In blood analysis, MID denotes the combination of three formed elements included in the cellular composition of biological fluid: monocytes, eosinophils, basophils. The study and calculation of the number of MIDs is carried out as part of clinical hematology (general blood test).
CCA (general clinical analysis) is a laboratory method for determining the chemical composition and physical properties of blood. This is the most common study that allows us to identify violations of microbiological processes in the body. Clinical hematology is prescribed to adults and children of all ages:
- for medical reasons (diagnosis of diseases and monitoring of treatment);
- for preventive purposes (medical examinations, routine medical examination).
For the study, capillary blood is taken (from a finger). A transcript of the results is transferred to the attending physician, or the patient collects the results independently. The analysis takes into account the quantitative characteristics of various blood cells:
- ESR – erythrocyte sedimentation rate (ESR), indicating the ratio of plasma protein fractions;
- RBC – erythrocytes or red blood cells;
- Hb – hemoglobin (a complex protein component of blood);
- Hct – hematocrit (red blood cell volume);
- PLT – platelets (bone marrow blood platelets);
- RET – reticulocytes (young anucleate red blood cells).
Separately, the results of the leukogram (leukocyte formula) are displayed, which includes WBC - total leukocytes (colorless or white blood cells), and the components:
- NEU or NEUT – neutrophils (band and segmented)
- LYM – lymphocytes;
- MID triad, including: MON - monocytes, EOS - eosinophils, BAS - basophils.
The microscopy process is automated. The results are assessed using a comparative method of the patient’s indicators obtained and the accepted reference values. The advantages of general analysis lie in its accessibility, simplicity, information content, and efficiency of implementation in a laboratory setting.
Important! A complete blood count is an important diagnostic test that cannot be ignored. Based on its results, the doctor may suspect the presence of a serious pathology that requires immediate treatment.
General blood test - interpretation, norms
To decipher blood test indicators, it is not enough to know their normal values. It is also necessary to have an idea of how each indicator affects the properties of blood and under the influence of what factors it can take values below or above normal. Here are descriptions of the general blood test indicators:
- Red blood cells - perform the most important function, which is to deliver oxygen to the tissues of the body and remove carbon dioxide from them. Their reduced level indicates that the body does not receive enough oxygen. When the level of red blood cells exceeds the norm, there is a high risk of blood cell sticking together (thrombosis).
- The width of the distribution of red blood cells - this indicator determines the difference in size of red blood cells. When deciphering blood test results, a high distribution width can be detected if there are both small and large red blood cells in the blood. This may indicate anisocytosis (a sign of iron deficiency or other types of anemia).
- Red blood cell volume - information about the average size of red blood cells. A low volume of red blood cells may indicate iron deficiency or microcytic anemia, and an increased volume occurs when there is a lack of folic acid or vitamin B12 in the body (megaloblastic anemia).
- The content of hemoglobin in the erythrocyte - a reduced indicator may indicate iron deficiency anemia, an increased indicator may indicate megaloblastic anemia.
- The concentration of hemoglobin in the erythrocyte - a value below normal can occur with iron deficiency anemia or thalassemia (congenital blood disease). Exceeding the norm for this indicator is observed in extremely rare cases.
- The erythrocyte sedimentation rate allows us to indirectly estimate the protein content in the blood plasma. An excess of this parameter may indicate probable inflammatory processes in the body, malignant tumors and anemia, and a decrease indicates an increased content of red blood cells (rare).
- Hemoglobin is a protein responsible for transporting oxygen to tissues and organs. Its decrease indicates anemia (oxygen starvation). An increase in hemoglobin can occur when the body is dehydrated or has a high red blood cell count.
- Hematocrit - indicates how much blood is contained in red blood cells. An increase in hematocrit may be a sign of erythrocytosis (increased red blood cell count) or dehydration. A low hematocrit can be observed with anemia or be evidence of an increase in the amount of fluid in the blood.
- Platelets - these blood cells prevent blood loss when blood vessels are damaged. An increased level of platelets, detected during a general blood test, is observed after removal of the spleen and in a number of blood diseases. If this indicator is below normal, this may indicate cirrhosis of the liver, idiopathic thrombocytopenic purpura, aplastic anemia, congenital blood diseases, etc.
