Infectious mononucleosis
is an infectious disease that also goes by several other names: Filatov’s disease, Epstein-Barr virus (EBV), monocytic tonsillitis, benign lymphoblastosis. It is characterized by a feverish state, damage to the pharynx, lymph nodes, spleen and liver, and changes the composition of the blood.
The causative agent of mononucleosis is the DNA genomic Epstein-Barr virus of the herpesvirus family (Herpesviridae). Divided into two types A and B, which are similar in symptoms and course of the disease.
Herpesvirus is widespread - 50% of children are carriers, among adults the incidence reaches 90%. In the vast majority of cases, the person is a carrier. No symptoms appear. Such a person is called seropositive or seropositive.
Sometimes the disease causes serious complications: airway obstruction, closed damage to the soft tissue of the spleen and neurological syndromes. The main diagnostic method is serological analysis. Therapy is symptomatic and supportive. Once infected, a person becomes a carrier of the virus for life.
tests
Transmission routes
The virus does not live outside the human body. Kills at high temperatures and from disinfectants. Transmitted by biological fluids and airborne droplets through close contact of a healthy and seropositive person. Infection occurs in both acute and chronic phases.
The most common method of transmission is a kiss, the rarest is through a blood transfusion. You can become infected by sharing utensils, clothing, bed linen and towels. Outbreaks of the disease occur in crowded places: dormitories, small families, child care institutions. Most often, herpesvirus is detected in social groups with low incomes, due to cramped living conditions.
Role in the body
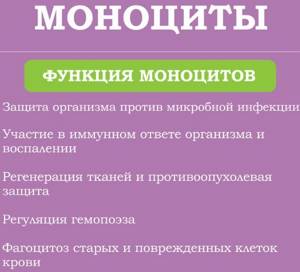
Mononuclear cells are divided into monocytes and lymphocytes. The first cells absorb foreign microorganisms and bacteria, and also spread information throughout the human body that an infection has invaded. Lymphocytes are responsible for producing antibodies that are necessary to fight pathogenic agents.
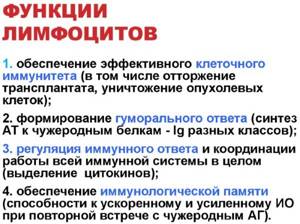
It is thanks to B-lymphocytes that strong immunity to various infectious diseases is developed. Immune memory makes it easier to endure re-infection without complications. In most cases, mononuclear cells in the blood indicate the development of a serious pathology.
Symptoms of mononucleosis
In young children under 5 years of age, primary EBV infection is usually asymptomatic. Symptoms of infectious mononucleosis most often develop in adolescents, and slightly less often in adults. The average incubation period is 40 days. At this time, the patient experiences increased fatigue.

The disease occurs in 3 phases:
1. Fever - the temperature rises during the day, reaching its peak in the evening. Reaches +40 C, but can be higher, subsides by morning.
2. Pharyngitis (inflammation of the pharynx and tonsils) - is severe, with severe pain. The mucous membranes turn red, swell, and exudate may form.
3. Adenopathy - generalized enlargement of lymph nodes. Changes can be noticed visually and by palpation of the posterior and anterior cervical lymph nodes, submandibular, axillary and inguinal. The lesion is symmetrical and can be observed on any group of nodes. In some cases, adenopathy may be the only sign of infection.
Depending on the individual characteristics of the body and the presence of other diseases, mononucleosis in some people can cause the following symptoms:
- Splenomegaly is an enlarged spleen, found in 50% of cases.
- Hepatomegaly - an increase in the size of the liver, pain when tapped.
Other symptoms include jaundice, swelling around the eyes, and broken capillaries (petechial rash).
Symptoms
Diagnostic measures will help to accurately determine abnormalities associated with mononuclear cells in the blood.
However, there are clinical signs that will allow you to suspect problems and promptly go to the hospital:
- a large amount of sweat is released;
- the person complains of general weakness and weakness;
- joint and muscle pain occurs;
- sudden fever appears;
- decreased ability to work;
- the skin becomes very pale;
- The cervical lymph nodes become enlarged and pain appears during palpation;
- a person breathes more often through his mouth;
- the voice becomes hoarse;
- shortness of breath appears;
- appetite worsens;
- sleep is disturbed, daytime sleepiness appears;
- mucous membranes and sclera turn yellow;
- hepatosplenomegaly develops.

In most cases, changes in the level of mononuclear cells in the blood occur as a result of the development of a specific disease. Therefore, the patient will also have characteristic signs of concomitant pathology.
Complications
During primary infection, the Epstein-Barry virus can be asymptomatic in the body, and in some cases cause serious consequences. First of all, these are respiratory complications.
- Obstruction of the upper respiratory tract - lymph nodes can increase to such a size that breathing will be difficult.
- Pulmonary infiltrates are the replacement of an area of normal airiness of the lung with denser enlarged tissues. More often observed in young children.

