Indications for the purpose of the study
A general clinical blood test is the most prescribed laboratory test for the quantitative and qualitative assessment of the main classes of blood cells.
The study includes determination of the concentration of the main blood elements (erythrocytes, leukocytes, platelets), hemoglobin level, hematocrit value, as well as calculation of erythrocyte indices (MCV, RDW, MCH, MCHC).
Erythrocytes (red blood cells) usually make up about 40% of blood volume. Their main function is to transport oxygen from the lungs throughout the body. The lifespan of an erythrocyte is on average 120 days. Thus, the bone marrow must continually produce new red blood cells to replace those that age and disintegrate or are lost through bleeding. Changes in the number of red blood cells are usually accompanied by changes in other indicators: hematocrit and hemoglobin level.
Hematocrit is the ratio of the volume of red blood cells to the volume of all components called whole blood; in practice, it is the proportion that all formed elements (quantitatively, mainly red blood cells) make up of the total blood volume.
Hemoglobin is an iron-containing protein found in all red blood cells that gives the cells their characteristic red color. Hemoglobin allows red blood cells to bind to oxygen in the lungs and carry it to tissues and organs throughout the body.
Most often, a low hemoglobin level is combined with a low red blood cell count and low hematocrit and indicates anemia.
Norm of indicators
When studying blood biochemistry standards, you can notice insignificant variability: when deciphering a biochemical blood test, the patient’s age, gender, and physiological state are taken into account. The upper and lower limits of normal were determined based on a study of healthy people. For ease of use, the norms of BAC indicators in adults are given in the table.
Biochemical blood test standards:
| Substance | Indicator name | Unit | For men | For women |
| Squirrels | Total protein | g/l | 64-83 | 64-83 |
| Albumen | 33-50 | 33-50 | ||
| SRB | mg/l | up to 0.5 | up to 0.5 | |
| Hemoglobin | g/l | 130-160 | 120-150 | |
| Pigments | Total bilirubin | µmol/l | 3,4-17,1 | 3,4-17,1 |
| Bilirubin indirect | Up to 20 | Up to 20 | ||
| Direct bilirubin | 0-3,4 | 0-3,4 | ||
| Carbohydrates | Glucose | mmol/l | 3,88-5,83 | 3,88-5,83 |
| Fructosamine | µmol/l | 205-285 | 205-285 | |
| NAV | Creatinine | 44-106 | 44-97 | |
| Urea | mmol/l | 2,4-6,4 | 2,4-6,4 | |
| Uric acid | µmol/l | 210-420 | 145-350 | |
| Enzymes | ASAT | U/l | Up to 41 | Up to 31 |
| AlAT | Up to 41 | Up to 31 | ||
| Alpha amylase | 27-100 | 27-100 | ||
| Alkaline phosphatase | Up to 270 | Up to 240 | ||
| Inorganic substances | Iron | µmol/l | 11,6-30,4 | 8,9-30,4 |
| Chlorine | mmol/l | 98-107 | 98-107 | |
| Potassium | 3,5-5,5 | 3,5-5,5 | ||
| Calcium | 2,15-2,5 | 2,15-2,5 | ||
| Phosphorus | 0,87-1,45 | 0,87-1,45 | ||
| Lipids | Total cholesterol | 3-6 | 3-6 | |
| LDL | 2,2-4,8 | 1,92-4,51 | ||
| HDL | 0,7-1,83 | 0,8-2,2 |
Main causes of anemia:
- Bleeding - acute (in case of injuries) or chronic (for example, in diseases of the gastrointestinal tract, organs of the urogenital tract).
- Nutritional deficiencies (iron, folic acid, or vitamin B12 deficiency).
- Damage to the bone marrow, such as from toxins, radiation or chemotherapy, or associated with severe infections.
- Bone marrow diseases (aplastic anemia, myelodysplastic syndrome), cancer (leukemia, lymphoma, multiple myeloma) or other types of diseases that spread to the bone marrow.
- Severe and chronic kidney disease, which leads to decreased production of erythropoietin (a hormone that stimulates the production of red blood cells in the bone marrow).
- Chronic inflammatory diseases.
- Decreased hemoglobin production (eg thalassemia).
- Excessive destruction of red blood cells, such as hemolytic anemia caused by autoimmune diseases or defects in the red blood cells themselves (hemoglobinopathy, red blood cell membrane abnormalities (eg, hereditary spherocytosis)).
Erythrocyte indices are calculated indicators that provide the doctor with information about the physical characteristics of red blood cells and are an important laboratory tool for diagnosing anemia and monitoring the effectiveness of therapy.
Platelets are shaped, non-nucleated blood cells that participate in the formation of thrombi (blood clots). Platelets are capable of “sticking” (aggregating) with each other and adhesion (“sticking” to the damaged vascular wall), which allows them to form a temporary clot and stop bleeding in small vessels.
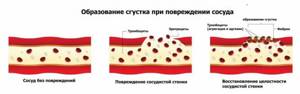
If there are not enough platelets or platelet function is impaired, a stable clot may not form and there is a risk of excessive bleeding. Platelets "live" in the bloodstream for 8 to 10 days, so the bone marrow must continually produce new platelets to replace those that age, become depleted, and/or are consumed by bleeding. Determining the number of platelets in your blood can help diagnose a number of diseases associated with too few or too many platelets.
Leukocytes (white blood cells) are the main cells of the immune system and the basis of the body's antimicrobial defense. They protect against infections and also play an important role in inflammation and allergic reactions.