- Leukocytes are responsible for protecting the body from bacteria, viruses and other infections. In the presence of infection, their levels increase. A decrease in the level of white blood cells may indicate blood diseases, and is also observed when taking a number of drugs.
- Granulocytes - the number of these cells can be increased during inflammatory processes, and a decrease in granulocytes can be a consequence of taking a number of medications, aplastic anemia and systemic lupus erythematosus.
- Monocytes are a type of white blood cell that turns into macrophages (cells whose task is to absorb bacteria and dead body cells). A high level of monocytes in the blood is observed in blood diseases, infectious diseases, and rheumatoid arthritis. A decrease in monocytes usually occurs under the influence of drugs that suppress the immune system, as well as after severe operations.
- Lymphocytes are a type of white blood cell responsible for fighting viruses and germs, as well as for developing immunity. An increased level of lymphocytes can be a sign of some blood diseases and infectious diseases; a decreased level is observed in conditions of immunodeficiency (renal failure, taking drugs that suppress the immune system, AIDS).
Each of the given indicators is important when deciphering a blood test, however, a reliable result of the study consists not only of comparing the data obtained with the norms - all quantitative characteristics are considered together, in addition, the relationship between various indicators of blood properties is taken into account.
Decoding the results
When receiving MID test results, the patient sees the values as percentages. Today, the results obtained are deciphered by special equipment, making errors in the interpretation of the obtained values unlikely.
Normal for women and men
Blood performs a number of important functions for the body, among which are the supply of organs with oxygen and essential microelements, as well as participation in protecting the body from various kinds of diseases. Thanks to blood, optimal body temperature is maintained, transportation of necessary elements to organs and systems is ensured, and carbon dioxide is removed. A general blood test gives a detailed picture of the state of the hematopoietic system.
Important! Normally, the content of a combination of eosinophils, basophils and monocytes in the total number of leukocytes ranges from 5-10%.
For men and women, these indicators are identical, that is, they are within the same limits.
Normal for a child
Blood composition indicators immediately begin to respond to changes occurring in the body. This applies to both adult patients and children.
If we talk about the norm of MID in children, then in their case this figure varies in the range from 0.5% to 7%.
If we talk about the norm of the MID components separately, then in children it is not much different from in adults.
Monocytes:
- from birth to 12 years - 2-11%;
- over 12 years old - 3-12%;
Eosinophils: from birth to 18 years - 1-5%.
Basophils:
- 1 month - 11 years - 0.5%;
- 12 years - 18 years - 0.7%.
Components of MID
MID in the leukocyte formula combines the smallest types of white blood cells: monocytes, eosinophils, basophils.
Monocytes (MON)
Agranulocytic leukocytes of this type are large in size and have a red-violet nucleus. The cells are formed in the bone marrow and then move into the systemic circulation, where they live on average for about three days. Monocytes then transform into macrophages and move to the tissues of the liver, spleen and lymph nodes.
Macrophages are active phagocytes of the immune system that cleanse the body of cellular debris (dead cells) and bacterial microorganisms. The hallmark of MON is its survival. Neutrophilic granulocytes (neutrophils) are initially programmed to die after meeting foreign agents and performing their function, while monocytes are not destroyed, but continue their security activities.
In addition to phagocytosis, the responsibilities of monocytes include the production of the protective protein interferon, which inhibits the activity of viruses and is involved in building specific immunity, tissue regeneration, participation in the process of hematopoiesis, suppression of the activity of cancer cells, and protection of the body from cancer.
The monocyte variety of white cells copes more effectively with viral agents than with bacteria and parasites. An increased content of monocytes in the blood is defined by the term “monocytosis”. A reduced amount is called monocytopenia.
Eosinophils (EOS)
Of all MID representatives, eosinophils remain in the blood for the shortest amount of time. After moving from the bone marrow, they remain in the systemic circulation for several hours and are then transported to the tissues of the digestive system, lungs and epidermis (skin). Eosinophilic leukocytes are intended for the eradication of helminthic infestations through phagocytosis of pathogens, the formation of antiparasitic immunity, and the metabolism of histamine (a bioactive indicator of allergic reactions).
Along with basophils, eosinophil cells take part in the initiation of immediate hypersensitivity (the system's response to the introduction of allergens into the body). Eosinophilia (high concentration of eosinophils), first of all, means the presence of parasites or allergic antigens in the body. Eosinopenia (low cell count) has no particular diagnostic value.
