Shoulder rehabilitation – restoration of functionality after various injuries and surgeries. Necessary for severe impacts, bruises, sprains, partial or complete rupture of muscle tissue, after endoscopic surgery and endoprosthetics.
The motor activity of the shoulder joint can be restored using a set of measures, from functional diagnostics using the Kaltenborn-Event method to the use of soft manual techniques, PNF, exercise therapy, physiotherapy, and massage. During rehabilitation, the biomechanics of the joint is taken into account for each individual disease.
Diagnosis of shoulder joint diseases
An important stage in the rehabilitation of the shoulder joint is diagnosis. To determine the cause of the shoulder joint pathology and find a solution, the rehabilitation specialist asks the patient to perform a series of simple anatomical and functional movements.
The pain that occurs at this moment will help determine its source and find the cause of the disease. The doctor also determines the consequences of the injury, for example, restriction of movements in the joint, or, conversely, their excessive mobility.
The specialist performs palpation to identify tension in the muscles, the presence of compactions and swelling, examines the patient’s reflexes and muscle strength, and checks the nerve endings for sensitivity. Then he tests hypotheses using manual techniques and determines the necessary methods for effective treatment and restoration of joint mobility.
Prices and manufacturers
Postoperative bandages have a wide range of prices. Depending on the manufacturer and material of manufacture, the cost varies from 1,500 to 10,000 rubles. Today the most popular manufacturers: Otto Bock. They make inexpensive products, but the quality is at the highest level. Comfortable to wear, easy to use and maintain. Trives. They produce a wide range of braces for the shoulder joint, from economy to premium class. The manufacturer is known not only in the Russian Federation, but also abroad. Medi. Bandages made in Germany have a very high price. But they occupy a leading position in the market. This brand also produces various types of orthoses. Orlett. They produce several types of fixation products for children and adults. After arthroscopy of the shoulder joint, the doctor will advise which type of brace is best to choose in your case. The duration of wearing is determined individually. Before purchasing a fixation product, be sure to consult your doctor.
| Complex therapy from leading medical specialists at the GarantKlinik center |
| Comprehensive orthopedics from leading medical specialists at the GarantKlinik center |
| Comprehensive cosmetology from leading medical specialists at the GarantClinic center |
| Complex phlebology from leading medical specialists at the GarantKlinik center |
— How to make an appointment for surgery to remove a lump on your leg at GarantKlinik in Moscow?
— Arthroscopy in Moscow at the Garant Clinic.
The leading clinic on the basis of the Sechenov First Moscow State Medical University is GarantClinic.
Manual therapy in the treatment of the shoulder joint
Once a preliminary diagnosis has been established, the rehabilitation process begins. The first task of specialists is to reduce pain. For this purpose, general immobilization is used, that is, bed rest to ensure immobility in the damaged joint, local immobilization using tapes, elastic bandages, and casts.
To gradually restore the functionality of the shoulder joint, gentle manual techniques are used. Their difference from traditional methods of treatment is that recovery occurs due to the patient’s own muscle strength. Ligaments and muscles are not stretched or injured, but rather come closer together, which helps relieve tension and pain.
The rehabilitation program uses proprioceptive neuromuscular facilitation. The essence of the technique is to restore the motor activity of the affected muscles associated with them by influencing healthy areas of the shoulder and shoulder girdle. The specialist stretches, compresses, twists the muscles to influence the proprioceptors that they contain. They, in turn, transmit the resulting impulses to the central nervous system, which forces them to perform a certain action. Thus, it is possible to initiate movements of damaged limbs, increase their volume, significantly facilitate recovery, and reduce pain.
To restore the shoulder joint, the following exercises are performed:
- Concentration is the tensing of strong, healthy muscles in order to excite weakened muscles.
- Elongation is muscle stretching. The rehabilitator first fully stretches them, while affecting the adjacent joints near which movements occur.
- Traction is the pulling of articular surfaces. It is carried out before the start of movement, it brings the parts of the limb closer together.
- Compression - bringing the surfaces of the joints closer to each other. It is used before the start of movements that push away parts of the limb.
The use of these rehabilitation methods according to the principles of biomechanics gives a long-lasting effect. While traditional trust recovery methods work temporarily, they carry a high risk of relapse and serious complications: sprains, bruises, dislocations. Gentle manual techniques and PNF are excellent for treating the elderly, children and debilitated patients.
