The liver is a key organ in copper metabolism; copper-containing and copper transport proteins are synthesized in the hepatocyte. The liver is the main excretory organ for copper and it is obvious that liver disease causes metabolic disorders.
Disorders of copper metabolism are both genetic, which underlies Menkes-Wilson-Konovalov disease (MWD), and acquired in nature.
However, the number of literature data regarding changes in copper levels in chronic liver diseases is limited. The problem of impaired copper metabolism in patients with chronic liver diseases, and primarily cirrhosis, may be of significant scientific and practical interest. According to morphological studies [1], copper granules are detected in chronic active hepatitis in 17.2%, alcoholic fibrosis with lobular disorganization in 22%, non-biliary cirrhosis in 28%, drug-induced cholestasis in 15% of cases. Japanese researchers have identified a direct, reliable correlation between the copper content in liver tissue and the degree of fibrosis in chronic viral hepatitis C [2]. Accumulation of copper in liver tissue is detected in chronic liver diseases accompanied by cholestasis: primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC) [3]. According to E. Sumithran et al. [4], detection of copper granules in liver tissue helps to distinguish chronic biliary liver diseases from acute inflammatory diseases, including those accompanied by cholestasis, PBC from chronic active hepatitis, primary liver tumors from metastasis in the liver of tumors of other localizations. Serum copper and ceruloplasmin levels have been shown to be higher [5] in the development of hepatocellular carcinoma compared with liver cirrhosis and can be used as a marker of hepatocellular carcinoma, especially when the tumor cannot be detected by alpha-fetoprotein testing. One of the most common diseases associated with the accumulation of copper in the liver is alcoholic liver damage [6]. Copper levels correlate with liver fibrosis (based on morphometric data), according to F. Rodriguez-Moreno et al. [7], increased urinary copper excretion is associated with the severity of cirrhosis, a poor prognosis for patient survival, and may serve as an independent risk factor for mortality in alcoholic cirrhosis.
In this regard, the purpose of our work was to study the prevalence of copper metabolism disorders among patients with chronic liver diseases.
Materials and methods
The study included patients with chronic liver diseases who were treated in the 1st and 2nd hepatology departments of the Central Research Institute of Geology in the period from 2006 to 2008. A study of copper content in the blood and urine was carried out in 162 patients.
The distribution of patients according to the etiological factor that caused chronic liver disease is presented in the figure
.
Of the 162 patients included in the study, alcohol abuse was the cause of chronic liver disease in 67 (42%). 42% of them developed chronic alcoholic hepatitis (AH), and 58% developed alcoholic liver cirrhosis (ALC).
In 54 (33%) patients, chronic liver disease developed as a result of a viral infection (hepatitis C virus and/or hepatitis B virus). 61% of them were diagnosed with chronic viral hepatitis (CVH) and 39% with liver cirrhosis of viral etiology (CLV). In 21 (12%) patients, based on clinical, laboratory and instrumental examinations, PBC was established, and in 21 (13%) patients, BVD (hepatolenticular dystrophy) was established.
Clinical and gender characteristics of the examined group of patients are presented in Table. 1
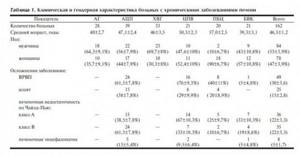
.
The average age of the examined patients was 46.5 years; in the examined subgroups, the average age of patients ranged from 39.3 years in the group of patients with BVC to 57 years in the group of patients with PBC; patients in this group were significantly older ( p
<0.05) than patients with hypertension and VCD. There was no significant difference in age between other subgroups.
Among the examined patients, the ratio of women and men was approximately equal, 47 and 53%, respectively. Women were significantly more common in the subgroup of patients with PBC ( p
<0.001), and in the subgroup of patients with chronic hepatitis, men were more common (
p
= 0.004). In the remaining subgroups of patients, no significant difference in the ratio of men and women was noted.