Basophils (BAS)
The smallest, but very important type of granulocyte. The phagocytic properties of the cells are less developed than those of other leukocytes, but their membranes contain receptors for immunoglobulin E (IgE). When allergenic agents enter the body, IgE activates the allergic reaction through the release of histamine.
An increased concentration of basophils in the blood (basophilia) is a clinical sign of the development of allergies. In addition, these colorless cells contain heparin, which maintains stable blood flow in the capillaries and prevents increased blood clotting.
This effect helps maintain optimal blood circulation in small vessels, liver and lungs. Basophils do not have accumulative properties in tissues, like other leukocytes. They move to the inflamed area as needed, eliminate the foreign invasion and die. A decrease in BAS levels is called basopenia.
Differences in indicators and boundaries of reference values
Blood decoding based on these indicators can exist in two versions: MID (MID) and MXD. What do these symbols mean?
- MID analysis - The absolute number of leukocytes, as well as their precursors or young forms, which circulate in the peripheral blood in small quantities relative to neutrophils and lymphocytes,
- MXD is the same value, only taken in a relative form.
What is the difference between absolute and relative content, and what does it mean? The answer is very simple: any absolute value is expressed as the number of cells per unit volume, and any relative value is expressed as a percentage relative to the total population. Since computerized algorithms can now make almost any calculation based on a given formula, there are a variety of red blood cell and leukocyte indices, many of which are not required by the doctor, but they are still displayed, “just in case.”
In the blood, the normal mid is 0.2-0.8 x 109/l. It is in this quantity that rare white blood cells are found. If we compare this value with the number of leukocytes in the blood in general, that is, with 4-9 x 109/l, then we can estimate how much less there are normally. In terms of relative abundance, it usually accounts for 5 to 10% of the total leukocyte population.
Results
MID is a combination of indicators of three groups of leukocyte cells: basophils (BAS), eosinophils (EOS) and monocytes (MON), determined during a general clinical analysis of capillary blood. These cells are the smallest in the overall composition of biological fluid, but have important diagnostic value for determining parasitic diseases, allergic reactions, malignant pathologies and infectious processes in the body.
The results of the total amount study (MON+ EOS+BAS) or absolute MID values are 0.2-0.8*10^9/l. Relative values are measured as percentages and amount to 5-10% of the total number of leukocytes. If the MID in the blood test is increased or decreased, it is necessary to thoroughly evaluate and compare all indicators of the leukocyte formula.
The extended leukogram provides separate normative values for all representatives of white blood cells (leukocytes). Unsatisfactory results of the analysis require additional laboratory tests (blood biochemistry, urine analysis, coprogram) and hardware diagnostic procedures (ultrasound, X-ray, MRI, CT, etc.).
Norms of indicators mid
Since the level of eosinophils, basophils and monocytes in the total number of leukocytes is quite small, these values were combined into a single indicator. But each of them has its own functionality, and when one of the factors changes, the whole picture changes.
If mid is low or high in a blood test, consider separately:
- Monocytes. The norm in men and women in percentage terms is 3–10%. A decrease in the indicator may indicate exhaustion, the formation of tumors, being in a state of shock, problems with the immune system, or abuse of hormonal drugs. An increase indicates the presence of infections and inflammations.
- Eosinophils. The norm in adults is 0.5–5%. A decrease indicates a decrease in immunity, intoxication, the presence of inflammatory processes of an infectious nature, and changes in the circulatory system. An increase occurs during allergic reactions of the body and various invasions.
- Basophils. Their number per total volume is only 0.5–1%. Larger changes are observed with allergies, diabetes, lung cancer, the presence of viral diseases, and changes in the circulatory system. The decrease is typical during periods of taking hormonal medications, stressful situations, and infectious diseases.
Normal indicator for children
It should be remembered when deciphering the analysis that for mid the norm in children differs slightly from the values in adults.
- From birth to 12 years, the norm of monocytes is in the range of 2–11%. After 12 years and until adulthood, the rate is slightly higher and ranges from 3 to 12%.
- In children, the level of eosinophils from the first day of birth until the age of 18 is within 1–5%.
- The number of basophils in a child changes with age. At birth it is usually zero. From 1 month to 11 years - 0.5%. From 12 to 18 years old - 0.7%.
What does this indicator mean?