After eliminating the pain syndrome, a special set of exercises is used to rehabilitate the shoulder. It is designed in stages and helps the patient to gently and gradually mobilize the joint in the first days after injury or surgery, and then return it to full functionality. Exercises are performed according to a clearly developed scheme, regularly and for a long time. Physical activity during rehabilitation with exercise therapy increases gradually. Since excessive activity and a premature increase in the range of motion in the joint leads to new injuries and complications.
What is the difference between a bandage and an orthosis?
Many people do not distinguish between orthoses and bandages. Indeed, they have the same function - fixing. But still, there are some differences. Bandages are “softer” retainers, consisting of elastic fabric of varying hardness. Orthoses, in turn, are considered more complex structures that have pins, metal plates and other similar elements inside. Orthotic structures are prescribed when there is a need to adjust the angle of fixation of the shoulder girdle and upper limb. Bandages have a broader purpose - they are required after surgery on joints; depending on the severity, different types of products can be prescribed.
Rehabilitation after a dislocated or fractured shoulder
Dislocation of the shoulder joint is a posterior and anterior displacement of the humerus with prolapse from the clavicular cavity. The shoulder joint is the most sensitive and most flexible of all. This mobility increases the risk of injury. Dislocations often occur after accidents and falls on an outstretched arm. In addition, as you age, the joint begins to wear out, so the risk of injury increases.
Most often, a dislocated humerus can be treated without surgery. Dislocation of the shoulder joint is eliminated by qualified specialists. They push the humeral head into the socket. In rare cases, when capsules, ligaments, vessels and nerves are damaged, the patient may require surgery.
After injury, the shoulder joint is usually fixed using elastic and sling bandages and orthoses. In case of a fracture, a plaster cast is required. A plaster cast fixes the joint in the correct position and completely removes the load from the arm and shoulder.
The patient wears the braces for two to three weeks, and the cast for about a month or a little more. During this time, muscle tone weakens significantly, they atrophy, tendon ligaments lose their natural elasticity, blood circulation slows down due to compression of blood vessels. Therefore, after a dislocation or fracture of the shoulder joint, a whole range of rehabilitation measures is very important. In addition to the above-mentioned soft manual techniques, exercises for clenching the fingers into a fist and flexion-extension at the elbow joint are prescribed for recovery. Then the intensity of the load gradually increases; you can use dumbbells, balls, and weights.
Examples of exercises with dumbbells that are used to restore the functionality of the shoulder joint after dislocation and fracture:
- The patient raises his arms above his head, then lowers them completely. The exercise must be repeated 10-15 times for each hand. Then the arm needs to be extended forward and bent at the elbow joint.
- Throwing exercise. The patient takes the ball and throws it with his hand, as if he wants to throw it into the basket.
- Circular movements of the shoulder. Rotation occurs clockwise and then counterclockwise.
- The patient moves his hands behind his back and forms a “lock”.
- Clenches and unclenches the fingers into a fist.
How is knee arthroscopy performed?
Before knee arthroscopy, your doctor will prescribe an anesthetic (anesthesia). It could be:
If you are awake, you may be able to watch the procedure on a monitor.
- The surgeon will make several small punctures (1-2) in the area of your knee joint.
- A sterile saline solution will then be injected to enhance the video quality on the monitor.
- An arthroscope is inserted into one of the punctures, and the surgeon examines your joint using an attached camera.
- When the surgeon finds a problem in your knee joint, he may insert small instruments into the incisions to correct the problem.
- After surgery, the surgeon drains the saline solution from the joint and stitches the punctures.
Shoulder rehabilitation after arthroscopy
Shoulder arthroscopy is a minimally invasive surgical procedure in which all manipulations are performed with an arthroscope through small incisions. The image of the shoulder joint is displayed on the monitor using a special camera. This allows the surgeon to diagnose and stitch small tears in the soft tissue of the joint without making a large incision or opening it completely. Arthroscopy is prescribed if there is a suspicion of hyaline cartilage injuries or ruptures of the articular menisci. The degree of connective tissue damage after arthroscopy is much lower, so the rehabilitation period is significantly reduced and the risk of complications is minimal.
Rehabilitation after arthroscopy of the humerus takes a long time, about 4-6 months. In the first days, drug treatment is carried out, which is aimed at pain relief in the joint and preventing the inflammatory process. The attending physician regularly changes the dressing and applies cold compresses. The operated arm is fixed with a special orthosis.
Rehabilitation classes begin on the second day. First, light breathing exercises and general tonic complexes for small and medium muscle groups are used.
