomosis of the distal ureter. J Am Assoc Gynecol Laparosc 2001; 8:412.
24. Seinera P., Farina C., Todros T. Laparoscopic myomectomy and subsequent pregnancy: Results in 54 patients. Hum Reprod 2000; 15: 1993.
25. Seinera P., Arisio R., Decko A. et al. Laparoscopic myomectomy: Indications, surgical technique and complications. Hum Reprod 1997; 12: 1927.
26. Ribeiro SC, Reich H, Rosenberg J et al. Laparoscopic myomectomy and pregnancy outcome in infertile patients. Fertil Steril 1999; 71:571.
27. Oktem O., Gokaslan H., Durmusoglu F. Spontaneous uterine rupture in pregnancy 8 years after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc 2001; 8:618.
28. Hasson HM, Rotman C, Rana N et al. Laparoscopic myomectomy. Obstet Gynecol 1992; 80:884.
29. Hasbargen U., Summerer-Moustaki M., Hillemanns P. et al. Uterine dehiscence in a NULLipara, diagnosed by MRI, following use of unipolar electrocautery during laparoscopic myomectomy: Case report. Hum Reprod 2002; 17:2180.
30. Pelosi MA 3rd, Pelosi MA Spontaneous uterine rupture at thirty-three weeks subsequent to previous superficial laparoscopic myomectomy. Am J Obstet Gynecol 1997; 177:1547.
31. Seinera P., Arisio R., Decko A. et al. Laparoscopic myomectomy: Indications, surgical technique and complications. Hum Reprod 1997; 12: 1927.
32. Dubuisson JB, Fauconnier A, Chapron C et al. Second look after laparoscopic myomectomy. Hum Reprod 1998; 13:2102.
33. Stringer NH, Strassner HT, Lawson L. et al. Pregnancy outcomes after laparoscopic myomectomy with ultrasonic energy and laparoscopic suturing of the endometrial cavity. J Am Assoc Gynecol Laparosc 2001; 8:129.
34. Dubuisson JB, Fauconnier A, Deffarges JV et al. Pregnancy outcome and deliveries following laparoscopic myomectomy. Hum Reprod, 2000; 15:869.
35. Landi S., Fiaccavento A., Zaccoletti R. et al. Pregnancy outcomes and deliveries after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc 2003; 10: 177.
Do complications after surgery lead to infertility?
If the situation develops favorably in the postoperative period (no inflammation, adhesions, hormonal imbalances), the woman manages to become pregnant after the body has fully recovered.
If complications arise during surgery or in the postoperative period, the function of the ovary on which the cyst was located may decrease slightly. For example, adhesions in the fallopian tube can impede the movement of the egg to the uterine cavity for fertilization. But even in this case, the woman’s reproductive function is preserved. If the cyst affects only one of the ovaries, and the second is healthy, then the answer to the question of whether it is possible to get pregnant is positive. As a paired organ, the ovaries work alternately: in one menstrual cycle, the follicle matures in the right, in the second - in the left. There are cycles without ovulation at all, when the ovaries “rest”.
If you cannot get pregnant after removing the cyst
Theoretically, removal of the cyst should increase the chances of conception, because. after removal of the foreign body, the ovary receives an impulse that stimulates the release of the egg. If, after the procedure, problems with conception persist, although no complications arose after the operation, then another reason for the decrease in fertility can be assumed.
The most common obstacles to getting pregnant are:
- “lazy” ovary syndrome, when ovulation occurs quite rarely;
- ovarian depletion;
- hormonal imbalance that makes ovulation difficult;
- hidden inflammatory process of the uterus or appendages.
To accurately identify the cause, a gynecologist must conduct a comprehensive examination, including a blood test for sex hormones (estrogen, progesterone, testosterone), and an ultrasound of the pelvic organs. Depending on the results of the examination, the doctor may prescribe hormonal therapy to stimulate ovulation, as well as physical treatment in case of endometriosis, tubal obstruction or other diseases of the female reproductive organs. It is better to give preference to natural and gentle methods. An excellent example is the peptide bioregulator Ovariamine. It has a focal effect on the ovaries, helping to restore the functional reserve of their cells, thereby participating in the preparation of the ovaries for conception.
Thus, it is possible to become pregnant after removal of a cyst; the main thing is to follow the recommendations of your doctor and use modern safe means to restore and maintain the physiological function of the ovaries.
Share: