When preparing for a hormonal examination, not all patients know what thyroglobulin is. This is a prohormone, a protein from which the thyroid gland synthesizes hormones. Its concentration indicates the presence of organic changes in the thyroid gland, relapses of malignant tumors. The thyroglobulin test has an independent diagnostic value. But to assess the condition of the thyroid gland, the results are interpreted in combination with tests for triiodothyronine (T3), tetraiodothyronine (T4) and thyrotropin (TSH).
What are triglycerides?
Triglycerides (abbr. TG) or triacylglycerides (abbr. TAG) are complex compounds (esters) of glycerol (trihydric alcohol) and fatty acids (also, as a rule, three - hence the prefix “THREE”). They are a priority “capacity” for the accumulation of fatty acids that are important for the body, as well as one of the most important sources of energy for humans (representing an alternative / “safety” version of glucose, i.e. when its reserves are depleted).
Triglycerides (fats) are very important for our health (having many vital/essential properties), but in excess they are harmful! Increasing the risks of developing cardiovascular diseases, atherosclerosis
, pancreatitis, diabetes, fatty liver and hypertension. However, their reduced level is considered no less alarming, indicating other problems with our health (more on this later in this article).
Triglycerides - macro photography
One of the main reasons for elevated levels of triglycerides in the blood is a large number of unspent calories (so-called “energy” units), which our body stores in the form of TG (as an “energy” reserve for the future). Thus, if you eat too much high-calorie/fatty foods and lead a sedentary/active lifestyle, this will certainly lead to an increase in the amount of “extra” (unclaimed) triglycerides!
Triacylglycerides are “transported” in the blood, being part of very low density lipoproteins (VLDL) or chylomicrons (CM). The main function of the latter is the transfer of dietary (i.e. food) triglycerides / exogenous fats (coming to us with food) from the small intestine (where they are absorbed) into the bloodstream (via lymphatic vessels). However, a much larger amount of TG, nevertheless, does not come to us with food, but is synthesized in the liver (these are endogenous fats), from where, in the protein shell of VLDL, they “go” to the cells along the highways of the circulatory system.
What is thyroglobulin and what is it responsible for?
Thyroglobulin (TG) is a protein that is synthesized by thyroid cells. It is involved in the production of iodine-containing hormones - T3 and T4. The TG molecule contains about 120 residues of the α-amino acid tyrosine, so it forms up to 6 molecules of tri- or tetraiodothyronine.
Elevated thyroglobulin indicates hyperactivity of thyrocytes - the thyroid cells that produce it. The synthesis of thyroid hormones from protein occurs according to the following principle:
- the TG molecule is cleaved by proteolytic enzymes, which are secreted by lysosomes;
- molecules T3 and T4 are formed in the cytoplasm of thyroid cells;
- synthesized hormones penetrate through the cell membrane into surrounding tissues and the systemic bloodstream.
The rate of thyroglobulin production is influenced by thyrotropin, a hormone produced by the adenohypophysis. With an increased level of TSH, the secretory activity of the thyroid gland increases, which also affects the content of the prohormone T3 and T4.
In a healthy body, thyroglobulin does not enter the bloodstream in an undigested form.
The biosynthesis of thyroglobulin is influenced by:
- volume of differentiated thyroid tissue;
- organic damage to the thyroid gland (trauma, inflammation, biopsy);
- increased levels of human chorionic gonadotropin (occurs in pregnant women).
Regardless of the cause, elevated TG levels are a sign of thyroid dysfunction. In most cases, the disorders are benign. But sometimes an increased level of a specific protein in the blood indicates the presence of adenocarcinoma in the organ - papillary or follicular. The thyroid gland is the only source of prohormones T3 and T4. But malignant tumors formed in the organ also begin to synthesize thyroglobulin.

Thyroglobulin analysis is the most accurate prognostic marker for thyroid cancer. Its increased concentration indicates malignancy of the gland cells.
Patients undergoing treatment for adenocarcinoma are periodically tested for thyroglobulin. An increased concentration of prohormone indicates the ineffectiveness of therapy, and this is the basis for surgery or radiotherapy. According to statistics, relapses of thyroid cancer occur in 15% of patients, so the TG test is a mandatory laboratory method for diagnosing recurrent tumors.