Complications of mononucleosis can affect individual organs:
- Liver. In 95% of patients, the level of aminotransferase increases 2-3 times. The skin may acquire a slight icteric tint. The liver will be enlarged and painful on percussion.
- Spleen. With mononucleosis, the spleen and capsules increase significantly in size, which leads to ruptures. Maximum swelling is observed 10–21 days after infection. On average, the complication is observed in half of the patients. The rupture may be painful or may be painless with hypotension (low blood pressure).
Hematological complications are also noted, which, as a rule, do not require medical intervention and are self-limiting. This includes:
- Granulocytopenia is a decrease in the content of granulocytes in the peripheral blood.
- Thrombocytopenia - decreased platelet count, increased risk of bleeding.
- Hemolytic anemia - premature breakdown of red blood cells
Similar symptoms are observed in 50% of patients. In rare cases, hematological complications are severe and can lead to bacterial infections.
The nervous system also suffers from EBV. In extremely rare cases, encephalitis, Guillain-Barre syndrome, cranial nerve palsies, meningitis, and myelitis may develop against the background of infectious mononucleosis.
Decoding the results. How are mononuclear cells designated?
Only a pediatrician, therapist or hematologist can fully examine the examination results. The specialist, guided by the data obtained, will make an accurate diagnosis.
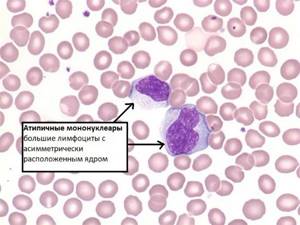
A general blood test shows:
- increase in atypical cells by 10%;
- increase in monocytes by 40%;
- lymphocytes increased by 10%;
- the total number of lymphocytes and monocytes is 80-90% when compared with the total number of leukocytes.
White blood cells and erythrocyte sedimentation rate (ESR) will be slightly increased. The same applies to neutrophils (by 6%).
Diagnostics
- Heterophilic antibody assay.
- Serological test for Epstein-Barr virus.
To carry out these tests, it is necessary to assume the presence of infectious mononucleosis virus based on typical symptoms. Such symptoms include enlarged lymph nodes in the back of the neck or generalized adenopathy in combination with an enlarged liver and spleen, exudative pharyngitis and high fever.
You should also pay attention to diseases with similar symptoms and exclude them.
Differential diagnosis
When diagnosing, it is necessary to make sure that the patient has a herpes virus, since there are several infections similar to EBV. Among them:
- Primary HIV infection. It can be excluded by conducting tests for the quantitative determination of HIV RNA in blood plasma and a combined enzyme-linked immunosorbent assay for antibodies and p24 antigen.
- Primary HIV infection has symptoms similar to EBV. All patients at risk must undergo an HIV test without fail.
- Cytomegalovirus. Similar to EBV in everything except pharyngitis. To exclude this disease, serological testing, antigen testing, or CMV DNA testing is necessary.
- Toxoplasmosis. A parasitic disease, which, like cytomegalovirus, differs from mononucleosis in the absence of pharyngitis. For differentiation, he performs serum serology and an analysis for the level of IgG antibodies.
In practice, there are cases of simultaneous infection with several types of viruses that are in the active phase in the body. Differentiation is also carried out when treatment is ineffective, the course of the disease is prolonged, and the results are insufficient for remission.
Laboratory methods for diagnosing mononucleosis
The main criterion for making a diagnosis is a serological test for EBV. Atypical lymphocytes may be present in influenza, hepatitis B, HIV, cytomegalovirus and other viral diseases. But, only with primary mononucleosis they are produced in very large quantities.

Serological analysis is confirmed by a test for specific (heterophilic) antibodies to EBV. The most productive research is when working with biological materials from adolescents and adults. In children under 5 years of age, it shows a positive result only in 50% of cases.
It is important to know!
In HIV-infected people, testing for heterophile antibodies may be false positive. It is recommended to conduct the study twice with a break of 7 - 10 days.
The presence of IgG antibodies to EBV VCA indicates primary EBV infection. They can be detected from the first days of infection for three months. Antibodies to EBV-IgG are developed later, approximately 2 months after the onset of the disease. They remain in the blood throughout a person’s life.
Instrumental diagnostics
To make a diagnosis, assess the severity, and monitor therapy, the following types of instrumental diagnostics are used:
- ultrasound examination of the peritoneal organs;
- electrocardiogram;
- chest x-ray;
- echocardiography;
- neurosonography;
- electroencephalography;
- X-ray of the paranasal sinuses.
An instrumental examination of the patient allows, by determining the size of the liver, spleen and lymph nodes, to assess the severity of the disease: mild, moderate, severe. When diagnosing “infectious mononucleosis,” they indicate the specifics of the course of the disease: clinical, nosological form, severity, duration. The presence of complications and concomitant diseases is entered in a separate line.
Mononuclear cell norms in adults and children
Mononuclear cells in a general blood test, namely their level depends on the person’s age:

Mononuclear cells in the general blood test (leukocyte formula) are normal
| Age | Monocyte count (%) | Lymphocyte count (%) |
| 0-5 years | 4-10 | 16-32 |
| 5-10 years | 4-7 | 40-60 |
| 10-15 years | 3-6 | 35-50 |
| 15-20 years | 3-7 | 30-45 |
| 20-50 years | 3-7 | 30-45 |
| over 50 years old | 4-8 | 35-50 |
Serious deviations from established norms indicate the development of a certain disease. Additional comprehensive diagnostics will help clarify the diagnosis.
Treatment of infectious mononucleosis
- Maintenance therapy.
- Corticosteroids for severe disease.
Treatment of infectious mononucleosis is aimed at stopping palogolic processes, preventing their development in the future, preventing complications, residual effects and the chronic course of the disease.
First of all, the patient must be provided with rest. During the period of enlarged spleen, physical activity and sports are prohibited. Heavy lifting should be avoided to reduce the risk of splenic rupture. To reduce symptoms and speed up recovery, drug and non-drug treatment methods are used.
Drugs for etiotropic, symptomatic therapy and immunocorrection are indicated:
- interferons;
- immunoglobulins;
- nucleosides and nucleotides, except reverse transcriptase inhibitors;
- derivatives of propionic and acetic acid;
- triazole derivatives;
- adrenomimetics;
- antibiotics;
- macrolides;
- glucocorticoids;
- solutions affecting water-electrolyte balance for detoxification;
- mucolytic drugs and others depending on the symptoms.
Antibiotics are prescribed only for viral-bacterial infections confirmed by microbiological diagnostics. If complications occur, corticosteroids may also be prescribed. It is believed that they help to get rid of fever faster and reduce the manifestation of pharyngitis. They are useful for complications such as threatened airway obstruction, hemolytic anemia, and thrombocytopenia.
The most effective methods of non-drug treatment include physical therapy, sanitation of the nasal passages, and frequent ventilation of the room. Depending on the extent of the disease, treatment can be carried out on an outpatient basis or in a hospital.
Indications for examination
The patient comes to the hospital with certain complaints and existing symptoms, taking into account which the pediatrician or therapist prescribes an examination.
There are the following indications for diagnosis:
- infectious and viral diseases;
- food or medication poisoning;
- blood disease;
- miliary tuberculosis;
- applastic anemia;
- liver failure;
- treatment with cytostatics;
- pyogenic infections;
- state of shock.
During pregnancy, the level of mononuclear cells may change. The same applies to vaccinations, tumors, autoimmune pathologies, and HIV infection. A blood test for mononuclear cells is also prescribed to patients before surgery or before vaccination. Research will help ensure that there is no hidden infection and monitor the treatment being carried out.
Prognosis and prevention
In most healthy people, the acute phase of infectious mononucleosis goes away on its own. However, a person remains a carrier of the virus forever. Severe course and complications are observed in 10 - 20% of cases, depending on the age group. The presence of chronic diseases and immunodeficiency conditions increases the risk of severe disease. Mortality is low, less than 1%, and is caused by complications that develop due to infection: airway obstruction, encephalitis, splenic rupture.
The duration of the acute phase of the disease is about 2 weeks. After this period, if there are no symptoms, the patient can return to school or work. Indications for discharge include: normalization of temperature, absence of signs of intoxication and inflammation in the nasopharynx, normalization of the size of the lymph nodes, liver and spleen. However, it is necessary to continue a gentle sleep-wake schedule and avoid increased mental and physical stress. High fatigue will persist for several more weeks, and in some patients for many months.
After mononucleosis, the body's sensitivity to respiratory diseases and the herpes virus increases. Many people note the onset of frequent skin lesions on the upper or lower lip after recovery from EBV.
Preparation for blood and urine tests
The procedure for collecting biological material requires compliance with the minimum rules to obtain the most accurate results:
- On the day of the examination, the patient is not recommended to eat.
- Before the analysis, it is necessary to completely eliminate physical activity.
- The day before blood sampling, it is recommended to refrain from drinking alcohol, fatty and fried foods.
- A week before taking the study material, you must stop taking medications.
- In the morning before the examination, it is not recommended to brush your teeth; it is enough to rinse your mouth.
- Before starting urine collection, hygiene procedures must be carried out.
Immediately before the blood test, patients should rest well and relax for 15-20 minutes.
Advantages of the laboratories of JSC "SZDCM"
- Our own laboratory and advanced equipment guarantee fast and accurate results.
- Qualified and friendly staff - anonymity, comfortable stay, no queues.
- Convenient location of the terminals - easy to reach not only by car, but also by public transport.
- Several ways to receive results - in person, via the email specified during registration.
You can get tested for infectious mononucleosis in St. Petersburg, Leningrad region, Veliky Novgorod, Staraya Russa, Okulovka, Kaliningrad and Pskov.