Complications of the underlying disease such as varicose veins, ascites, liver failure (HF), hepatic encephalopathy (HE) were mainly observed in patients with ADC and CVP, in patients with PBC and BVC they were less common, and in patients with viral hepatitis and hypertension no such complications were noted. VRVP occurred significantly more often in patients with ADC and CPV than in patients with PBC and BVC ( p
<0.05).
Ascites in patients with ADC was more common than in patients with CPV and PBC, but there was no significant difference. Also, patients with ADC more often, but not significantly, had a more severe degree of PN according to Child-Pugh than patients with CPV ( p
= 0.066).
In patients with BVC and PBC, PN according to Child-Pugh class B was significantly less common ( p
<0.05).
PE was diagnosed in 5% of the examined patients, most often in patients with ADC, but there was no significant difference with patients of other subgroups.
The examination plan includes an assessment of complaints, analysis of anamnesis data, objective status, laboratory and instrumental research methods. Adherence to the consumption of alcoholic beverages was studied using the :AGE questionnaire of the European Gastroenterological Association.
All patients underwent general clinical and laboratory tests. To verify the diagnosis, a survey and examination were carried out to identify major and minor liver signs (tremor, telangiectasia, hepato- and splenomegaly, dilatation of the saphenous veins of the abdomen, ascites, peripheral edema, etc.). A clinical blood test was performed (levels of hemoglobin, red blood cells, platelets, etc.). The functional state of the liver was assessed by the activity of alanine (ALAT) and aspartic (AST) aminotransferases, alkaline phosphatase (ALP), γ-glutamyl transpeptidase (GGTP), amylase, the content of bilirubin, cholesterol, glucose, total protein, protein fractions, creatinine, urea, prothrombin serum iron using an Olimpus automatic biochemical analyzer and reagents *.
Markers of hepatitis - HBsAg, H:VAb IgG, alpha-fetoprotein - were determined in the blood serum of all subjects.
To verify PBC, all patients were examined for the presence of antimitochondrial antibodies, and, if necessary, a liver biopsy was performed. To confirm the diagnosis of BVD, patients were examined by an ophthalmologist and a neurologist.
In order to clarify the degree of liver damage and the severity of portal hypertension, an ultrasound examination of the abdominal organs, a Doppler examination of the abdominal vessels using a Sony RTX 200 apparatus, and esophagogastroduodenoscopy (using a Fudjinon apparatus with assessment of the degree of varicose veins of the esophagus and stomach according to the Scherzinger classification) were performed. To assess the state of copper metabolism in patients with chronic liver diseases, the level of copper in the blood and daily urine and the level of ceruloplasmin in the blood were determined. To determine the concentration of copper in blood serum, commercial reagent kits were used; the study was carried out on an Olimpus automatic biochemical analyzer.
Statistical processing of the results was carried out using applied statistical programs Statistica 6.0 and Biostat. The significance level of error (probability of type I error) was considered reliable at α≤0.05, with sensitivity (probability of type II error) &Bgr;=0.8. Analysis of the difference in the results obtained was carried out for quantitative parameters using the t test, for multiple comparisons - the t test in the Newman-Keuls modification, the reliability of the difference in qualitative indicators was assessed using c2 or Fisher's test. To identify relationships, regression analysis was performed with calculation of the Pearson correlation coefficient.
ANALYSIS FOR MICROELEMENTS AND VITAMINS

Tests for the content of microelements and vitamins: indications for use, norms and causes of deviations
Vitamins and microelements are substances that provide all vital processes in the body without exception. Microelements are biologically significant inorganic elements contained in all living organisms in minimal quantities - 0.001% of body weight. These substances are often confused with vitamins. However, the latter belong to organic substances, although they are no less important for the body. Microelements and vitamins together are involved in all life support processes, and their deficiency or excessive excess leads to dangerous pathological changes. In order to timely identify a deficiency of certain biologically active substances, it is necessary to undergo a special test for vitamins and microelements.
You can often notice how the body, through the desire to consume certain foods, regulates the internal balance of the substances it needs. But, in order to find out more reliably about the internal state, you can do a blood test for vitamins and microelements.
