In the overwhelming majority of cases of ARVI, including coronavirus, antibiotics are not needed, according to the Russian Ministry of Health. Bacterial infection can be determined by several blood test parameters.
Altai and Russian doctors have recently been talking a lot about the dangers of prescribing antibiotics for signs of acute respiratory viral infection from the first days of illness, especially on their own. In the vast majority of cases, such treatment is unjustified, since viral pneumonitis and bacterial pneumonia are different diseases. And yet there are situations when bacteria join viruses. The most obvious sign is the appearance of purulent sputum. But the best way to tell is blood tests.
Detailed description of the study
Many infectious and non-infectious diseases can be suspected even before the appearance of pronounced clinical symptoms. Then diseases can be prevented by taking preventive measures, or identified and started therapy: the sooner the better. A general blood test makes it possible to assess the patient’s health status, therefore it is used as a screening diagnostic method. This study is important for monitoring the progress of pregnancy, when the doctor monitors the well-being of two organisms, and not one.
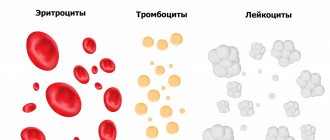
The analysis includes three studies:
- Complete blood count (CBC);
- Determination of erythrocyte sedimentation rate (ESR);
- Leukocyte formula.
Full list of hematological parameters determined during the study:
- Red blood cell count;
- Leukocyte count;
- Platelet count;
- Amount of hemoglobin;
- Hematocrit;
- Average hemoglobin content in a red blood cell;
- Color index;
- Average erythrocyte volume;
- Average hemoglobin concentration in a red blood cell;
- Leukocyte formula, types of leukocytes with counting;
- Erythrocyte sedimentation rate.
These indicators make it possible to determine the presence of inflammation or infection, anemia, and also detect some other pathological processes. A diagnosis cannot be made from this test alone, but the findings are a great starting point to confirm that a person is healthy. Otherwise, for further diagnostics.
Indicators: norms and deviations
Most laboratories that test blood for a fee indicate reference values in the results - the “plug” of the norm. These are the ones you should focus on first.
All information presented below is taken from open sources and is primarily for informational purposes only. Only a doctor can interpret test results and prescribe medications for treatment.
C-reactive protein
C-reactive protein (CRP) is an acute phase protein of inflammation. It increases within 6 hours after the onset of the disease and increases 10-100 times within 24-48 hours.
May 28, 8:00
Is it worth testing for antibodies to coronavirus and where to do it in Barnaul?
Test for immunity to coronavirus: why is it needed, how much does it cost, how is it carried out and the dangers of asymptomatic disease
This indicator is the main laboratory marker of the activity of the process in the lungs. Its increase is directly dependent on the extent of damage to the lung tissue and is the basis for starting anti-inflammatory therapy, according to the Russian Ministry of Health.
Normally, the C-reactive protein (CRP) level should not exceed 1 mg/l. If the level of CRP exceeds 10 mg/l, this may be evidence of an ongoing infectious inflammatory disease, according to specialists from the Helix laboratory.
High levels of CRP (more than 100 mg/l) are observed with bacterial infection. With a mild viral infection, the level of CRP, as a rule, does not exceed 20 mg/l.
The clinical recommendations of the Ministry of Health for the treatment of COVID-19 indicate that exceeding 30 mg/l indicates a moderate to severe course of the viral infection. When CRP is above 60 mg/L, patients in hospitals are prescribed immunosuppressants to combat cytokine storm (excessive inflammatory response of the immune system).
CRP levels may also increase due to pregnancy, intense physical activity, oral contraceptives, and hormone replacement therapy. CRP may decrease due to the use of nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, statins, and beta blockers.
Leukocytes, neutrophils and ESR
Most patients with COVID-19, according to the Russian Ministry of Health, have a normal number of leukocytes. A third have leukopenia – a decrease in white blood cells (below 4*10 to the 9th degree/l). Severe leukopenia (below 1*10 in the 9th degree/l) is characteristic of a cytokine storm and requires hospitalization.
October 22, 6:04
To the pharmacy 250 km away. How Barnaul residents bought up vital medicines
Patients with chronic diseases, bacterial infections and pregnant women are forced to reserve emerging drugs
Leukocytosis (increased white blood cells) is characteristic of a bacterial infection, not a viral one. The Ministry of Health of the Russian Federation considers an indicator above 10 * 10 to the 9th power / l in combination with other signs in adults to be a basis for considering the issue of taking antibiotics. At the same time, in clinical recommendations for the treatment of acute respiratory infections in children edited by Baranov, leukocytosis is called an indicator of over 15 * 10 to the 9th degree / l.
