What blood types are there?
There are 4 blood groups.
ABO system
At the end of the 19th century. Australian scientist Karl Landsteiner, while conducting a study of red blood cells, discovered an interesting pattern: in the red blood cells (erythrocytes) of some people there may be a special marker, which the scientist designated by the letter A, in others - marker B, in others neither A nor B were found. Later It turned out that the markers described by Landsteiner are special proteins that determine the species specificity of cells, or antigens. In fact, these studies divided all of humanity into 3 blood groups.
The fourth group was described in 1902 by scientists Decastello and Sturli. The joint discovery of scientists is called the ABO system.
People with the first blood group 0(I) are universal donors, since their blood, taking into account the ABO system, can be transfused to persons with any blood group. Holders of the fourth blood group AB (IV) belong to the category of universal recipients. They can receive blood transfusions of any type.
However, now doctors are striving to transfuse a person with an identical blood type. This rule is deviated from only in extreme cases.
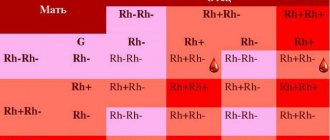
Rh factor
Unlike blood group antigens, Rh factor is an antigen found only in the red blood cell membrane and is independent of other blood factors. The Rh factor is inherited and persists throughout a person’s life. 85% of people whose red blood cells contain the Rh factor have Rh-positive blood (Rh+), the blood of the remaining people does not contain the Rh factor and is called Rh-negative (Rh-).
Kell factor
The Kell system is a blood group system that includes 25 antigens, including the most immunogenic after A, B and D, the K antigen.
Based on the presence or absence of K antigen in red blood cells, all people can be divided into two groups: Kell-negative and Kell-positive. The presence of antigen K (Kell-positive) is not a pathology and is inherited, like other human group antigens. In Russia it occurs in 7-10% of residents.
Currently, blood service institutions determine the presence of antigen K, as the most dangerous for the occurrence of immunological complications. Many cases of blood transfusion complications and hemolytic disease of newborns, the cause of which was isoimmunization with the K antigen, have been described.
Kell-negative patients should only receive blood transfusions from donors who do not have the K antigen to prevent hemolysis. Kell-positive individuals are universal recipients of blood, since they do not experience rejection of its components.
In order to prevent post-transfusion complications caused by the K antigen of the Kell system, departments and blood transfusion stations issue red blood cell suspension or mass that does not contain this factor for transfusion into medical institutions. When transfusing all types of plasma, platelet concentrate, leukocyte concentrate, antigen K of the Kell system is not taken into account.
Therefore, plasma donation is recommended for Kell-positive donors.
Interesting Facts
The Japanese believe that a person's character is influenced by their blood type. Japanese scientist Masahito Naomi, based on research, deduced such a relationship between blood type and human character.
The first blood type is samurai. These people have pronounced leadership qualities. They are ambitious, self-confident, and, as a rule, occupy high positions.
The second blood group is peasants. These are perfectionists. Such people are conservative in everything, they honor traditions and are not used to changing their habits and way of life. He is quite reserved, stubborn, and has his own opinion on everything.
The third blood type is traders. Optimistic, passionate natures. They can be selfish, they always put their interests first, and they will never miss their benefits.
The fourth blood group is artisans. The blood type character of these people is characterized by a rational mindset. They are persistent and can be vindictive.
Oversweetened
But the differences between blood groups are not limited to resistance and vulnerability to certain microbes alone. The fact is that the genes of the ABO locus, which are responsible for AB0 (surface antigens of red blood cells), encode not the sugar plaques themselves, but the enzymes that attach them. And nothing prevents these enzymes from sticking excess galactose somewhere else.
Sometimes such an addition can enhance the activity of the protein - for example, if it is a signaling molecule, then it will begin to stick better to its target. And this does not always benefit the body: if any growth factor is overactive, then the cells begin to divide more often than expected. This may be why people with blood type II (A) are more likely to develop tumors in a variety of organ systems, from the blood to the esophagus and vagina.
Another example is the ICAM-1 molecule in the walls of blood vessels. When it is attached to the surface of cells, it allows white blood cells to adhere tightly to the wall and crawl through it into the tissue from the blood. When ICAM-1 floats in the bloodstream, it, on the contrary, prevents leukocytes from entering the tissue. People with blood type A have suspiciously little dissolved ICAM-1 - and at the same time, inflammation, for example, atherosclerosis, occurs more often. And although it is still unclear exactly what exactly happens to ICAM-1 in their body, it can be assumed that the extra sugar residue prevents enzymes from biting off the molecule from the cell surface, so there is less of it in the bloodstream, leukocytes more often stick to the walls of blood vessels - and hence frequent inflammation occurs.