MICROELEMENTS AND VITAMINS
Microelements are classified as inorganic substances, the content of which in the body is about 4% of the total mass of the human body.
Trace elements are divided into metals and non-metals (halogens). They enter the body with food, water, air, and some organs are provided with their own reserves of these biologically significant substances. Vitamins are low molecular weight organic substances. Many of these organic compounds are related to coenzymes or their precursors. The body obtains vitamins from food and the environment. The daily need for vitamins is small, but the supply of these substances should be regular. Because almost all the vitamins necessary for life support are not synthesized by the body, but come from outside.
Deficiency of vitamins and microelements is especially dangerous during the formation of the embryo and for the growing organism, because it leads to underdevelopment of organs and systems. For an adult, in whom all the structures of the body are formed, the deficiency of any vitamin and mineral is not so critical. But over time, the systematic absence of any substance leads to an imbalance in some vital processes. And if the lack of certain vitamins and microelements required by the body is not corrected in time, then over time this can lead to the development of pathologies.
Which vitamins are missing in the blood can be easily determined by conducting laboratory tests. In tests for vitamins and microelements analyzed by the attending physician, a list of values for each test substance will be indicated. Which will give a full-scale picture of the vitamin and mineral balance in the body
PROCEDURE FOR CONDUCTING RESEARCH
To determine the content of vitamins and minerals in the body, various studies are prescribed.
Whole blood or serum, hair, nails, and urine can be used as biomaterial A test for vitamins takes 1 business day, but a comprehensive analysis for microelements takes up to 6 business days. If the study involves taking blood, then you should come to the laboratory in the morning and on an empty stomach (after an 8-hour overnight fast). To submit hair and nails for examination, you must read special instructions (they are usually provided in the laboratory before the analysis), since the process of collecting them requires compliance with many nuances.
WHEN IS A BLOOD TEST REQUIRED?
A comprehensive blood test for vitamins and minerals should be taken in the following situations:
- During the period of planning, bearing and breastfeeding a child.
- A woman after completing the process of breastfeeding a child.
- Representatives of the fairer sex who are prone to heavy menstruation.
- Children in the active growth phase.
- Teenagers during puberty.
- Persons on strict diets.
- People employed in heavy and hazardous industries.
- To everyone who lives in an environmentally unfavorable area.
- For those who are susceptible to chronic pathologies.
- Patients after chemotherapy.
- Individuals exposed to constant stress.
- During the spring and winter months.
- To old people.
A blood test for microelements and vitamins requires certain preparation:
- You will need to come to the laboratory in advance to put your emotional (rest after the road) and physical (calm your pulse, blood pressure) in order.
- At least eight hours must have passed since your last meal.
- In the morning you are allowed to drink water, a little and always only clean water without any additives.
- For about a week, drinking any drinks containing alcohol is prohibited, this applies to both alcoholic and pharmaceutical products.
- On the day of taking a blood test for minerals and vitamins, it is advisable to refrain from smoking.
- To take a blood test correctly and get a reliable result, you cannot combine days of visiting the laboratory and physiotherapeutic (hardware) procedures.
- The laboratory technician or attending physician must be notified if drug therapy is being administered. Most likely, you will need to stop taking medications while blood is drawn to study the levels of vitamins and minerals in the body.
It is possible to obtain distorted examination results if a person is in a state of strong emotional distress. Intense physical activity also does not have the most favorable effect on blood composition. This applies not only to people involved in heavy physical labor, but also to athletes.
INTERPRETATION OF THE RESULTS OBTAINED
Modern medicine reliably knows a list consisting of 13 vitamins (water- and fat-soluble) and 16 microelements.
