The mechanism of appearance of plasma cells
The function of plasma cells is protective
Unlike other immune cells, plasma cells are not constantly present in the blood. They are contained mainly in lymphatic tissues, spleen and bone marrow, leaving their shelters only in case of danger to the body. Their main function is the production of antibodies.
The mechanism of appearance occurs as follows:
- immune cells send a signal to the brain that pathogenic organisms of a certain type have invaded;
- the brain sends a signal to B lymphocytes with information about which particular virus or bacterium has penetrated;
- B lymphocytes move to the lymph nodes, where they transform into plasmocytes (plasma cells) to fight a specific pathogen;
- Plasmocytes begin to develop an immune response, forming several thousand molecules of protein compounds—antibodies—in a second.
During the transformation of B lymphocytes, some of the newly formed cells become so-called memory cells. They live for decades in the bone marrow, carrying antibodies against every bacteria or virus. Plasmocytes die within a few days after their birth.
Causes of plasma cells in blood tests

Infection of the body can lead to the appearance of plasma cells
Thus, plasma cells appear in the bloodstream only when it is necessary to produce antibodies. In the absence of a pathogenic factor, there is no need for plasma cells. If transformed B lymphocytes are found in a blood sample, then an infection is present in the body, or has been present in the recent past.
Factors that provoke the formation of plasma cells:
- flu,
- ORZ,
- ARVI,
- bacterial infection
- infectious diseases,
- mononucleosis,
- tuberculosis,
- dysbacteriosis,
- pathologies of an autoimmune nature,
- oncological tissue lesions.
When is the presence of plasma cells normal?

Plasmocytes may circulate for some time after infection
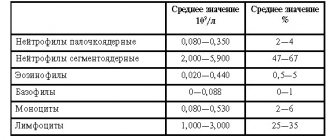
In a healthy adult, plasma cells should not be present in the bloodstream. They can appear in a ratio of 1-2 per 1000 leukocytes, so they are most often not detected when diagnosing a blood sample.
After the disease, transformed cells continue to circulate in the plasma for some time. Therefore, if plasma cells are detected, it is necessary to retake the test after a few days.
For children, the presence of a small percentage of plasma cells is normal. From the 5th day of life until the end of puberty, the blood may contain from 0.25 to 0.5% plasma cells. The percentage is calculated in relation to the total number of leukocytes.
What analysis is it determined by?
In the case when a person feels unwell and clinical signs of a cold appear, a simple blood test , taken from a finger, is sufficient. To do this, a small puncture is made in the ring finger, after which blood is drawn onto a glass slide using a capillary. Next, the resulting sample is examined under a microscope, where the total number of blood cells is assessed, as well as the presence or absence of plasma cells. In cases where additional diagnostics are required, blood is taken from a vein and the exact number of plasma cells is detected using PCR or other reactions. Most often, a blood test from a finger prick is sufficient. The second diagnostic method is used when a person does not experience any symptoms, but the plasma cell count remains high.
Plasmocyte detection test

The plasma cell test requires minimal preparation
The doctor may refer you for an analysis to detect plasma cells if the patient is concerned about various ailments: aching joints, lethargy, causeless fatigue, low-grade fever, pain in the abdomen, swollen lymph nodes.
Plasmocytes are detected during a general blood test. Most often, a blood sample is taken from a finger, less often from a vein. Before blood collection, it is recommended not to eat for 8 hours.
If the analysis reveals the presence of plasma cells, it is necessary to undergo additional examinations to determine the cause. Only after this the doctor prescribes treatment.
Analysis indicators and diagnostics
The main reason for concern is only the increase in these elements in the blood. The decrease is not diagnosed. In a healthy body, plasma cells are in a kind of sleep mode. It is considered normal for a child and an adult to have only a few units. Approximately 1-2 out of 1000 total blood cells. In infants, this amount is slightly larger, approximately 10-20 units.
The most common diagnostic method is a clinical blood test. In laboratory conditions, various pathologies that a person presumably suffers from are identified. For this purpose, biomaterial is taken from both a finger and a vein, but capillary blood is much more suitable than venous blood. The first research method is considered simpler. To take tests, it is recommended to adhere to a number of rules:
- You can’t drink or eat in the morning, the last meal should be no later than eight o’clock in the evening of the previous day;
- drinking alcoholic beverages is prohibited during the last three days;
- on the day the material is submitted, it is advised not to smoke.
Attention! Doctors do not recommend taking tests if a person visited the gym in the morning. The functioning of the body changes after physical activity. Tests may give false results.
The result will be accurate if these rules are followed. If the numbers are very high or, conversely, low if you feel unwell, the doctor should prescribe a retake. Often the results increase even further. This means that the disease is progressing.
Factors influencing the result

