CCA (general clinical analysis) of blood is a clinical and hematological method for assessing the composition of the main biofluid of the body, the purpose of which is to identify possible disorders. The study of blood composition in laboratory conditions is carried out under a microscope (microscopy “manually”) and on hematological automatic analyzers.
The computer records the final data of the automatic calculation and sends it to print. The study form indicates the decoding of the general blood test in Latin letters (an abbreviation for the full name of the indicator).
Manual counting microscopy takes longer but is considered more accurate. The optimally informative assessment option is an automatic analysis, supplemented by the calculation of a leukogram by a laboratory specialist.
Purpose and information content of a general blood test
OKA is prescribed:
- for symptomatic complaints to identify blood composition disorders;
- to control the therapy of a diagnosed disease;
- as part of a medical examination, medical examination, perinatal screening, military medical commission;
- during hospitalization and before discharge from the hospital (sanatorium).
For children, analysis is mandatory when passing a medical commission for registration in a preschool or educational institution. The doctor can easily read the analysis form with the designation of parameters in Latin and English and, based on the results of the study, can assess the general condition of the body, as well as detect the presence of:
- inflammation;
- anemia;
- infectious processes provoked by viruses, bacteria, protozoan parasites and helminths;
- coagulation disorders (problems with the rate of blood clotting).
The discrepancy between some indicators and norms suggests the activity of cancer cells.
Designation and definition of the main indicators of OKA
All biofluid parameters studied during the analysis are closely interconnected and dependent on each other. Conventionally, correlation indicators can be divided into three groups.
Blood sampling for OKA is performed on an empty stomach
Hemoglobin and red blood cells
90% of the two-component iron-containing protein (hemoglobin) is found in red blood cells - erythrocytes. Their joint efforts ensure blood saturation with oxygen and the respiratory function of the body. To get a complete picture, the laboratory evaluates not only the hemoglobin concentration and the number of red cells, but also related parameters:
- hematocrit - determines the degree of saturation of the bloodstream with red cells;
- erythrocyte sedimentation rate - reflects the speed of blood division into liquid plasma and the cellular part, as well as the ratio of proteins in the biofluid;
- reticulocytes are immature precursors of red cells.
Additional parameters are erythrocyte indices. They are calculated to estimate average values.
Table of designations and indicators corresponding to laboratory standards
| Abbreviation on the results form given to the patient | Parameter under study | References | ||
| For adults | For children | |||
| NV is measured in g/l | hemoglobin | husband. 140-160, women. 120-150 | 120-130 g/l | |
| RBC count the number of cells in 1 liter of blood, multiplied by 10 to the 12th power - 10^12/l | erythrocytes or red blood cells | husband. 3.9-5.6; wives 3.5-5.2 | 4,0-4,5 | |
| HCT | hematocrit | husband. 40-50%, women 37-47% | 33-41% | |
| ESR or ESR measurement value – mm/h | erythrocyte sedimentation rate | husband. 2-15, female 3-20 | 4-12 | |
| RET | reticulocytes | 2-10% (of red blood cell mass) | ||
| erythrocyte indices or average values | ||||
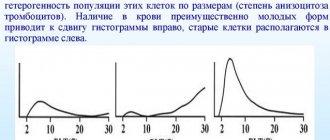
| MCV | red blood cell volume | 78–98 fl (femtoliters) | ||
| MCH | hemoglobin content in one cell | 28 - 32 pg | ||
| MCHC | hemoglobin concentration in the total number of red blood cells | 30 - 37 g/l | ||
Platelets
Blood cells in the form of plates that are responsible for normal coagulation (blood clotting) and also protect the epithelial (inner layer) of the vascular walls. In a clinical blood test, the number of platelets, the percentage of platelet plates in relation to the total blood volume and platelet indices are determined.
Designations and indicators of the norm
| Abbreviation indicated on the final results form | Platelet parameters | References | |
| adults | children | ||
| PCT | platelet crit | 0,15-0,4 | |
| PLT (10^9/l) | platelets or platelets | husband. 180-320 women 150-400 | 160-375 |
| Indexes | |||
| MPV | mean platelet volume | 7-10 fl | |
| PDW | distribution of platelets throughout the blood volume | 11,5-14,5 % | |
Leukocyte cells
Leukocytes are several groups of white blood cells that have the protective function of phagocytosis (capturing and destroying pathogens). When the opportunistic flora of the body is activated or when pathogenic bacteria, viruses, parasites and fungi invade, leukocytes are mobilized, trying to eliminate them.