Of the microelements, nine substances have essential status. Vital microelements include: I (iodine), Fe (iron), Mn (manganese), Co (cobalt), Mo (molybdenum), Cr (chromium), Se (selenium), Zn (zinc), Cu (copper) . The norm of each substance must be present in the blood at all times. When normal levels of vitamins or minerals fail to decrease or increase, pathologies begin to develop in those organs and systems for which certain useful particles are responsible. Pathologies due to a lack of vitamins and microelements:
- Dysbacteriosis;
- Tendency to anemia, various types of anemia;
- Weakness of the immune system;
- Excess weight;
- Development of diabetes;
- Loss of hair on the head;
- Skin diseases;
- Digestive disorder;
- Pathologies of bones and joints;
- Cardiovascular diseases;
- Disorders of the nervous system (central and peripheral);
- Slow development in children;
- Weakening of sexual and reproductive function.
This is only a partial list of pathologies that arise as a result of a deficiency of nutrients. The clinical picture of vitamin and mineral deficiency is especially pronounced if a person has a tendency to bleed, as well as after chemotherapy. This procedure, aimed at destroying malignant cells, causes enormous damage to the entire body. Therefore, after chemotherapy, to restore the balance of vitamins and microelements, you will need to take special complexes and, in addition, fruits and vegetables. But not only for recovery after chemotherapy, increased intake of mineral and vitamin complexes is recommended. A diet, as well as taking medications with a certain content of vitamins and microelements, depending on the specific need for a particular substance, is indicated in many cases.
Often, doctors and patients themselves do not associate diseases with a lack of any elements, but such a problem is quite easy to eliminate by simply changing the diet or prescribing appropriate vitamin and mineral complexes. However, before you run to the pharmacy, you should take a test for vitamins and microelements and take the results to your doctor, who can expertly select certain vitamin and mineral supplements or prescribe the right diet.
MICROELEMENTS IN SERUM AND WHOLE BLOOD: SCREENING
Cobalt is a component of vitamin B12, necessary for DNA synthesis, hematopoietic processes, and the functioning of the nervous system. Cobalt deficiency can lead to such serious diseases as pernicious anemia, funicular myelosis, megaloblastic anemia. Determination of cobalt plays an important role in differentiating B12-deficiency anemia from folate deficiency. Excess cobalt, on the contrary, has a toxic effect on the body and usually occurs when working in hazardous industries. The normal level of cobalt in blood serum is 0.00045–0.001 mcg/ml.
Copper is a metal whose daily requirement is 2 mg per day. Copper metabolism occurs mainly in the liver. The element is a structural component of many enzymes and important proteins. Lack of copper leads to impaired pigmentation of hair and skin, anemia, osteoporosis, damage to bones and joints. With an excess of copper, poisoning occurs, accompanied by nausea, vomiting, and loose stools.
The norm of the presence of copper in blood serum:
- men 0.75–1.5 mcg/ml;
- women 0.85–1.8 mcg/ml.
Molybdenum - this microelement is part of some metalloenzymes that participate in metabolic processes. Molybdenum enters the body with food - it is found in nuts, legumes and grains. In the body it is concentrated mainly in the bones, kidneys and liver. Molybdenum deficiency in medical practice has been described only under conditions of prolonged artificial parenteral nutrition. Molybdenum poisoning has not been described. Reference blood levels are 0.0004–0.0015 mcg/ml.
Selenium is an element that is especially important for thyroid function (thyroid function). It is part of iodothyronine deiodinase, an enzyme that converts the inactive hormone thyroxine (T4) into active 3-iodothyronine (T3). In addition, selenium is necessary for the normal functioning of the immune, reproductive, cardiovascular and nervous systems. Selenium is a natural antioxidant that is used in cosmetics. Selenium deficiency can lead to mental disorders, increase the virulence of viruses and reduce the body's defense against certain types of cancer. In excess quantities, selenium is toxic. Excess may be associated with work in hazardous work and voluntary use of the drug. The normal level in blood serum is 0.07–0.12 mcg/ml.