Plasmocytes in a blood sample in children are not uncommon.
The presence of plasma cells in adults is a clear sign of a pathological process in the body. If the acute stage of the disease is not observed, the doctor may suspect a sluggish chronic infection, which may not manifest itself in any way externally. Subsequent research will reveal the factor that influenced the appearance of plasma cells.
In children, the immune system is just developing, encountering many viruses, fungi and bacteria. To create lasting immunity for life, white blood cells actively develop a response to every dangerous object. Plasmocytes can always be detected in a child’s blood sample. Therefore, the patient's age is one of the factors influencing the result.
An increase in the number of transformed cells is detected after vaccination. It is with the help of plasma cells and memory cells that an immune response is formed to virus particles introduced into the body, which allows the cells to fight back this virus in the future.
Diagnosis of multiple myeloma
The diagnosis is made by blood tests, where paraproteins are found and their total and type concentrations are determined. Paraproteins are designated as immunoglobulins - IgA, IgG and IgM. Plasmocytes produce immunoglobulins at their own discretion and in varying quantities; their changes in the production of pathological proteins subsequently assess the effectiveness of treatment and disease activity.
The degree of aggressiveness of plasma cells is determined by microscopy of the bone marrow; it is obtained from the sternum during a sternal puncture or during a biopsy of the pelvic bone. The study is especially relevant when the production of paraproteins is low or when the nature of the course of the disease changes.

A long-standing marker of the disease is Bence Jones protein in the urine, detected in 70% of patients. The protein is formed from chains of small molecular weight immunoglobulins A and G—“lungs”—that leak out of the kidney tubules. The Bence-Jones content also controls the course of the disease.
Often the disease is accidentally discovered during a routine chest x-ray based on lytic defects of the ribs. At the first stage, it is necessary to identify all destructive changes in the bones in order to further monitor the process and results of therapy, which is possible with highly sensitive low-dose CT of the entire skeleton.
MRI examines the condition of the flat bones - the skull and pelvis, which is necessary for smoldering and solitary tumors. MRI helps to evaluate not only bone defects, but also the presence of tumor infiltration of soft tissues and involvement of the spinal cord in the process.
A karyotype analysis is required to identify genetic abnormalities that affect the patient’s prognosis and the effectiveness of treatment.

Threat of presence of plasma cells
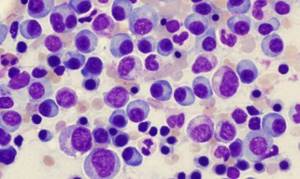
Blood smear from a patient with plasmacytoma
The presence of plasma cells in itself is a consequence of the inflammatory process in the body. If the pathogenic cause is eliminated, the cells will no longer circulate in the blood. However, under the influence of certain factors, plasma cells can form incorrectly and turn from friends of the immune system into its enemies.
This phenomenon is the most common concern of patients who receive a form about the content of plasma cells in the blood. The idea that all plasma cells pose a threat and are an indicator of oncological changes in the blood is erroneous. Such a failure at one of the stages of transformation of a B-lymphocyte into a plasma cell occurs in rare cases; a possible cause may be toxic damage to the body, exposure to radiation, or genetic disorders.
As a result of the failure, an atypical plasma cell appears, which, through continuous division, forms a plasmacytoma. The neoplasm is a malignant tumor of plasma cells and poses a danger to human life.
Biology and medicine
Plasma cells are microscopic factories, each of which produces huge quantities of antibodies ready to fight a strictly defined antigen.
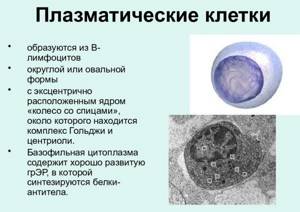
Plasmocytes, derived from B lymphocytes, are protein-synthesizing cells rich in ER elements, located near small blood vessels in the organs of the immune system, in the mucous membrane of the digestive and respiratory systems.
They produce antibodies (immunoglobulins), which determines their most important role in protecting the body.
Upon encountering and recognizing an antigen, B cells undergo characteristic ultrastructural changes, becoming lymphoblasts.
It goes like this. After stimulation by antigen, differentiating lymphoblasts appear in the germinal centers. The plasma cells formed from them are located in the medullary cords of lymphoid cells passing between the medullary sinuses.
The maturation of antibody-forming cells in areas remote from where antigenic stimulation occurred is also observed in the spleen (here plasma cells are detected mainly in the marginal zone).
Subsequently, many B lymphoblasts mature into antibody-producing cells (AFCs), which proliferate and differentiate into plasma cells in vivo. These form and release large quantities of receptor molecules in soluble form - antibodies.
Normally, plasma cells are found only in secondary lymphoid organs and tissues, and, in addition, they are quite numerous in the red bone marrow.
Antibodies produced by one plasma cell have the same antigen specificity and belong to the same immunoglobulin isotype.
Plasma cells: pathology
EPIGENETIC REGULATION OF PLASMA CELL DIFFERENTIATION
Treatment and prevention

Treatment is aimed at the cause that caused the appearance of plasma cells
Treatment consists of identifying and eliminating the cause that caused the appearance of plasma cells in the blood. Depending on the factors that provoked the formation of plasma cells, drugs are prescribed:
- antiviral,
- antibacterial,
- antibiotics,
- antihistamines,
- anthelmintics,
- vitamin complexes.
If a cluster of atypical plasma cells forms, radiation and chemotherapy, the use of glucocorticosteroids, and surgery may be required.
Preventive measures include a balanced diet, proper rest, and the absence of physical and emotional stress. An important component is the absence of untreated diseases, in order to avoid their development into chronic forms.