Leukocyte cells are divided into two large groups, each of which includes subgroups:
- agranulocytes - leukocytes that do not contain azurophilic granules in the cytoplasm (monocytes and lymphocytes);
- granulocytes - leukocyte cells with a segmented nucleus and specific granules in the cytoplasm (neutrophils - segmented and band, eosinophils and basophils).
Laboratory assessment takes into account the absolute number of cells (in units) and the relative number (in percentage). The analysis form most often indicates the absolute number of leukocytes in units and the percentage of individual leukocyte groups.
Table of designations and norm indicators
| Abbr. in the final results form | Parameter under study | Content standard | |||||
| for adults | for children | ||||||
| in units | V % | in units | V % | ||||
| WBC | leukocytes or white blood cells | 4-9 | — | 6-10 | — | ||
| LYM (LY#) (LY%) | lymphocytes | 1,2 — 3,0 | 25-40 | 30-45 | |||
| NEUT (NE#) (NE%) | neutrophils (neutrophils) band/segmented | 2-5 / 55-70 | 1-4 / 40-60 | ||||
| MON (MO#) (MO%) | monocytes | 0,1-0,7 | 6-8 | 4-6 | |||
| EOS (EO#) (EO%) | eosinophils | 2-5 | 1-4 | ||||
| BAS (BA#) (BA%) | basophils | 1 | 0-1 | ||||
| MID (MON+ EOS+BAS) | mixture (monocytes + basophils + eosinophils) | 0,2—0,8 | 5-10 | 5-10 | |||
Units are most often calculated manually. This is the number of cells in a liter of blood (for convenience, the resulting number is multiplied by 10 to the 9th power - 10^9/l).
The importance of triglycerides and lipoproteins in the analysis
Triglycerides are compounds of special fatty acids and glycerol. Basically, these substances accumulate in adipose tissue, while they are contained in small quantities in the blood plasma. Such lipids serve as the main source of energy in the body. But when triglyceride levels rise along with low-density lipoproteins, the risk of developing cardiovascular disease increases dramatically.
Excess triglycerides remaining after being burned and converted into energy synthesize cholesterol and are stored as fat. Triglycerides are designated by the Latin letters TRIG. When triglycerides in the blood exceed more than 2.3 mmol/l, there is every reason to believe that the patient has developing atherosclerosis. A value of more than 5.6 mmol/l is regarded as an extremely high indicator. A value from 1.8 to 2.2 mmol/l is considered normal.
High levels of triglycerides are also observed with high blood sugar. There are two types of cholesterol: low density and high density. Both indicators are crucial in assessing the development of atherosclerosis and predisposition to it. Low-density cholesterol is considered “bad” because it is what settles on the walls of blood vessels in the form of atherosclerotic plaque.
Its structure is such that it practically does not dissolve and is deposited. Low-density lipoproteins are an important indicator in blood biochemistry, since they are the cause of the development of atherosclerosis. These substances are also called atherogenic. They are synthesized in the liver, and their main function is to transport triglycerides into the circulatory system.
Most of these lipids are synthesized by liver cells, and some are obtained from food. When the liver begins to produce such cholesterol in excess, in addition, it comes from the outside, it does not have time to be utilized and accumulates in the body. LDL (low-density lipoprotein) levels range from normal to very high. The optimal value is considered to be a low-density lipoprotein level of no more than 2.6 mmol/l.
Experts consider it acceptable when this indicator is in the range of 2.6–3.35 mmol/l. But when tests reveal an increase from 3.4–4.1 mmol/l, then this is already a borderline value. LDL levels of 4.1 and above 4.9 mmol/l are deciphered as high and very high. Good cholesterol, or high-density lipoprotein (HDL), has anti-atherosclerotic effects.
They do not provoke the deposition of fats on the walls of blood vessels; moreover, they counteract this process. When assessing the results of a lipid profile, a decrease in HDL levels is considered a negative sign. An increase in its level is not regarded as a pathology. The level of high-density lipoproteins is assessed according to values accepted in international practice.
Thus, an HDL level in women less than 0.9 mmol/l is regarded as an indicator of a high risk of developing atherosclerosis and coronary heart disease. If this indicator in adult men is less than 1.16, then it is assessed similarly. The norm for high-density cholesterol for both sexes is more than 1.6 mmol/l. This value indicates a low risk of developing atherosclerosis.
No ads 2
About deciphering blood biochemistry
Along with OKA, a biochemical blood test is a popular test. In the form with the results, the studied parameters can be designated by both Russian and Latin abbreviations. Assessment of the biochemical composition of plasma allows us to identify functional failures in specific organs and systems.