Other molecules, on the contrary, work worse due to the addition of galactose. This happens, for example, with von Willebrand factor, one of the participants in blood clotting. The extra sugar residue gives it stability, so in people with the first blood group (0), von Willebrand factor is destroyed faster and its concentration in the blood is lower. Therefore, people with the H antigen benefit in all cases where it is good to have thinner blood: they are less likely to form blood clots and develop stroke and myocardial infarction. And in the same way, the first blood group loses where coagulation, on the contrary, is useful - for example, in the case of intestinal ulcers, when bleeding can be fatal.
Blood type: risks and compatibility
Before a person receives donated blood, doctors will check its compatibility. Giving someone the wrong blood type can lead to potentially life-threatening reactions and complications.
If a person with a group B antigen receives red blood cells from a person with a group A antigen, their body mounts an immune response and rejects the transfused blood. The anti-A antibody in the recipient's plasma will attack and destroy the red blood cells of the antigen A donor.
When the recipient's plasma attacks and destroys the donor cells, the blood may clump or agglutinate. This can lead to the formation of blood clots, which can block blood vessels. If the vessels burst, intoxication may begin due to leaked hemoglobin.
Other possible side effects include allergic reactions and anaphylaxis. In some cases the body can cope, but others can be life-threatening.
Some reactions occur immediately, while others may take up to 28 days to develop.
Additionally, blood may sometimes contain unexpected antibodies, viruses, or parasites. The donor may not have symptoms, but they may affect the health of the recipient.
Doctors and other specialists perform detailed tests and screenings before a patient can receive donated blood, plasma or other blood products.
Who can live well during a pandemic?
As much as we would like to believe that everyone is equal in the face of illness, this is rarely true. And COVID-19 was no exception. As soon as there were enough patients with the new disease to form a sample, statistical calculations began and attempts were made to understand who was at greater risk than others and who was less vulnerable (we collected them in the material “We Are Here”). And in the list of risk factors, in addition to the most obvious ones - gender, age, pregnancy and serious illnesses - blood type appeared.
First, Chinese doctors noticed that patients with the first (0) blood group are less likely to end up in hospital with a coronavirus infection - only 26 percent of them were counted there, compared to 33 percent on average for the population. And although not everyone was able to later confirm this correlation, in most studies it was repeated, and most often the winners were precisely people in the first group (0), who, according to various estimates, were less likely to catch the coronavirus, were more mildly ill and died less often.
The pandemic has not yet given doctors time to understand in detail the mechanisms of this pattern. But given what we already know about the inequality between carriers of different blood types, it is not surprising. SARS-CoV-2, like many other viruses, multiplies in our cells and is covered with their membrane at the exit - which means, like HIV and SARS-CoV-1, it can camouflage better in the body of people with A- or B-antigens or stronger stick to sugar residues on the surface of cells.
Problems with the “distribution” of red blood cell antigens to other cells also play a role. Lagging extra sugars onto the ICAM molecule leads to more severe inflammation, which is often associated with coronavirus pneumonia. And an excess of von Willebrand factor in the blood of people with the second (A), third (B) and fourth (AB) blood groups increases the formation of blood clots - for which COVID-19 is also notorious.
However, one should not be too envious of those whom nature has deprived of galactose residues on the membrane proteins of erythrocytes. Like many other human characteristics, blood types are useful because of their diversity. Each new infection hits some people harder than others, leaving humanity a chance to survive it and move on. This time, carriers of “shaved” red blood cells were lucky - but who knows what pandemic will be next?
What can a child inherit?
The principles of transmission of hereditary characteristics from parents to children were formulated more than a century and a half ago by the Austrian biologist, monk Gregor Johann Mendel. Mendel's experiments were understood and recognized only half a century after his death. Thus, classical genetics appeared at the beginning of the 20th century, Dmitry Okunev, a therapist and senior medical consultant at the Teledoctor24 service, tells Izvestia.
“Despite this, today parents are still concerned about the same questions: who will the baby look like, why did he become the owner of wonderful curls or a square chin. At this point, it is appropriate to recall that brown eye color and the gap between the front teeth are caused by a dominant gene, and the gene for straight hair is recessive, explains the doctor.
Blood for blood
Photo: Depositphotos/Paha_L
Pathogenic engineering: Izvestia found a patent for an “invisible” assembly of the genome of viruses
This method makes it possible to discreetly modify SARS-like microorganisms
According to him, recently in Russia there has been a steady increase in diseases transmitted by inheritance. Approximately 35–40 children suffer from them per thousand newborns.
— If we talk about the characteristics of hereditary diseases, then daughters are passed on from their mothers not only a tendency to be overweight and the entire range of characteristics of the monthly cycle, but even such a formidable disease as migraine (associated with the level of female sex hormones), depressive states, eye disease glaucoma and osteoporosis , metabolic disease. At the same time, the main parental figure for the child remains the maternal grandmother,” says Izvestia’s interlocutor.
On the paternal side, boys are transmitted the characteristics of the functioning of the male reproductive system, the degree of baldness and testosterone levels. In addition, heart and dental diseases can be transmitted to the child.