Zinc is the second most abundant element in the body after iron. It is part of more than 300 metalloenzymes and plays a key role in the synthesis of proteins and nucleic acids. In food, zinc is mainly associated with proteins, the most accessible is considered to be in red meat and fish. Zinc deficiency is a consequence of a diet low in animal proteins. In addition, iron supplementation may reduce zinc absorption. The symptoms of zinc deficiency are not specific, so it is diagnosed primarily through micronutrient testing. The normal level of zinc in the blood is 0.75–1.50 mcg/ml.
Manganese is an element that is involved in the formation of connective tissue and bones. Associated with growth mechanisms, reproductive functions, carbohydrate and lipid metabolism. As a rule, manganese enters the body in small quantities, and its deficiency can lead to demineralization of bones. Low levels of manganese are characteristic of diseases such as multiple sclerosis, vitiligo, diabetes mellitus, etc. Excess manganese is manifested by neurotic syndromes, increased fatigue, rickets, and hypothyroidism. Chronic manganese poisoning is typical for some professions - for example, foundry workers, welders, miners, and workers in certain specific industries. Reference values in the analysis (whole blood) for microelements are 0.007–0.015 μg/ml.
On a note
Separately in the list of microelements are microelements such as iodine and iron, the properties and importance of which most of our compatriots know firsthand, and therefore we will not dwell on them in detail. Determination of serum iron levels is included in an advanced blood chemistry test along with calcium, potassium, sodium and chlorine. Hair, urine and nails are used to determine iodine content.
VITAMINS IN BLOOD SERUM

Most people know much more about the benefits of vitamins than microelements. Vitamins are designated by letters of the Latin alphabet. Some of them are independent substances, and some represent a whole complex of substances (B vitamins). At the moment, vitamins A, B, C, D and E are considered the most studied. Vitamins C and B are water-soluble, vitamins A, D, E are called lipovitamins, that is, they are fat-soluble.
Chronic deficiency of these vitamins leads to serious consequences. For example, the daily requirement for vitamin A is 900 mcg for adults, and its deficiency leads to the development of night blindness. At the same time, an excess of this biologically active substance is dangerous and can disrupt the development of the fetus and cause intoxication of the body. A lack of B vitamins is associated with many skin diseases, mental disorders, metabolic disorders, weakened vision and memory, hair loss, joint pain and liver dysfunction. Vitamin C deficiency causes scurvy, bleeding gums and nosebleeds. Lack of vitamin D leads to the development of rickets and osteomalacia (softening of the bones). Vitamin E deficiency is a cause of neuromuscular disorders, myopathy and anemia.
The most common vitamin tests look at vitamin D, B12 (cyanocobalamin) and B9 (folic acid). Blood serum is used for the study. Content standards:
- D - 25–80 ng/ml;
- B12 - 187–883 ng/ml;
- B9 - 3.1–20.5 ng/ml.
So, micronutrient tests can be comprehensive or performed as separate studies. A comprehensive analysis is more indicative and is recommended for regular use in order to prevent deficiency of a certain set of microelements and vitamins. Tests for individual elements are prescribed by a doctor to clarify the causes of certain diseases. Remember that common symptoms such as fatigue, drowsiness, depression, sleep disturbances, brittle hair and nails may be due to a lack of vitamins or minerals.
Results and discussion
The average blood copper level was 18.1±0.52 µmol/L. The average value was 0.41±0.01 µmol/day, the median and value of copper content in urine at the 16th and 84th percentiles was 0.38 (0.29-0.47) µmol/day. The average content of ceruloplasmin in the blood of patients in the examined group was 47.3±1.44 mg/dl, the median and values of ceruloplasmin at the 16th and 84th percentiles were 48.2 (25-65) mg/dl.
The levels of copper in the blood and urine and ceruloplasmin in the blood did not differ significantly between men and women. There was also no significant correlation of these indicators with the age of the patients. Consequently, neither the age nor the gender of the patients affected the levels of copper and ceruloplasmin. The values of copper in the blood and urine and ceruloplasmin in the blood depended on the etiology of the disease, which was confirmed by the values of these indicators depending on the etiological cause of the disease ( Table 2

).