Today, patients are more conscious of their own health and try to understand the significance of the tests that are prescribed to them by their attending physicians.
One such test is a blood test for MID, which reflects the content of eosinophils, basophils and monocytes. If we recall the history of medicine, we can see that previously the designation of the indicator was MXD. However, due to the fact that eosinophils, basophils and monocytes belong to the intermediate cells of leukocytes, the term MID began to be used. The key task of such cells is to protect the body from various types of infections.
Deviations revealed by test results are a possible sign of disturbances in the functioning of the human immune system, which can be caused by various pathologies. In addition, such a phenomenon may indicate the body’s fight against harmful microbes and viruses. This is precisely what determines the importance of MID analysis and the correct interpretation of its results.
How to take an analysis to determine the MID indicator
To find out the MID (MXD), you need to donate blood from a finger, less often it is taken with a syringe from a vein. The blood to be tested is usually taken from the ring, middle or index finger. Unnamed is preferable, because it is least involved in daily activities and heals faster, and its skin is thinner.
During the selection procedure, a puncture is made with a disposable instrument - a scarifier, or a lancet - an automatic instrument with a needle in a plastic case. They are released from packaging in the presence of the patient, which eliminates concerns about the sterility of the instrument and the risk of infection.
When using a scarifier, the puncture can be painful, which causes negative perceptions of medical care in children.
Therefore, if a child is undergoing the study, ask if there are lancets in the blood collection room. If the answer is negative, you can purchase it at the pharmacy and bring it with you. With the help of a lancet, the puncture is made quickly, purposefully and with a controlled depth, which reduces pain to a minimum.
After puncture, using a special adapter, the second and subsequent drops of blood are collected by massaging the fingertip into a glass tube. To ensure that an absolutely healthy body does not show parameters characteristic of a patient during the study, it is necessary to follow the following simple rules before the blood sampling procedure:
- you should not consume food, tea, coffee, or other drinks other than water at least 8 hours before the blood test;
- drinking alcohol the day before is prohibited - it can greatly distort the blood picture, the same applies to smoking;
- It is necessary to refrain from physical and emotional stress on the day preceding the analysis; it is recommended to get a good night's sleep.
Features of the study
A general blood test is one of the most popular and most highly informative ways to determine the state of health of the body.
It is performed in almost any medical institution that has its own laboratory.
When examining blood using laboratory methods, a large number of different indicators are determined, each of which has its own specific norm.
Photo:
A blood test is taken from a finger, or in some cases from a vein. The examination itself is considered quite simple, but requires the patient to follow some simple rules.
You should take a blood test on an empty stomach in the morning. On the eve of the study, you should avoid fatty, fried and spicy foods.
In addition, it is highly undesirable to drink alcohol a few days before the blood test.
If you do not follow these basic recommendations, then according to the survey results, the norm for many indicators will differ significantly from the true value.
This will lead to the fact that the reliability of the blood test as a whole will sharply decrease.
Each indicator that is determined in the blood in the laboratory can be increased or, conversely, decreased, which indicates certain problems with the body.
Meanwhile, the norm indicates the absence of problems and various diseases. A general blood test allows us to establish both the pathology itself and its main causes.
READ What should be the normal level of creatinine in the blood?
Video:
To determine the overall picture of a person’s health, all the main blood indicators are determined in the laboratory, after which they are deciphered.
Each indicator is carefully analyzed separately. If any parameter is increased or decreased, this means that there are certain problems in the body.
First of all, the number of red blood cells is determined, as well as the total level of hemoglobin. Each of them has its own specific norm, and the decoding allows us to determine the resulting value in accordance with it.
Basophils
If the patient has complaints of allergic reactions, then testing for basophils plays an important role in case of increased MID in the blood test. What it is? Basophils fight allergens that enter the body. This releases histamine, prostaglandins and other substances that cause inflammation.
Normally, the relative amount of basophils in the blood in adults is 0.5-1%, and in children 0.4-0.9%.
An increased content of these cells is called basophilia. This is quite a rare occurrence. It is usually observed in allergic reactions and hematological pathologies such as leukemia and lymphogranulomatosis. Basophils can also be elevated in the following pathologies:
- gastrointestinal diseases;
- diabetes;
- chickenpox;
- early stages of respiratory tumors;
- hypothyroidism;
- iron deficiency;
- taking thyroid hormones, estrogens and corticosteroids.