Why do TG levels matter to doctors?
For doctors, triglycerides (TG) in the blood serum are an indicator of fat (lipid) metabolism, which is extremely necessary (most often) for diagnosing hypertriglyceridemia and other disorders of fat metabolism (lipid metabolism / dyslipoproteinemia). As well as assessing the risks of developing coronary heart disease (CHD), atherosclerosis (in particular, atherosclerotic lesions of the coronary vessels or cerebral vessels).
Plus, determination of triglyceride levels by doctors is used for accurate classification of hyperlipoproteinemia (i.e. for pheno/typing of lipoproteins) and, accordingly, prescribing adequate treatment (for each pheno/type separately). And also in the diagnosis of obesity, hypertension (high blood pressure), diabetes and pancreatitis. For example, an increased TG content - over 11.2 mmol/l - directly indicates to treating specialists an increased risk of complications of acute pancreatitis.

As a rule, the detection of the amount of triglycerides in the blood (using a lipid profile ) is carried out simultaneously with the determination of other (no less important) indicators of lipid metabolism: total cholesterol (TC), LDL ( low density lipoproteins / “bad” cholesterol) and HDL ( lipoproteins high density /good cholesterol). As a rule, laboratory staff immediately calculates the atherogenicity coefficient (index) . You may have a question: why is one of them good and the other bad? We answer immediately - in a way that is easy to understand.
Conventionally, “bad” cholesterol is called LDL (LDL) cholesterol due to the fact that its excess levels contribute to the formation of cholesterol/atherosclerotic plaques (inside the walls of blood vessels / SEE VIDEO AT THE BOTTOM OF THE PAGE - 43 sec
). Which narrow the gaps, interfere with normal blood flow, or can even clog them (over time and without treatment), which can lead to a stroke or heart attack. That is why HDL (HDL) cholesterol is considered “good” - because it takes the excess of the first “prankster fellow” and “transports” them back to the liver (for processing and removal from the body).
What is dangerous about changes in thyroglobulin levels?
An increase in thyroglobulin is a pathological condition that occurs when the endocrine system malfunctions. If the test results exceed the reference values, this often indicates malignant processes in the thyroid gland:
- Papillary cancer is a common form of adenocarcinoma, which is detected in 85% of cases of all gland tumors. In 30% of patients, regional lymph nodes are involved in the malignant process. With late diagnosis and treatment, metastases are detected in the lungs and bone tissue.
- Follicular cancer is an aggressive, low-quality thyroid tumor that is prone to metastasis to internal organs. More often diagnosed in women and children, they are characterized by the growth of cancerous tissue into the blood vessels in the neck area.
Elevated thyroglobulin values indicate structural changes in the thyroid gland. Because of this, the protein enters the blood undigested. It is recognized by the immune system as an antigen, so antibodies are synthesized against TG. This causes autoimmune inflammation of the gland - Hashimoto's thyroiditis.
Most patients with benign tumors in the thyroid gland exhibit increased concentrations of thyroglobulin. Such results are obtained in acute iodine deficiency, which is dangerous due to thyroid pathology. It manifests itself with the following symptoms:
- memory impairment;
- difficulty swallowing;
- fast fatiguability;
- hair fragility, etc.
Changes in TG levels are fraught with nodular goiter. A decrease in thyroglobulin during pregnancy is dangerous for the thyroid gland of the mother and fetus. Endocrine pathologies in the early stages often lead to spontaneous abortion and hypothyroidism in newborns.

A decrease in TG due to iodine deficiency during pregnancy leads to a severe complication in the child - neurological cretinism.
Triglycerides and cholesterol - what are the differences and similarities?
Despite the fact that both cholesterol and triglycerides, in essence, are the same lipids (i.e. fats/fat-like substances), their functions are completely different. Although, they are EQUALLY vital/important for us! The main tasks of cholesterol (CS) are to participate in the production of vitamin D, adrenal hormones, sex hormones, as well as ensuring the normal functioning of the brain and immune system (including reliable protection against cancer). In addition, cholesterol forms the sheaths of nerve fibers and is the “protective frame” of the cell membrane. The main task of triglycerides (TG) is to provide our body (partly “built” by the above/mentioned cholesterol) with energy (by burning calories from the “reserve”). That is, to give us the opportunity to live, and when necessary, to effectively “fight for survival.”