According to the Invitro laboratory, in adults, neutrophilia (a significant increase characteristic of a bacterial infection) is considered to be more than 7.5 * 10 to the 9th power / l. Neutropenia (significant decrease) is considered to be a decrease in the absolute amount below 1.8 thousand per microliter. In recommendations for the treatment of acute respiratory infections in children, an increase in neutrophils is considered to be over 10 thousand per microliter.
The Ministry of Health of the Russian Federation does not provide exact data on the level of ESR, so it should be assessed based on laboratory reference values.
Procalcitonin
Autoimmune diseases, chronic inflammatory processes, viral infections and mild local bacterial infections rarely lead to an increase in procalcitonin of more than 0.5 ng/ml.
November 03, 6:04
Encephalitis and the tongue is larger than the mouth: how Altai children cope with Covid
In the Altai Territory, approximately 1% of children suffer from coronavirus severely, the rest are mildly ill or generally asymptomatic
Unlike other tests, the assessment of this indicator is quite expensive, so it is rarely taken during outpatient treatment. The Ministry of Health of the Russian Federation recommends taking blood for procalcitonin when patients with COVID-19 are admitted to hospital for early assessment of the risk of death and to exclude a bacterial infection.
According to the Invitro laboratory, procalcitonin levels below 0.25 ng/ml may be a reason to refrain from using antibiotics or stop taking them.
Important Notes
Material for research
children under 7 years of age: venous blood/capillary blood (for special indications) children over 7 years of age and adults: venous blood Taking capillary blood for research is carried out only for children under 7 years of age (for special indications)! According to GOST R 53079.4-2008, indications for taking capillary blood are possible: in newborns, in patients with very small or hard-to-reach veins, with large-area burns, and severe obesity of the patient.
How to prepare for tests?
For maximum accuracy of results, we recommend donating blood in the morning, on an empty stomach. You can take the test during the day, but at least 3 hours must pass after your last meal. It is allowed to drink water without gas. It is recommended to limit the consumption of fatty and spicy foods and alcohol during the day.
As for how to prepare for urine tests, it is worth talking about submitting for examination a morning portion of urine, collected in accordance with all requirements, after a thorough hygienic toilet of the genitals.
In conclusion, let’s say: despite the fact that you know what blood and urine indicators may be during ARVI, visiting a doctor to interpret the results is mandatory! Remember, only a specialist with a higher medical education can correctly evaluate the data obtained and develop the only correct tactics for your further management.
What are viruses
A virus is a tiny organism that can exist and reproduce only inside living cells. In the external environment, the virus is found in microparticles of biological material, but multiplies exclusively in the cells of living beings. In other words, the virus is not active until it is inside a person2.
And he gets there like this:
- Airborne, like most respiratory infections
- When drinking dirty water, with food, or not following hygiene rules
- From mother to unborn child
- Contact – in close contact through the skin or mucous membranes
- Parenterally - bypassing the gastrointestinal tract, by injection
After entering the body, the virus first attaches to the cell, then delivers its biological genome into it, loses its envelope, and only then multiplies. After reproduction, the virus leaves the cell, and the infectious agent spreads along with the blood, continuing total infection. Viruses can suppress the immune system2.
Microbiological cultures
What is microbiological culture? Microbiological culture is a study in which any biomaterial (blood, urine, mucus, pus, etc.) is transferred from the body to a nutrient medium, and if the transferred biomaterial contains microbes, they grow in this medium. In some cases, we combine microbiological cultures with PCR (polymerase chain reaction) research, because not all microbes grow well on media, but are easily detected by PCR, and vice versa, some microbes are poorly detected by PCR, but grow well on nutrient media. PCR is widely used to determine viral infections.
What biomaterials of the body can be tested on nutrient media. In our clinic you can inoculate almost any biomaterial: eye and nasal discharge, material obtained during puncture, saliva, various smears, sputum, feces, urine, blood, skin scrapings, hair (if there is a scalp infection), nails and etc.
Based on the readiness of microbiological inoculation, the sensitivity of the inoculated microbes to various antibiotics can be determined. After determining the sensitivity, it will be clear which drug will be suitable for treatment. It is also possible to determine the sensitivity of microbes to bacteriophages in cases where treatment without the use of antimicrobial chemotherapy is required.
Symptoms of mononucleosis
In young children under 5 years of age, primary EBV infection is usually asymptomatic. Symptoms of infectious mononucleosis most often develop in adolescents, and slightly less often in adults. The average incubation period is 40 days. At this time, the patient experiences increased fatigue.

The disease occurs in 3 phases:
1. Fever - the temperature rises during the day, reaching its peak in the evening. Reaches +40 C, but can be higher, subsides by morning.
2. Pharyngitis (inflammation of the pharynx and tonsils) - is severe, with severe pain. The mucous membranes turn red, swell, and exudate may form.