Sometimes basophils can be slightly elevated in minor chronic inflammations. Slightly increased levels of these cells are observed in women at the beginning of menstruation and during ovulation.
If, with a reduced MID, the decoding of the blood test for basophils shows results less than normal, then this indicates a depletion of the leukocyte supply. The reasons for this analysis result may be different:
- physical and emotional stress;
- increased activity of the thyroid or adrenal glands;
- acute infections;
- exhaustion.
It must be remembered that false test results are possible in women during pregnancy. This is due to an increase in blood volume, which causes the relative number of basophils to decrease.
Leukocyte indices
Of the parameters describing the main populations of white blood cells (WBC), the indicators of numerous cell populations have the greatest diagnostic value. In a blood test, these include granulocytes (GRAN, GRA, GR) and lymphocytes (LYMPH, LYM).
The group of granulocytes is represented mainly by neutrophils. Eosinophils and basophils, which also contain cytoplasmic granules within the cell and belong to granulocytes, are found in the blood in small quantities.
Due to the small number of basophils and eosinophils, all properties of GRA, as a component of cellular immunity, are determined mainly by neutrophils.
Small populations of leukocytes are combined into one group or, as it is also called, a mixture of leukocytes. When counted in a hematology analyzer, this total combination of eosinophils, monocytes and basophils is designated MID or MIX.
The indicators MID%, GRA%, LYM% are indicated in the blood test transcript as a percentage of the total number of leukocytes and in absolute indicators (#), reflecting how many population cells are contained in a unit volume of blood plasma.
Normally, the absolute number MID# is 0.2 – 0.8*109/l. The percentage or relative indicator of the mixture of cell populations of eosinophils, basophils, monocytes MID% lies in the range of 5% - 10%.
MID values are determined primarily by the blood monocyte count (MON). The concentration of monocytes in a healthy person is higher than the level of basophils and eosinophils.
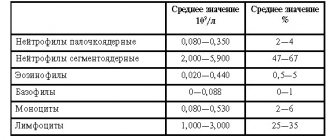
For comparison, the norms in the CBC (general blood test):
- basophils - BASO% - 0 - 1%, BASO# - up to 0.09*109/l;
- eosinophils – EOS% – up to 5%, EOS# – up to 0.3*109/l;
- monocytes – MON% – 2 – 9%, MON# – 0.09 – 0.6*109/l.
This suggests that with an increase in MON, a value such as MID also increases in blood tests. And when BASO or EOS increases or decreases, the MID indicator changes little.
The GRAN% concentration in a blood test is 45 – 72% of total leukocytes. The absolute amount of GR is 1.2 – 6.8*109/l.
The content of GRA in the blood can be calculated from the results of the analysis using the formula WBC - LY - MON, where WBC is leukocytes, the same value as LY - lymphocytes, and MON, which means “monocytes”.
Granulocytes are reduced during a long course of infectious diseases caused by bacteria, AIDS viruses, measles, influenza, and rubella. Anemia, radiation therapy, and malaria can cause a decrease in granulocytes.
GRAN indicators are increased in the blood with an increase in neutrophil leukocyte indicators, which can be read about on a separate page of the site.
Basic values
Blood is an important element of the human body. It is she who is responsible for the delivery of oxygen to all internal organs and tissues.
If any of its indicators are increased or decreased, this means that the body does not receive enough nutrition in full.
A blood test reveals the number of leukocytes and platelets. The last indicator characterizes the degree of bleeding in case of external damage to blood vessels.
The decoding also shows such an important value as ESR. If this indicator is elevated, then the patient may develop an infectious disease, for example, tuberculosis or syphilis.
Video:
The laboratory also establishes the MID value, which is characterized by the total content of blood components such as monocytes, eosinophils, basophils in percentage terms.
Each blood indicator has its own norm, however, small deviations from it are possible due to the individual physiological characteristics of each patient.
All this must be taken into account when drawing up a final conclusion based on the results of a blood test.
A blood test is highly informative, and if all the basic rules for taking it have been followed, then you can obtain reliable values for many indicators, on the basis of which various pathologies are diagnosed.
READ What does increased hemoglobin mean in women?
Photo:
The norm for some parameters may differ slightly between men and women due to their physiological characteristics.