Norm of triglycerides in the blood (in mmol/l and mg/dl)
Reference values (i.e., the normal level of triglycerides in the blood of adults) range from 0.5 to 2.2 mmol/l (from 55 to 195 mg/dl according to the standards of the USA, Germany, Israel and France). You can find other values and, accordingly, risk groups below in the table (based on data from the Mayo Clinic). And just below, after detailed tables (for men and women by age), you will learn about what is indicated - both high and low triglyceride levels (for both men and women - sometimes separately).
| (mmol/L) | (MG/DL) | What does it mean? | Reasons for deviations |
| below 0.3 | less than 26.5 | / very low level / | exhaustion of the body after a long fast or at high risks of ischemic stroke / cerebral infarction in the elderly |
| 0.3 – 0.49 | 26.5 – 43.7 | / low level / | unhealthy diets, side effects from medications, some types of developing diseases |
| 0.5 – 1.0 | 44.3 – 88.5 | / borderline reduced (acceptable) level / | |
| 1.1 – 1.7 | 97.4 – 150.5 | / normal level (for adults not of retirement age) / | |
| 1.8 – 2.2 | 159.0 – 194.7 | / borderline elevated (acceptable) level / | |
| 2.3 – 5.6 | 203.5 – 495.6 | / high level / | there is a high probability of developing cardiovascular diseases, type II diabetes, acute pancreatitis, and “fatty” liver |
| from 5.7 and above | from 500 or more | / very high level / | increased risks of dangerous complications of acute pancreatitis |
Recommendation 63
- Patients with low and average risk who have undergone surgical removal of the thyroid gland or adjuvant therapy, who do not have evidence of disease progression based on the results of ultrasound examination of the neck area, need to determine thyroglobulin (TG) during the period of 6-18 months during Levothyroxine therapy using sensitive methods (<0.2 ng/ml) or after TG stimulation to confirm the absence of disease progression.
(Strong recommendation, moderate quality of evidence)
- Repeating the TG stimulation test is not recommended for low- and intermediate-risk patients with an excellent response to therapy.
(Weak recommendation, low quality of evidence)
- A TG stimulation test may be performed in patients with an indeterminate, biochemically incomplete or structurally incomplete response to treatment, in patients with a spontaneous decrease in TG values on thyroid hormone therapy over a long period of time in order to review/reassess the response to therapy.
(Weak recommendation, low quality of evidence)
- In the future, a stimulation test is not required for patients without signs of the disease, because the benefit of its use in this population is small. The use of sensitive methods for determining serum TG helps to avoid the use of this test in low-risk patients on Levothyroxine therapy with TG levels below 0.1-0.2 ng/ml.
Serum TG measurement and clinical utility
- Determination of serum TG levels is an important method for monitoring patients with residual or recurrent disease.
- Most laboratories now use immunometric methods to measure serum TG levels, it is important to note that these methods are calibrated against international standards (CRM-457).
- Despite improvements in the standardization of TG analysis methods, there are often still differences between the results of different methods. This led to the recommendation that patient measurements should be performed using the same method.
- Variability in methods for measuring TG Ab levels can lead to false-negative antibody levels, which in turn leads to undetectable TG in serum.
- However, radioimmunological methods for measuring TG are not widely used and are less sensitive to the influence of antibodies than immunometric methods.
Most of the data are from studies using 1 ng/mL functional sensitivity methods. The functional sensitivity of many modern methods is ≤0.1 ng/ml. High sensitivity ensures reliable measurement of TG in patients on thyroid hormone therapy, even compared to the stimulation test.
- Since TSH stimulation increases basal serum TG by 5-10-fold, significant serum TG levels (>1-2 ng/ml) detected after stimulation using a method with a functional sensitivity of 0.5-1 ng/ml may be predicted in patients on Levothyroxine therapy without stimulation, using a highly sensitive method for measuring TG, provided that the TG level is above 0.2 ng/ml.