After the patient’s general condition has improved, the task of rehabilitation therapists is to activate the motor mode. The arm is in a bandage for 3-4 weeks, movements are limited. Therefore, classes are aimed at training the muscles of the external rotators of the shoulder and biceps, preventing wasting of the muscles of the shoulder girdle and improving blood circulation. For this purpose, massage, electrical stimulation, muscle training in isometric mode, and PNF are used.
The patient consistently performs active and passive movements on the healthy side in order to form a program of actions and remember the exercises. Then the trainer invites him to perform all the same movements mentally on the operated side. Only after this the patient begins to perform rehabilitation exercises on the sore arm with a measured load. During this period, you can use gymnastic balls, sticks and other light objects.
To reduce contractures, the patient tries to tense the muscles of the shoulder joint: raise the arm, connect the shoulder blades, push the shoulder forward. At this time, the trainer counteracts the patient’s movements. Then the muscles that surround the shoulder joint tense in the same way. With each new approach to the exercises, the range of motion gradually increases by several degrees. This method of rehabilitation makes it possible to get rid of myogenic contracture without compromising the stability of the head of the shoulder joint and without stretching the capsule.
To consolidate the results obtained, it is important to apply therapeutic positioning of the operated shoulder in the correction position. The shoulder joint is fixed in the abduction position using sandbags. The patient lies on a couch or sits at a table. At first, styling takes 5 minutes, then the correction time can be increased.
Rehabilitation classes are held every day, their intensity gradually increases. At first, you may feel some discomfort during exercise. This is a protective reaction of the body, which is expressed in reflexive muscle tension. If the patient experiences severe pain in the joint and swelling, then the load is reduced. In some cases, rehabilitation is stopped for a while.
The next stage is a dosed force load on the muscles, which ensures the stability of the position of the head of the shoulder joint. The patient performs straight and bent arm movements forward, to the side, inward rotation, and flexion of the forearm with weights and counteraction. Exercises should be performed slowly, lying or standing. At this stage, you can already use expanders and dumbbells.
Also of great importance is increasing endurance to long-term static and dynamic loads of the shoulder muscles. To do this, exercises are performed with holding the hand in a certain position for a long time. To increase the load, weights are used.
results
No complications were observed in the subjects during or after the operation.
All subjects completed the one-year prospective study on time.
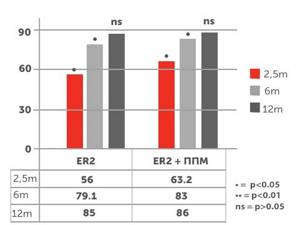
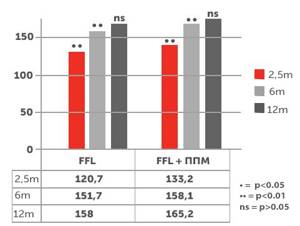
At the first stage of the prospective study, conducted 2.5 months after surgery, subjects from group B had statistically significant higher scores on the VAS scale (7.5 ± 0.1) (P < 0.01), FF (133 ± 21.1) (P < 0.01) , ABD (66.7 ± 14.5) (error < 0.05), ER2 (63.5 ± 15.4) (P < 0.05) than in subjects from the group, A on the VAS scale (9.1 ± 0.2), FF (120.7 ± 20.6), ABD ( 60.1 ± 14), ER2 (56 ± 14).
After 6 months, a prospective study gave the following results: in patients from group B, FF scores were still significantly different (158.1 ± 9.4) (P < 0.01), ABD (86.9 ± 5.3) (P < 0.01), ER2 (83 ± 7.7 ) (P < 0.05), while patients from group A had the following indicators: FF (151.7 ± 12.5), ABD (82.3 ± 7.6), ER2 (79.1 ± 7.4). There were no statistically significant differences in VAS scores between group B (0.5 ± 0.1) and group A (0.6 ± 0.1) (P > 0.05).
At the third stage of the prospective study (after 12 months), no statistically significant differences in parameters were detected in both groups. In group B, the VAS scale scores are as follows: (0.2 ± 0.1) (P > 0.05), FF (165.2 ± (P > 0.05), ABD (90 ± 2.5) (P > 0.05), ER2 (86 ± 4) (P > 0.05), while in group A the values on the VAS scale are as follows: (0.2 ± 0.2), FF (158 ± 10.1), ABD (88 ± 1.8), ER2 (85 ± 4.2).