Blood sampling for biochemistry is carried out using disposable syringes or vacutainers
Squirrels
The correct concentration of proteins (proteins) is a sufficient amount of building material for new cells, normal muscle contractions, complete protection of the body from infections, timely movement of hormones, acids, and nutrients through the bloodstream.
| Name | Total protein | Albumen | C-reactive protein | |
| Content standard | in adults | 64-84 | 33-55 | no more than 5 |
| in children | 60-80 | 32-46 | ||
| Abbreviation on the form | Tr | Albu | Crp | |
Laboratory measurement of protein is made in g/l.
Carbohydrates
Sugar normally means proper carbohydrate metabolism and the pancreas producing the required amount of the hormone insulin.
| Name | Glucose | |
| Concentration rate | Adults | 3,3-5,5 |
| Children | ||
| Abbreviation | Glu | |
Measuring value – mmol/l.
Nitrogen compounds
The coincidence of the analysis results with the reference values reflects the full functioning of the renal apparatus.
| Indicator name | Urea | Uric acid | |
| Norm | Adults | 2,8-7,2 | Husband. – 210-420, women. – 150-350 |
| Children | 4,2-7,2 | 120-330 | |
| Abbreviation | Urea | Uric asid | |
The measurement value is µmol/l.
Fats
Normal fat levels are a sign of proper lipid metabolism, healthy blood vessels in the brain and lower extremities, liver, and thyroid gland.
| Name | Cholesterol total | Low density lipoproteins | High density lipoproteins | Triglycerides | |
| Norm | husband. | 3,2-5,2 | 1,7-4,3 | 0.6-1,8 | 1,7 |
| wives | 1,8-4,4 | 0,8-1,8 | |||
| Abbreviation | Chol | LDL | HDL | TG | |
Laboratory value – mmol/l.
Fat-soluble bile pigment
The compliance of the results obtained with the standards indicates the good functioning of the organs of the hepatobiliary system.
| Name | Total bilirubin | Unconjugated bilirubin (free or indirect) | Conjugated bilirubin (bound or direct) |
| Norm | 20,5 | 1,7-17,0 | 0,86-5,3 |
| Abbr. | Tbil | Dbil | Idbil |
In laboratory conditions it is measured in µmol/l.
Enzymes
Normal enzyme levels reflect the uninterrupted processes of digestive chemical reactions, protein and carbohydrate metabolism, stable muscle contractions (including the heart muscle - myocardium), normal functioning of the liver, pancreas, and adjacent organs of the hepatobiliary system.
| Name | Norm | Abbr. | |
| adults | children | ||
| Alanine aminotransferase | husband. 45 women 39 | 29 | Alt, or ALT, AlAT |
| Aspartate aminotransferase | husband. up to 31 women up to 37 | up to 30 | Ast or AST, AsAT |
| Creatine phosphokinase | husband. up to 195 women up to 167 | up to 270 | KFK or KFK |
| Alkaline phosphatase | 20-130 | 100-600 | Alp or alkaline phosphate |
| Amylase | up to 120 | Amyl | |
Measurement is carried out in medical units per liter (U/L).
Types of blood sugar tests.
A standard laboratory blood test will help determine with high probability the presence or absence of diabetes mellitus in a person. To carry it out, material can be collected from a vein or finger. Patients can measure their glucose levels at home using a glucometer. This blood test is called the rapid method. But this test does not always provide reliable information about sugar content. The error in the results provided by the glucometer sometimes reaches 20%.
With exercise or glucose tolerance test. If a standard laboratory test shows that your sugar levels are normal, it is recommended to undergo a glucose tolerance test to ensure that you are not predisposed to diabetes. The load test is carried out in two stages. First, venous blood is taken from a person on an empty stomach, and then he is given sweet water with sugar to drink (75-100 g of glucose is diluted in 250-300 ml of liquid). Then, over the course of 2 hours, material for examination is taken from the finger every 0.5 hour. After 2 hours, the last blood sample is taken.
Glycated hemoglobin.
A hemoglobin A1C test is prescribed to confirm diabetes and monitor the effectiveness of insulin treatment. Glycated hemoglobin is a red pigment in the blood that irreversibly combines with glucose molecules. Its content in plasma increases along with an increase in sugar in it. A glycated blood sugar test reveals the average glucose level over a period of up to 3 months.
General urine analysis
The results of a laboratory urine test primarily inform about the health of the urinary system. Only a doctor can correctly decipher a urine test (general clinical), taking into account all the parameters that depend on each other. Using the table, you can only compare the results obtained with standard values.

A container for OAM can be purchased at any pharmacy
During the analysis, physicochemical characteristics, organoleptic properties, and urine sediment are assessed, including:
- blood cells;
- unclassified and classified elements (cylinders);
- foreign impurities (mucus, bacteria, salts, yeast, epithelial cells).