The highest degrees of sensitivity of serum TG were observed with the abolition of thyroid hormones or with stimulation using recombinant human thyrotropin. Serum TG measurements obtained during TSH suppression may be insufficient in identifying patients with relatively small amounts of residual tumor.
- Residual tumor tissue is often located in the neck, and ultrasound examination in such patients has great diagnostic value for recognizing or excluding neoplastic processes, even if it is impossible to determine serum TG.
- Conversely, even measurement of TG levels during TSH stimulation may be unreliable for patients with a clinically noticeable tumor due to the presence of antibodies to TG or, less commonly, due to insufficient production and secretion of immunoreactive TG by tumor cells.
- The TG level should be assessed in light of the likelihood of detecting clinically significant residual tumor.
- An aggressive and poorly differentiated tumor may be present even despite low basal or stimulated TG levels; in contrast, minimal increases in TG after stimulation may be observed in patients at low risk of clinically significant disease progression.
- However, a stimulated serum TG level of <0.5-1.0 ng/ml in the absence of anti-TG antibodies provides a 98%-99.5% probability of developing remission.
- Measurement of stimulated TG does not require a repeat test in most cases; detection of an undetectably low basal serum TG and absence of signs of disease progression according to ultrasound is sufficient. However, 0.5% to 0.3% of patients may experience clinical or biochemical relapse despite stimulated TG levels <0.5 ng/mL.
Initial follow-up of low-risk patients (approximately 85% of postoperative patients) undergoing total or subtotal thyroidectomy and radioiodine treatment should be based primarily on stimulated TG and neck ultrasound.
- However, a TG method with a functional sensitivity of 0.1–0.2 ng/mL may reduce the need for stimulation testing. In one study using this method: serum TG levels on Levothyroxine <0.1 ng/ml were rarely (2%) associated with an increase in stimulated TG >2 ng/ml;
- however, 42% of patients had a basal TG level with TSH suppression >0.1 ng/mL, but only one patient had residual tumor.
- Annual determination of serum TG levels during levothyroxine therapy with periodic ultrasound examination of the neck are sufficient methods to detect relapse without further need for stimulated TG testing in patients with serum TG <0.2-0.3 ng/ml on thyroid hormone therapy.
Approximately 20% of patients in remission with a serum TG level <1 ng/ml while receiving suppressive doses of levothyroxine have a stimulated TG level >2 ng/ml 12 months after surgery or radioactive iodine therapy.
- In this cohort of patients: in 1/3 with a persistent course or relapse of the disease, an increase in the level of serum TG is detected,
- and in 2/3 – without progression of the disease, the level of stimulated serum TG is stable or gradually decreasing
- It appears that stimulated TG levels above 2 ng/mL are highly sensitive for identifying patients with persistent tumors.
[C7] AT to TG
- The presence of anti-TG antibodies, which is found in approximately 25% of those with thyroid cancer and 10% of the general population, will underestimate serum TG levels when measured by immunometric methods.
- Serum antibodies to TG should be measured in combination with serum TG by an immunometric method.
- Although standardization of International Reference Preparation 65/93 methods has been recommended, wide-ranging differences in the results of different methods and their analytical sensitivities remain.
- Anti-TG antibodies may increase transiently after surgery due to an apparent immune reaction to the operation itself, and may also increase after ablative therapy.
- Anti-TG antibodies should be measured repeatedly if routine anti-TG antibody testing is negative in patients with surgically confirmed Hashimoto's thyroiditis. This may be useful when measuring anti-TG antibodies immediately after thyroidectomy and before ablation, as high levels may predict the likelihood of relapse in patients without Hashimoto's thyroiditis.
- Decreasing levels of antibodies to TG may indicate successful therapy.
The recent development of liquid chromatography-coupled mass spectrometry TG assays promises to be a more accurate method for measuring TG in the presence of anti-TG antibodies, but future studies will need to first validate this method in terms of functional sensitivity, correlation with immunoassays, and patient outcomes.
[R8] What is the role of TG measurement in patients not treated with radioactive iodine?