In group B, the VAS scale scores are as follows: (0.2 ± 0.1) (P > 0.05), FF (165.2 ± (P > 0.05), ABD (90 ± 2.5) (P > 0.05), ER2 (86 ± 4) (P > 0.05), while in group A the values on the VAS scale are as follows: (0.2 ± 0.2), FF (158 ± 10.1), ABD (88 ± 1.8), ER2 (85 ± 4.2).
Figures 1, 2 and 3 show a summary of the results of range of motion restoration in both groups of patients.
Rice. 1 — Results on the degree of arm abduction in group A (ABD) and in group B (ABD + PPM) at 2.5 months, 6 and 12 months.
Rice. 2 — Results on the degree of forward flexion of the arm in group A (FFL) and in group B (FFL + PPM) at 2.5, 6 and 12 months.
Rice. 3 — results on the degree of excess rotation during arm abduction in group A (ER2) and in group B (ER2 + PPM) at 2.5, 6 and 12 months.
Shoulder arthroplasty
A surgical procedure to replace shoulder components using implants. It is carried out in order to restore lost motor functions of the shoulder in all directions and return the patient to normal life. Endoprosthesis replacement is used in cases where conservative methods of treating the joint have proven ineffective.
Here are the indications for the operation:
- wear of articular surfaces, which is caused by degenerative-dystrophic diseases of the joints: osteoarthritis and arthritis;
- shoulder bone tumors;
- infectious inflammation of the shoulder joint;
- severe fractures and serious injuries to the shoulder, which caused circulatory problems in the cartilage tissue or avascular necrosis - death of the bone tissue of the joint, resulting from compression of the vessels and nerve fibers that feed it.
- joint instability - increased mobility of the joint and weakening of the connective tissue, in which the head of the humerus periodically comes out of the socket of the shoulder joint, most often develops after injury.
- congenital joint defects.
- chronic polyarthritis is inflammation of the shoulder joint that has become permanent.
Rehabilitation begins almost immediately after installation of the prosthesis; the arm is mobilized using a scarf. All exercises are performed under the strict supervision of a rehabilitation specialist. During the first week, only passive warm-up is performed to prevent overstrain of the muscles that are in the first stage of regeneration. These are light, calm movements of the wrist, fingers and forearm. Then the patient begins to work the muscles of the back and neck. Only after 3 weeks are more intense movements with light loads allowed.
After three months, you can begin active rotational movements, abduct and adduct the shoulder to the head.
At 15 weeks after shoulder surgery, you can use 1 kg dumbbells, bend and straighten your arm, and lift it up and down.
Contraindications to knee arthroscopy
Knee arthroscopy is contraindicated in the presence of such ailments as:
- Local skin inflammation.
- Impaired balance of blood clotting;
- Severe dysfunction of the pulmonary or cardiac systems;
- Diabetes mellitus in the stage of decompensation;
Important!
Therapeutic and diagnostic arthroscopy is performed with caution; the consequences can be unpredictable if you are allergic to local/general anesthetic. Therefore, be sure to tell your specialist if you are prone to allergic reactions to any medications.
Massage after shoulder injuries
Medical or therapeutic massage is a universal remedy for symptomatic and restorative treatment after various injuries and operations on the upper and lower extremities. Therefore, it is also considered an important step during shoulder rehabilitation.
Massage for shoulder injuries has a number of advantages:
- avoids tissue scarring;
- prevents the formation of contractures in the joint area;
- eliminates pain;
- improves blood circulation and stimulates lymph outflow; ensures the supply of nutrients to the affected tissue area;
- accelerates the healing of damaged bone components in fractures of the shoulder joint.
The massage begins with impact on the periarticular tissues. The doctor rubs the shoulder blades, shoulders, and shoulder girdle. Then he makes kneading movements in opposite directions. With his palms he presses on the soft tissues, thus stimulating the outflow of lymph and blood circulation in the joint. Then he repeats light, stroking movements again. Next, the massage therapist begins to knead individual muscles. Works the shoulders, chest and back. If swelling is present, then makes pressing movements towards the distal parts of the arm.
A shoulder joint massage session lasts about 20-30 minutes. To get a good result, you will need a course of 10-15 procedures.
Timely rehabilitation can completely restore joint function after any injuries and operations and return the patient to normal life. A whole range of proprietary methods of manual therapy, physical therapy, massage and physiotherapy accelerates the regeneration of bone tissue, strengthens muscles, increases the range of movements to the maximum physiological level, and eliminates pain.