In this case, any blood parameter in one sex may be increased or, conversely, decreased when its value is normal.
The blood test is carried out on the direction of the attending physician, and it is not necessary to have any symptoms to perform it.
It is recommended to take this test at least once a year as a preventative measure.
The blood test itself is carried out in several stages using various equipment and special chemical indicators.
Video:
The first step is to check the ability of the blood fluid to nourish internal organs and tissues. In this case, the number of red blood cells is determined.
The norm for this parameter for women is in the range from 3.8 to 5.5x1012/l, for men - from 4.3 to 6.2x1012/l, in addition, there is a value for children.
What do deviations mean?
A deviation from the norm of the MID indicator to a greater or lesser extent most likely indicates pathology. It should be noted right away that the value cannot be influenced by any random factors. However, it is incorrect to diagnose a patient based only on the results of this study.
Eosinophils
If we talk about the norm of eosinophils in the leukocyte structure, then it is 1-5%. With elevated levels, experts talk about eosinophilia, which may be a sign of the following pathologies:
- the appearance of worms;
- development of an allergic reaction;
- the emergence and development of malaria;
- presence of bronchial asthma;
- non-allergic skin pathologies;
- development of rheumatoid processes;
- previous myocardial infarction;
- blood diseases;
- formation of malignant tumors;
- development of pneumonia;
- deficiency of immunoglobulins;
- development of liver cirrhosis.
In addition to pathology, taking certain medications, including antibiotics, hormones, etc., can provoke an increase in eosinophils. When eosinophils are low, experts talk about eosinopenia. The reason for this may be:
- severe infectious processes;
- development of sepsis;
- peritonitis due to appendicitis;
- prolonged state of emotional stress;
- previous injuries;
- burns received;
- previous operations;
- chronic lack of sleep.
Deviation of the result from the established norm may be a consequence of recent childbirth, surgery, or taking medications.
Basophils
If there is an allergic reaction, the patient is prescribed a test for basophils. In adults, the relative level of basophils varies from 0.5 to 1%.
Reference! In case of high content, experts talk about basophilia. This happens quite rarely. As a rule, with the development of an allergic reaction or with diseases of a hematological nature, for example, leukemia.
In addition, an increase in basophil content may occur in the following cases:
- diseases of the digestive system;
- diabetes mellitus;
- chickenpox;
- formation of tumors of the respiratory organs at an early stage;
- iron deficiency;
- hypothyroidism;
- taking hormonal medications to compensate for thyroid hormones.
If we are talking about a reduced concentration of basophils, then we are talking about a lack of leukocytes, which may be a consequence of:
- excessive physical and emotional stress;
- increased work of the thyroid gland or adrenal glands;
- acute infectious processes;
- exhaustion.
Monocytes
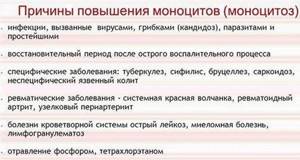
As for monocytes, an excess of this indicator relative to the norm can occur when:
- development of a viral infection;
- the appearance of worms;
- development of tuberculosis;
- infection with syphilis;
- development of autoimmune pathologies;
- bone marrow diseases, etc.
A decrease in the level of monocytes indicates the following pathological conditions:
- development of a purulent-inflammatory process;
- depletion of the immune system;
- excessive use of hormonal drugs;
- blood diseases.
What to do if downgraded or upgraded?
If MID values are abnormal, the patient is referred for additional testing. It is impossible to identify any pathology using these results alone. The prescribed treatment will depend on the diagnosed pathology.
If the deviation from the normal value is a consequence of an infectious disease, then the patient will be prescribed antibiotic and antiviral drugs. If we are talking about allergies, then antihistamines are prescribed. In turn, blood diseases require long-term and complex treatment.
In some cases, deviations from the normal level do not require therapeutic intervention. To do this, only changing the patient’s lifestyle is sufficient. However, such a scenario is possible only in the absence of serious illnesses.
Thus, analysis to determine the level of MID has enormous diagnostic value . In this case, it is very important to correctly interpret the results of a general blood test and choose further tactics for diagnosing and managing diseases.
Components of MID
MID in the leukocyte formula combines the smallest types of white blood cells: monocytes, eosinophils, basophils.