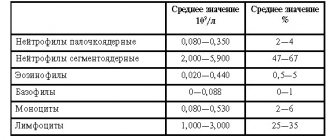
Triglycerides are normal in men (table by age)
Below is a detailed table: the norms of triglycerides (TAG / TG) in the blood in men (by age) / in young men and boys (i.e. in adolescents and young children). Units of measurement: mmol/l and mg/dl.
| AGE | (mmol/L) | (MG/DL) |
| up to 10 years | 0.35 — 1.14 | 31.0 — 100.9 |
| 10-15 | 0.37 — 1.42 | 32.7 — 125.7 |
| 15-20 | 0.46 — 1.82 | 40.7 — 161.0 |
| 20-25 | 0.51 — 2.28 | 45.1 — 201.8 |
| 25-30 | 0.53 — 2.82 | 46.9 — 249.6 |
| 30-35 | 0.57 — 3.02 | 50.4 — 267.3 |
| 35-40 | 0.62 — 3.63 | 54.9 — 321.2 |
| 40-45 | 0.63 — 3.62 | 55.7 — 320.3 |
| 45-50 | 0.66 — 3.71 | 58.4 — 328.3 |
| 50-55 | 0.66 — 3.62 | 58.4 — 320.3 |
| 55-60 | 0.66 — 3.24 | 58.4 — 286.7 |
| 60-65 | 0.66 — 3.30 | 58.4 — 292.0 |
| 65-70 years | 0.63 — 2.95 | 55.8 — 261.0 |
Triglycerides are normal in women (table by age)
We bring to your attention a table: the norms of triglycerides (TAG / TG) in the blood of women (by age) / in girls and young women (i.e. in small children or adolescents). Units of measurement: mmol/l and mg/dl.
| AGE | (mmol/L) | (MG/DL) |
| up to 10 years | 0.41 — 1.25 | 36.3 — 110.6 |
| 10-15 | 0.42 — 1.49 | 37.2 — 131.9 |
| 15-20 | 0.41 — 1.54 | 36.3 — 136.3 |
| 20-25 | 0.42 — 1.49 | 37.2 — 131.9 |
| 25-30 | 0.43 — 1.64 | 38.0 — 145.1 |
| 30-35 | 0.45 — 1.71 | 39.8 — 151.3 |
| 35-40 | 0.46 — 2.00 | 40.7 — 177.0 |
| 40-45 | 0.52 — 2.17 | 46.0 — 192.0 |
| 45-50 | 0.53 — 2.43 | 46.9 — 215.0 |
| 50-55 | 0.60 — 2.64 | 53.1 — 233.6 |
| 55-60 | 0.63 — 2.97 | 55.7 — 262.8 |
| 60-65 | 0.64 — 2.71 | 56.6 — 239.8 |
| 65-70 years | 0.69 — 2.72 | 61.0 — 240.7 |
Triglycerides (TG) - below normal
What do low triglyceride (TG) levels in the blood mean in women and men? This condition may be caused by simple malnutrition (for example, due to “harmful” diets) or as a side effect after taking certain medications. Even from ascorbic acid (i.e. vitamin C - in large dosages). Also, low triglycerides in a biochemical blood test can be observed in people suffering from hyperthyroidism, COPD (chronic obstructive pulmonary disease), malabsorption syndrome, and hyperparathyroidism. Other reasons for their low levels in the blood serum are recent (surgery), trauma, burns or radiation therapy. Critically low levels “warn” about cerebral infarction.
(Follow the link) in more detail about LOW TRIGLYCERIDES IN THE BLOOD (WHAT DOES THIS MEAN?)
Analysis for thyroglobulin: indications, norms and rules for delivery
Early diagnosis of relapses and metastases of malignant thyroid tumors is the main goal of taking the TG test. Periodically, blood tests are done in patients who have undergone surgery or radiotherapy for adenocarcinoma.
Indications for laboratory testing:
- suspicion of thyroid cancer;
- preventive diagnosis of carcinoma;
- assessment of the functional state of the thyroid gland after surgery;
- identifying the causes of insufficient production of thyroid hormones;
- determination of the level of antibodies to TG in patients with autoimmune thyroiditis;
- signs of artificial thyrotoxicosis;
- suspicion of endemic goiter in pregnant women;
- monitoring the effectiveness of treatment during radioactive iodine therapy;
- determination of the severity of iodine deficiency conditions;
- symptoms of thyroid inflammation.