Recommendations for use and care
Wear the brace strictly as directed by your doctor. Observe the hourly schedule and duration of wearing. If you need to remove it, do it as carefully as possible, it is better to have someone help you. Do not make sudden movements. Do not put the bandage on wet skin, including after applying various creams or ointments. Wait until they are completely absorbed. Please read the instructions carefully. As a rule, they clearly show how to properly put on and secure the bandage. To ensure that the bandage does not lose its properties and does not change visually, follow a few simple requirements. It is advisable to wash by hand; it is not recommended to use a washing machine. The maximum water temperature is 30 degrees. Use only gentle washing powders or gels. This product must not be ironed.
Shoulder rehabilitation training
Specialists from the International Academy of Medical Rehabilitation (IMR) have developed a practical course on shoulder rehabilitation, where they share their knowledge of functional diagnostics and practical experience in the use of biomechanics in the treatment of the shoulder joint. The course will be useful for traumatologists, physiotherapists, massage therapists, and instructors at sports centers. You will gain skills in functional diagnostics, conservative and postoperative treatment of injuries to the shoulder joints. Study in detail the anatomy and biomechanics of the shoulder girdle, the role of muscles, blood vessels and nerves, bones and joints, standards for the amplitude of arm movements in different directions.
The webinars provide detailed examination schemes for the shoulder girdle, including the Kaltenborn-Evient system. Our specialists explain in detail what impact concomitant diseases can have on the shoulder joint: neurological pathologies, gastrointestinal problems, old injuries. As part of the training, our teachers will use specific examples to demonstrate what tests are performed to diagnose diseases, and will analyze what methods are used for recovery after surgery on the shoulder joint. The treatment process is discussed in detail: from the very beginning of conservative treatment, or from the first days after surgery until complete restoration of the functions of the shoulder joint.
For each stage of recovery, its own tasks and methods are determined, including medications, special exercises, massage, and physiotherapy. Our teachers will provide course participants with information that they have collected over many years, share experience and knowledge from their own practice, and talk about techniques that they have personally tested and helped cure thousands of patients. You will master modern diagnostic principles and proprietary methods of treating the shoulder joint, which are not publicly available or in medical textbooks. Gain knowledge that will allow you to reach a new professional level and help patients restore joint mobility without surgery.
Main types
Bandages can be used for various purposes, so there are several types: Restrictive. Looks like a vest with small sleeves. Provides complete immobility of the joint; if necessary, the range of motion can be adjusted with straps. Children's. In childhood, special attention should be paid to the musculoskeletal system. After surgery on the shoulder, it is recommended to wear a children's bandage; it looks like an adult fixation bandage, but is made of natural materials and has appropriate sizes, which are regulated by special Fixation belts. This brace secures the shoulder in the desired position. The patient cannot lift or move the arm. Made of semi-rigid material, it performs its function perfectly. Clavicular. Provides reliable fixation of the shoulders - they are laid back. This product is shaped like a figure eight. Prescribed for damage or fracture of the collarbone in the initial post-rehabilitation period. Supportive. Indicated for shoulder instability. Prevents dislocations and other injuries; as a rule, such bandages are worn for preventive purposes. Made of soft fabric material, does not restrict movement.
Video of knee arthroscopy
Description of the problem:
Meniscal tears
- The most common injury to the knee joint. The meniscus is a natural shock absorber in the knee joint, which, due to its shape, increases the area of contact between the articular surfaces of the knee joint, ensuring an even load on the articular surfaces of the knee joint.
There are traumatic and degenerative injuries to the menisci. Unlike a traumatic meniscal tear, in which pain in the knee joint occurs immediately after the injury, with a degenerative tear, pain often occurs gradually; there is no clear connection between the occurrence of pain and the injury to the knee joint.
An examination by a traumatologist allows in most cases to establish the correct diagnosis and prescribe the necessary treatment. The examination includes examination and x-rays to exclude damage to the bone structure (fractures). Sometimes an MRI (magnetic resonance imaging) scan of the knee may be required.
The gold standard for knee injuries is arthroscopy.
Frequently asked questions (FAQ)
What kind of orthosis is needed after knee arthroscopy?
To achieve the optimal effect from wearing the product, you need to know how to choose an orthosis for the knee joint. It is necessary to understand that these products are prescribed by a doctor after a thorough examination of the joint. To choose the right knee orthosis, you must strictly follow your doctor’s recommendations. Certain product characteristics must also be taken into account.
After knee arthroscopy, when can you walk?
You are allowed to stand up, but walk only with walkers or crutches. It is necessary to protect the leg from full load for at least one week.
After knee arthroscopy, fluid accumulates. What to do?
This may be associated with the development of tissue inflammation.