The subgroup of patients with VCD differed significantly and significantly from all groups of patients. This subgroup showed the largest decrease in copper levels in the blood with the lowest ceruloplasmin content and a more than 2-fold increase in urinary copper excretion compared to other subgroups. Such laboratory indicators of copper metabolism generally correspond to the state of copper metabolism in this disease. Only in this subgroup of patients were changes in the average concentration of copper in the blood and urine and the level of ceruloplasmin, different from normal values, noted.
The copper level in the blood of the remaining patients ranged from 17.0 µmol/L in the group of patients with hypertension to 24.5 µmol/L in the group of patients with ADC. The level of copper in the blood in patients with ADC was significantly higher than in patients of other subgroups, with the exception of patients with CPV. In patients with CPV, the level of copper in the blood was significantly higher than in patients with chronic hepatitis of viral or alcoholic etiology and patients with PBC.
The copper content in urine did not change significantly depending on the etiology, with the exception of patients with BVC.
The highest concentration of ceruloplasmin in the blood was observed in patients with PBC; it was significantly higher than the concentration of ceruloplasmin in patients of other subgroups. The lowest concentration of ceruloplasmin, as already noted, was characteristic of patients with BVC. The content of ceruloplasmin in the blood in the remaining subgroups of patients did not differ significantly.
Thus, the differences we identified in the content of the studied parameters in patients with various nosological forms of liver disease, the absence of a normal distribution of copper in the urine and ceruloplasmin in the blood suggest the presence of multidirectional changes in copper metabolism in the examined group of patients. In this regard, an analysis of the state of copper metabolism in patients was carried out in subgroups depending on the etiological factor that caused chronic liver disease.
The average copper level in patients with chronic liver diseases (except for BVD) was 19.1±0.45 µmol/l and was almost 3 times higher than in patients with VD ( p
=0.0007). The average values of copper in the blood were the highest in patients with cirrhosis of the liver and did not depend on the etiology; the difference in values was significant. Blood copper levels above normal physiological values were observed in 10 (14.9%) patients with ADC, 5 (9.3%) patients with liver damage of viral etiology and 2 (10%) patients with PBC, a significant difference in incidence There was no hypercuprumemia between groups.
An increase in the level of copper in the blood plasma was also noted by other researchers: in chronic hepatitis [8, 9], in acute hepatitis [10], in patients with PBC [11], and PSC [3]. According to P. Berresford [6], alcoholic cirrhosis is the most typical common disease associated with the accumulation of copper in the liver. According to their data, copper accumulation was detected in the liver of patients with liver cirrhosis and was not detected in patients with alcoholic disease without liver damage.
F. Rodriguez-Moreno et al. [7] also found that alcoholic liver damage affects the content of iron, zinc, copper and manganese in the liver.
A decrease in copper levels in the blood below normal was observed in only 1 patient with hypertension. In the group of patients with BVC, only 2 patients had normal copper content; in other cases, in 90% of patients it was below normal. Thus, it was the decrease in the level of copper in the blood that was one of the differences in the laboratory picture of the diseases we studied in comparison with the indicators of patients with BVC. The sensitivity and specificity of this indicator for diagnosing BVD were 95 and 24%, respectively.
The next indicator studied was urinary copper levels. In no patient did the daily excretion of copper in urine go beyond the normal range, with the exception of patients with BVC. The values were higher than normal in 13 (62%) patients with BVC. The average copper level in urine in patients with chronic liver diseases was 0.37±0.007 µmol/day and was significantly lower than in patients with CD (p=0.026).
In patients with ADC ( r
=-0.61;
p
=0.02) and BVC (
r
=-0.57;
p
=0.007), an inverse correlation was noted between copper levels in the blood and urine. This trend indicated that for patients with BVC, a decrease in copper content in the blood is not associated with an increase in copper excretion in the urine. In patients with ADC, hypercuprumemia is not accompanied by an increase in copper excretion in the urine.
In patients with viral cirrhosis ( r
=0.66;
p
=0.001), hypertension (
r
=0.41;
p
=0.02), the level of copper in the blood is directly related to the level of copper in the urine.