To determine the concentration of thyroglobulin, a biochemical blood test is performed, which is taken from the ulnar vein.
The level of prohormone depends on many factors, the influence of which leads to false positive or false negative results. To avoid errors, you need to:
- take venous blood on an empty stomach only in the morning before 11-00;
- postpone diagnosis for 1.5 months after surgery to remove adenocarcinoma;
- within 24 hours, refuse to undergo other instrumental examinations - MRI, ultrasound, CT;
- refrain from smoking, excessive emotional and physical stress 30 minutes before the examination.

An increased concentration of prohormone in the blood indicates relapse of tumors, sluggish or autoimmune thyroiditis. The frequency of the study is determined by the endocrinologist or oncologist:
- after thyroidectomy – after 6 or 12 months;
- with a low probability of relapse of adenocarcinoma - every year;
- with a high risk of exacerbation of cancer - every six months.
An increased concentration of thyroglobulin in patients with adenocarcinoma indicates relapse of the oncological disease. The test results are affected by:
- exacerbation of cytomegalovirus infection;
- parasites in the blood;
- increased level of antibodies to thyroglobulin;
- production of defective thyroglobulin by carcinomas;
- relapses of monocytic tonsillitis.
To minimize errors in the results, a TSH-stimulated TG (TSG) provocative test is performed before the examination. According to practical observations, the sensitivity of TG analysis increases after this test.
The thyroglobulin norm is in the range of 1.4-78 ng/ml. Threshold values largely depend on:
- analysis conditions;
- reagents used;
- sensitivity of the equipment of a particular laboratory.
Therefore, the results obtained are compared with the accepted normal indicators, which are indicated on the form.

Elevated thyroglobulin is detected in many women during pregnancy and immediately after childbirth. But this does not indicate disturbances in the functioning of the thyroid gland or tumor diseases.
Triglycerides (TG) - above normal
High triglycerides (TG) in the blood lipid profile can indicate to doctors the risks of diseases such as atherosclerosis, diabetes mellitus, pancreatitis (chronic or acute / for complications of AP), “fatty liver”, liver cirrhosis, hypertension, coronary heart disease (coronary artery disease) , renal failure (chronic). They also directly indicate a previous myocardial infarction, increased risks of developing cerebral thrombosis, obesity, and gout. In addition, TG levels (much higher than normal) can be observed in people suffering from alcoholism.
We recommend checking out (links below):
- high TG levels - what does this mean, what are the reasons for the increase?
- how to quickly and effectively reduce TG levels in the blood? (detailed material)
- medications that increase cholesterol and triglyceride levels in the blood
- medications (tablets, capsules, injections) to reduce their concentration in the blood
It is definitely worth noting that elevated triglyceride values can be detected specifically in women during pregnancy, during menopause (menopause), after taking birth control pills, or during hormonal therapy (especially while taking oral estrogens). And finally, they point to a purely female disease - PCOS (polycystic ovary syndrome).
Also read about WHAT DO HIGH TRIGLYCERIDES MEAN FOR WOMEN?
Causes and symptoms of changes in the level of thyroglobulin in the blood
Low or high levels of thyroglobulin occur in most patients with thyroid dysfunction. But it is impossible to determine the type of disease based on the content of prohormone T3 and T4. To clarify the diagnosis, patients are referred for further examination. To confirm oncology, a chest x-ray, MRI, ultrasound or CT is prescribed.
Increased concentration
If thyroglobulin is elevated in patients with previously diagnosed adenocarcinoma, this indicates an exacerbation of cancer. In this case, there is a direct relationship between the concentration of TG and the size of malignant neoplasms. In patients of other groups, elevated thyroglobulin indicates:
- subacute thyroiditis;
- hyperthyroidism;
- endemic goiter;
- Hashimoto's syndrome;
- iodine deficiency conditions;
- tumors in the adenohypophysis;
- Graves' disease;
- nodular toxic goiter;
- benign adenoma.
Sometimes elevated thyroglobulin levels are caused by hormonal therapy or radioactive iodine. High TG is found in men and women who have undergone ethanol sclerotherapy for cystic nodular formations in the gland.