In addition to infections and inflammation, there are a number of conditions that can affect the production of white blood cells in the bone marrow or the survival of white blood cells in the blood, such as cancer or an immune disease, which results in either an increase or decrease in the number of white blood cells in the blood. The white blood cell count, along with other components of a complete blood count, alerts the practitioner to possible health problems in the patient.
There are five types of leukocytes, each of which performs its own function: depending on the presence of specific granules in the cytoplasm of the cells, a subgroup of granular leukocytes (neutrophils, basophils, eosinophils) and non-granular leukocytes (lymphocytes and monocytes) are distinguished.

A high white blood cell count, called leukocytosis, can result from a number of conditions and diseases. Here are some examples:
- infections, most often caused by bacteria and some viruses, less often by fungi or parasites;
- inflammation or inflammatory conditions such as rheumatoid arthritis, vasculitis or inflammatory bowel disease;
- leukemia, myeloproliferative neoplasms;
- conditions leading to tissue death (necrosis), for example, trauma, burns, surgery or heart attack;
- allergic reactions.
A low white blood cell count (leukopenia) can result from conditions such as:
- bone marrow damage (eg, toxins, after chemotherapy, radiation therapy);
- bone marrow diseases, where the bone marrow does not produce enough white blood cells (eg, myelodysplastic syndrome, vitamin B12 or folic acid deficiency);
- lymphoma or other cancer that has spread (metastasized) to the bone marrow;
- autoimmune disorders - the body attacks and destroys its own white blood cells (for example, lupus);
- dietary deficiency (eg, vitamin B12 deficiency);
- suppressive infections (eg, sepsis);
- diseases of the immune system, such as HIV, that destroy T lymphocytes.
When white blood cell counts are used to monitor medical conditions, a series of white blood cell counts that continue to rise or fall to abnormal levels indicates that the condition or disease is worsening. A white blood cell count that returns to normal indicates improvement and/or successful treatment.
Blood chemistry
Another test that needs to be taken during pregnancy is a biochemical blood test. With the help of this study, the functions of the organs and systems of the woman’s body are assessed. This study is not mandatory (confirmed by the regulatory documents of the Ministry of Health of the Russian Federation), but if the expectant mother has chronic diseases of the internal organs (chronic pyelonephritis - inflammation of the kidneys, chronic cholecystitis - inflammation of the gallbladder, chronic gastritis - inflammation of the stomach mucosa, etc.), then carry out it is necessary. And since during pregnancy the load on the work of the whole organism increases, it is very important to carry out this study in order to diagnose an exacerbation of a chronic disease in time, therefore the first time the “biochemistry” of the blood must be taken when registering at the antenatal clinic, again at 18-20 and at 30 weeks of pregnancy, unless there is a need to conduct this study at other times.
For biochemical analysis, blood is taken from a vein, strictly on an empty stomach, to eliminate possible inaccuracies in the measurement.
Using this analysis, various metabolic processes in the body of the expectant mother (carbohydrate, lipid, protein), the function of the urinary system (kidneys, bladder), liver and gall bladder are assessed. Of the huge range of biochemical studies, the most important and informative are the protein composition of the blood (albumin and protein fractions), serum iron and total iron-binding capacity of serum (these indicators are important for diagnosing anemia in pregnant women), urea, uric acid, creatinine and blood electrolytes (potassium, calcium , magnesium, sodium), AlaT, AsaT, alkaline phosphate. However, taking into account the clinical manifestations and severity of the chronic process, the range of studies can be significantly expanded.
One of the important biochemical tests is to determine the level of sugar (glucose) in the blood of a pregnant woman. This is especially worth paying attention to for women with increased body weight before pregnancy, as well as women with pathological weight gain during pregnancy, i.e. women at risk for diabetes mellitus in pregnant women (gestational diabetes mellitus).
Preparation for the procedure
Donate blood for analysis on an empty stomach; at least 8 hours must have passed since the last meal. On the eve of the study, it is necessary to eliminate stress (physical and emotional), sudden changes in temperature (bath, sauna), intake of excessively fatty, sweet, spicy foods, and maintain a normal drinking regimen. A blood test is taken before physiotherapeutic procedures and, in agreement with the attending physician, before starting to take certain medications.
In emergency situations, the above rules are offset by the vital need for research, which in such cases is carried out without preparation.
Rules for collecting urine for analysis
Urine is collected in a special sterile container purchased from a pharmacy. For newborn children, urine bags are used. Before collecting a sample, it is important to thoroughly wash your genitals. It is recommended to collect the first morning urine. For reliable research results, a small volume of stream (the first 2 seconds of urination) must be released into the toilet, then place a container and collect 50-100 ml of urine into it. The edges of the container should not be pressed against the skin. It is advisable to deliver the collected urine to the clinic within 3 hours.
Complexes with this research
Advanced male anti-aging diagnostics Advanced monitoring of key indicators in men aged 40+ RUR 22,630 Composition
Your immunity Analysis of blood system disorders, vitamin D levels and allergic reactions RUR 2,060 Composition
Women's anti-aging diagnostics Monitoring of basic blood parameters in women aged 40+ 7,220 R Composition
IN OTHER COMPLEXES
- Examination during pregnancy. 1st trimester 10,260 RUR
- Examination during pregnancy. 2nd trimester 670 RUR
- Advanced anti-aging diagnostics in postmenopause RUR 19,860
- Future dad 5,600 RUR
- Examination during pregnancy. 3rd trimester 5,820 RUR