In patients with PBC, the same trend was noted, but with an unreliable significance of the correlation coefficient ( r
= 0.41;
p
= 0.075).
The diagnostic value of increased urinary copper for the diagnosis of BVC was also analyzed. The specificity and sensitivity of excess daily urinary copper excretion are 61 and 50%, respectively.
One of the most important components of copper metabolism is its transport protein, ceruloplasmin. Ceruloplasmin is also an acute phase protein and increases during inflammatory processes of various etiologies. In patients with chronic liver diseases, the average level of ceruloplasmin ranged from 44.9 mg/dl in patients with hypertension to 65.5 mg/dl in patients with PBC, and was significantly lower than in patients with BVC - 21.2 mg/dl. Only in 2 (10%) patients with this disease the level of ceruloplasmin reached normal. An increase in ceruloplasmin levels above normal was observed in 10 patients with alcoholic liver damage, 9 patients with viral liver damage, and 14 patients with PBC. Thus, an increase in ceruloplasmin levels was significantly more often observed in patients with PBC than in patients with alcoholic liver damage (χ2=8.4; p
=0.004) and patients with viral liver damage (χ2=4.32;
p
=0.032).
There was a direct and significant correlation between the levels of ceruloplasmin and copper in the blood only in patients with liver cirrhosis of alcoholic ( r
=0.53;
p
=0.01) and viral (
r
=0.71;
p
=0.001) etiologies. In patients with PBC, there was no relationship between ceruloplasmin and copper, so, most likely, the increase in ceruloplasmin in patients with PBC is associated with the severity of inflammatory changes, and not with disturbances in copper metabolism.
One of the indicators of a copper metabolism disorder is the presence of direct copper in the blood. Direct copper is an unfavorable factor, as it can cause extrahepatic tissue damage (nervous system, kidneys, heart, joints), and with the rapid release of copper, enzymatic penic hemolysis occurs. This is observed, for example, in the fulminant form of the disease.
Direct copper in the blood was noted significantly more often in case of VCD - 19 patients than in case of viral liver damage - 6 patients (χ2 = 39.4; p
<0.001) and alcoholic liver damage - 25 patients (χ2=16.1;
p
<0.001). The diagnostic value of detecting direct copper for diagnosing BVC was calculated. The specificity and sensitivity for detection of direct copper were 27 and 17%, respectively.
To increase the diagnostic value of this test, additional conditions were introduced: the diagnostic value of direct copper was calculated only in patients with a decrease in copper levels in the blood. In the patients with chronic liver diseases we examined, not a single patient was noted with a reduced level of copper in the blood and the presence of direct copper. This combination was observed only in 19 patients with BVC. Thus, the sensitivity and specificity for detecting direct copper in hypocuprumemia is 100%.
SPECTRAL ANALYSIS OF HAIR FOR MICROELEMENTS
Hair provides very reliable information about the state of the body - being a storage material, it can retain information about substances for a long time. Also, this type of material is quite resistant to the influence of random factors.

Currently, a new type of diagnostics of the state of the body has appeared in medical science - a mineralogram (or spectral analysis of hair for microelements ). It allows you to identify the ratio of about 40 substances necessary for health, as well as determine the degree of their excess or deficiency in order to select the most suitable method for correcting the imbalance. Hair is analyzed for microelements using the patented method of A. V. Skalny.
General comprehensive assessment of the elemental composition according to Profile ME10:
conclusions
In patients with chronic liver diseases, the main disorder of copper metabolism, in contrast to BVC, is an increase in the level of copper in the blood. It occurs in 9.3% of patients with viral liver disease, 10% of patients with PBC and 14.9% of patients with alcoholic liver disease.
An increase in copper content in the blood in patients with chronic liver diseases, unlike patients with BVC, is not accompanied by an increase in daily copper excretion in urine above normal values.
The greatest diagnostic significance for diagnosing BVD is the detection of direct copper when the level of copper in the blood decreases below normal (hypocuprumemia).