All analyzed parameters are specified in the study form. However, normally some of them should not be present in the urine. Unfound elements are denoted by English “Neg” or Russian – “negative”.
Physico-chemical characteristics
| Indicator name | Reference values | Abbreviation for the designation on the form |
| acidity | 4–7 units. | RN |
| protein | Neg or not more than 0.033 g/l | PRO |
| sugar (glucose) | ≤ 0.8 mmol/l | G.L.U. |
| hemoglobin | Neg | NV |
| ketone bodies | Neg | KET |
| bilirubin | Neg | BIL |
| urobilinogen | 5-10 mg/l | URO |
Urine sediment
| Elements | Norm | Abbreviation for the designation on the form |
| red blood cells | men - 1-2 women - ≤ 3 | BLD or RBC |
| leukocytes | male -≤ 3; women-≤ 6 | LEU |
| classified hyaline casts | no more than 20 | HYAL |
| unclassified casts (erythrocyte, granular, epithelial, waxy) | Neg | UNCC |
| bacteria | Neg | NIT or BACT |
| yeast fungi | Neg | BYST |
| slime | slightly or Neg | MUCS |
| bladder epithelium | Neg | VTC |
Organoleptics
| Study parameter | Norm | Abbreviation for the designation on the form |
| color | straw | COLOR |
| density (specific gravity) | 1.010–1.022 g/l | S.G. |
| transparency | close to absolute | TURB – if there is turbidity |
| smell | unsharp | — |
| foaminess | absent | — |
Additional designations: accumulation of leukocytes (leukocyturia) - WBCC, squamous epithelium - SQEP, ascorbic acid - VC.
Results
The patient receives the results of laboratory tests of blood and urine on a special form, where the study parameters are indicated by a Latin (English) abbreviation. Each indicator has its own level of content in the blood or urine.
Only a doctor can correctly decipher the results of the study, since all parameters are correlated with each other. The patient can only compare his results with reference values. The standards to be followed are usually indicated in the analysis form.
Lipid profile and total cholesterol
A lipidogram is an extended biochemical blood test, including the lipid spectrum and reflecting the content of total cholesterol, high and low density lipoproteins, as well as triglycerides. In addition, this analysis determines the ratio of these indicators. One of the main indicators of the lipid profile is total cholesterol. It reflects the total content of a substance such as sterol in the blood.
Cholesterol is a fat-like alcohol that is insoluble in water. There are 2 sources of cholesterol in the human body: exogenous, which is caused by the consumption of fatty foods, and endogenous - the body produces cholesterol on its own. With certain metabolic disorders, cholesterol formation occurs faster than usual. This leads to an increase in its level in the blood.
Total cholesterol is denoted in Latin - CHOL. According to the current recommendations of the World Health Organization, the following indicators have been adopted to assess the level of total cholesterol in the blood:
- less than 5.15 mmol/l – optimal;
- 5.15 to 6.18 mmol/l – borderline;
- more than 6.2 mmol/l – high value.
An increase in these indicators indicates not only metabolic disorders, but also the development of certain diseases. Pathology is considered to be both an increase and a decrease in these indicators.
The reason for the increase in total cholesterol, or hypercholesterolemia, is observed in the following pathologies and conditions:
- excessive dietary intake of saturated fats;
- blockage of the bile ducts;
- cardiac ischemia;
- hypothyroidism;
- diabetes;
- gout;
- liver diseases;
- family predisposition to hypercholesterolemia;
- lack of somatotropic hormone.
No ads 1
If during pregnancy a woman was found to have a slight increase in total cholesterol, then there is no need to worry, since this is regarded as normal. A similar result can result from donating blood while taking certain medications from the group of diuretics and androgens, as well as cyclosporine, amiodarone, and ergocalciferol.
Hypocholesterolemia, or a decrease in total cholesterol, may occur when a patient has a blood test after a long fast or while on a diet low in saturated fat. A decrease in this indicator may also indicate malabsorption syndrome, liver necrosis, hyperthyroidism, megaloblastic anemia, and rheumatism.
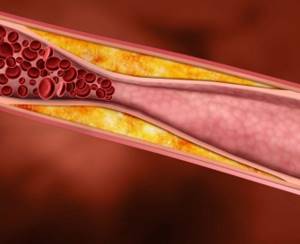
Total cholesterol levels reflect the risk of atherosclerotic plaque formation
Hypocholesterolemia may occur in patients with extensive burns, severe infection, or mental retardation. If there is a hereditary disorder of hemoglobin synthesis, the cholesterol level will also be reduced.
[node:field_similarlink]