3. Adenopathy - generalized enlargement of lymph nodes. Changes can be noticed visually and by palpation of the posterior and anterior cervical lymph nodes, submandibular, axillary and inguinal. The lesion is symmetrical and can be observed on any group of nodes. In some cases, adenopathy may be the only sign of infection.
Depending on the individual characteristics of the body and the presence of other diseases, mononucleosis in some people can cause the following symptoms:
- Splenomegaly is an enlarged spleen, found in 50% of cases.
- Hepatomegaly - an increase in the size of the liver, pain when tapped.
Other symptoms include jaundice, swelling around the eyes, and broken capillaries (petechial rash).
Treatment of infectious mononucleosis
- Maintenance therapy.
- Corticosteroids for severe disease.
Treatment of infectious mononucleosis is aimed at stopping palogolic processes, preventing their development in the future, preventing complications, residual effects and the chronic course of the disease.
First of all, the patient must be provided with rest. During the period of enlarged spleen, physical activity and sports are prohibited. Heavy lifting should be avoided to reduce the risk of splenic rupture. To reduce symptoms and speed up recovery, drug and non-drug treatment methods are used.
Drugs for etiotropic, symptomatic therapy and immunocorrection are indicated:
- interferons;
- immunoglobulins;
- nucleosides and nucleotides, except reverse transcriptase inhibitors;
- derivatives of propionic and acetic acid;
- triazole derivatives;
- adrenomimetics;
- antibiotics;
- macrolides;
- glucocorticoids;
- solutions affecting water-electrolyte balance for detoxification;
- mucolytic drugs and others depending on the symptoms.
Antibiotics are prescribed only for viral-bacterial infections confirmed by microbiological diagnostics. If complications occur, corticosteroids may also be prescribed. It is believed that they help to get rid of fever faster and reduce the manifestation of pharyngitis. They are useful for complications such as threatened airway obstruction, hemolytic anemia, and thrombocytopenia.
The most effective methods of non-drug treatment include physical therapy, sanitation of the nasal passages, and frequent ventilation of the room. Depending on the extent of the disease, treatment can be carried out on an outpatient basis or in a hospital.
Analysis of cerebrospinal fluid for neuroinfections. Examination of cerebrospinal fluid for viruses, bacteria, fungi
Our clinic specializes in neurology, neuroimmunology and the treatment of autoimmune diseases of the nervous system. The study of cerebrospinal fluid for neuroinfections is one of the most reliable methods for laboratory diagnosis of inflammatory and autoimmune diseases of the nervous system. We will offer you a study of cerebrospinal fluid for neuroinfections on an outpatient basis, with a stay in the day care ward. Read more about the procedure for obtaining cerebrospinal fluid.
A number of studies for neuroinfections can also be performed using blood tests: more details.
Which neuroinfections are available for research in our clinic:
| Chlamydia trachomatis PCR |
| Herpes simplex virus types 1 and 2 / Herpes simplex virus I, II PCR |
| The causative agent of syphilis / Treponema pallidum PCR |
| Cytomegalovirus / Cytomegalovirus PCR |
| Epstein-Barr virus / Epstein Barr virus PCR |
| Herpes virus type 6 / Human herpes virus VI PCR |
| Pathogen of tuberculosis / Mycobacterium tuberculosis complex PCR |
| Listeria / Listeria monocitogenes PCR |
| Toxoplasma / Toxoplasma gondii PCR |
| Microscopic examination of a stained smear (bacterioscopy) |
| Culture of microflora and determination of sensitivity to antibiotics |
| CSF culture for meningococcus |
| Culture for fungi of the genus Candida and determination of sensitivity to antimycotic drugs |
| Culture for anaerobic microflora and determination of sensitivity to antibiotics |
| Culture for gonococcus and determination of sensitivity to antibiotics |
| Serological diagnosis of tick-borne borreliosis using immunochip method (blood + CSF) |
| Enterovirus / PHK Enterovirus PCR |
| Varicella-Zoster virus (causative agent of herpes zoster) / Varicella-Zoster PCR |
| Adenovirus / Adenovirus (groups B, C, E) PCR |
The study of cerebrospinal fluid helps to make a differential diagnosis between neuroinfection and demyelinating disease, neurosarcoidosis, neuroleukemia, etc. CSF examination helps diagnose neuroborreliosis in doubtful cases. It is also possible to examine the cerebrospinal fluid for the presence of oligoclonal Igg antibodies to diagnose multiple sclerosis.
Carrying out a lumbar puncture. Lumbar puncture is a method of obtaining cerebrospinal fluid for laboratory testing. You can find out more information about lumbar puncture here.
To perform a lumbar puncture, we may need:
- MRI of the brain. If you have brain images no more than 3 months old, please bring them to the clinic. This is important for your safety: there may be risks.
- Examination by a neurologist. The doctor who will perform a lumbar puncture must know exactly the indications for this study in your case and understand the possible risks.