Most therapeutic and diagnostic procedures that affect thyrocytes lead to an increase in serum TG concentrations.
Elevated thyroglobulin during the treatment of cancer indicates the need to adjust the treatment regimen, increase the dose of chemotherapy, etc. Only a specialist can understand the test results. Sometimes an imbalance of T3 and T4 caused by pathologies of the adenohypophysis also affects the TG content.
Decreased concentration
A drop in TG in patients with adenocarcinoma in the thyroid gland indicates the effectiveness of treatment and the absence of secondary neoplasms. But even if thyroglobulin is lowered, this does not indicate complete recovery. Other reasons for a decrease in TG in the blood include:
- inhibition of secretory activity of the thyroid gland;
- errors when collecting biomaterial for analysis;
- congenital anomalies of the thyroid gland;
- chronic stress;
- iodine deficiency;
- exacerbation of toxoplasmosis or mononucleosis.
Biochemical analysis is carried out in combination with a test for antibodies (AT) to thyroglobulin. An increased level of AT indicates the autoimmune nature of the thyroid disease. Manifestations of pathology include:
- thickening of the thyroid gland;
- moderate pain in the throat area;
- labored breathing;
- reduction or enlargement of the thyroid lobes.
Symptoms of endocrine diseases increase slowly, so patients do not rush to see a doctor. The reasons for contacting an endocrinologist are:
- problems with conception;
- depression;
- difficulty falling asleep;
- menstrual irregularities;
- decreased libido, etc.
Most endocrine diseases are polysymptomatic, that is, thyroid dysfunction affects the functioning of many internal organs and systems.
It is recommended to undergo a preventive examination if close relatives suffered from autoimmune or oncological pathologies.
Prevention of triglyceride (TG) levels
"Forewarned is forearmed!" or “Beware of troubles while they are gone,” our ancient ancestors teach us. Therefore, instead of “heroically” solving problems with excessively high levels of triglycerides (or low ones) in the future, isn’t it better to immediately protect yourself with competent prevention? Likewise, it’s not particularly wise to step on the same rake twice. That is, having been healed of diseases, one again returns to the “old ruts”, provoking their re-development.

Prevention of normal levels: healthy lifestyle and proper nutrition. Moderate physical activity + control of calories, weight and waist size.
So, how can you protect yourself from the negative effects of “abnormal” triglycerides in the blood? How to keep your health strong for many years? Which means positivity and vitality!
- Do not get carried away with alcoholic beverages (especially beer and wines)!
- Limit the amount of sweet and starchy foods in your diet (and eliminate “store-bought” ones altogether). Instead of “sugary” pastries and cakes, love with all your heart: fresh (sour) fruits, berries (priority: strawberries and blueberries), as well as low-fat yoghurts (from trusted manufacturers).
- Eat exactly - sour fruits, i.e. not loaded with fructose (for example, DO NOT eat a lot of grapes, bananas, melons and peaches). “Lean on” green apples, tangerines and oranges. If you really want sweet fruits, then in quantities of no more than 100 grams. per day.
- Make it a rule (especially if you are over 50): eat fatty sea fish 2 times a week. Which will not only protect you from high triglycerides, but will also reduce the risk of developing cardiovascular diseases by at least 30%!
- Actively develop your own culinary skills, using not only proven products (without harmful “store-bought” additives to increase shelf life), but also healthy “tools” for their preparation. Those. “oven”, grill steamer (with grate) or frying pan (with ANTI/stick coating).
- When preparing homemade meals or dressing salads, buy only the best vegetable oils. Health is more important than anything! The ideal option is olive oil. Eliminate margarines, lard and butter. Beware of products (especially store-bought ones) that contain palm oil!
- Significantly reduce your consumption of meat products such as smoked sausage, bacon, brisket, and sausages or wieners with a high pork content. After all, it’s not for nothing that God considers pork “unclean.” The best option is doctor's sausage! No wonder it's called that!?
- Properly balance the amount of protein in your daily menu. Alternating the amount of animal proteins recommended by doctors with plant proteins (legumes/beans, soy and tofu).
- Try to eat more vegetables (plus wholemeal products), thereby providing your body with enough FIBER. Just drink plenty of water (clean/room temperature).