Monocytes (MON)
Agranulocytic leukocytes of this type are large in size and have a red-violet nucleus. The cells are formed in the bone marrow and then move into the systemic circulation, where they live on average for about three days. Monocytes then transform into macrophages and move to the tissues of the liver, spleen and lymph nodes.
Macrophages are active phagocytes of the immune system that cleanse the body of cellular debris (dead cells) and bacterial microorganisms. The hallmark of MON is its survival. Neutrophilic granulocytes (neutrophils) are initially programmed to die after meeting foreign agents and performing their function, while monocytes are not destroyed, but continue their security activities.
In addition to phagocytosis, the responsibilities of monocytes include the production of the protective protein interferon, which inhibits the activity of viruses and is involved in building specific immunity, tissue regeneration, participation in the process of hematopoiesis, suppression of the activity of cancer cells, and protection of the body from cancer.
The monocyte variety of white cells copes more effectively with viral agents than with bacteria and parasites. An increased content of monocytes in the blood is defined by the term “monocytosis”. A reduced amount is called monocytopenia.
Eosinophils (EOS)
Of all MID representatives, eosinophils remain in the blood for the shortest amount of time. After moving from the bone marrow, they remain in the systemic circulation for several hours and are then transported to the tissues of the digestive system, lungs and epidermis (skin). Eosinophilic leukocytes are intended for the eradication of helminthic infestations through phagocytosis of pathogens, the formation of antiparasitic immunity, and the metabolism of histamine (a bioactive indicator of allergic reactions).
Along with basophils, eosinophil cells take part in the initiation of immediate hypersensitivity (the system's response to the introduction of allergens into the body). Eosinophilia (high concentration of eosinophils), first of all, means the presence of parasites or allergic antigens in the body. Eosinopenia (low cell count) has no particular diagnostic value.
Basophils (BAS)
The smallest, but very important type of granulocyte. The phagocytic properties of the cells are less developed than those of other leukocytes, but their membranes contain receptors for immunoglobulin E (IgE). When allergenic agents enter the body, IgE activates the allergic reaction through the release of histamine.
An increased concentration of basophils in the blood (basophilia) is a clinical sign of the development of allergies. In addition, these colorless cells contain heparin, which maintains stable blood flow in the capillaries and prevents increased blood clotting.
This effect helps maintain optimal blood circulation in small vessels, liver and lungs. Basophils do not have accumulative properties in tissues, like other leukocytes. They move to the inflamed area as needed, eliminate the foreign invasion and die. A decrease in BAS levels is called basopenia.
Components
So, when assessing MID, the quantitative composition of elements such as eosinophils, basophils and monocytes is examined.

- Eosinophils are the cells responsible for producing bone marrow. As you know, when any infection enters the body, the immune system begins to produce antibodies. As a result, complex complexes are formed that help the body fight foreign proteins. And it is eosinophils that neutralize these proteins and help cleanse the blood.
- In the case when a patient complains of an allergic reaction, great importance is attached to the analysis of the quantitative content of basophils in the blood. They allow the body to fight various irritants in the form of allergens.
- Monocytes are blood cells that primarily fight viral infections. These cells can overcome not only foreign proteins, but also already dead leukocytes, as well as damaged cells. It is thanks to monocytes that suppuration does not appear in the event of a viral inflammatory process.
Leukocytes: granulocytes and agranulocytes
In a broad view of the composition of blood, red blood cells and white blood cells are distinguished. White blood cells are grouped under the general concept of “leukocytes.” These include many cells that differ in appearance, structure, functions and maturation dynamics in the body. Based on their functionality, leukocytes are divided into cells that perform phagocytosis (capture and lysis of foreign organisms) and cells that produce antibodies.
The generally accepted classification of leukocytes is based on morphological characteristics: the presence or absence of granules in the cytoplasm of the cell, stained using the Romanovsky-Giemsa method:
- Granulocytes. They have large kernels divided into segments. The stained cytoplasm in the microscope has a characteristic granularity. Grains are lysosomes, peroxisomes with granules of hydrolytic enzymes. Based on the ability of cells to be stained with alkaline and acidic dyes, neutrophils (all dyes), eosinophils (acidic), and basophils (alkaline) are distinguished.
- Agranulocytes. They are not grainy and contain a regular core. Agranulocytes are lymphocytes and monocytes.
When is the test prescribed?
CBC is the most common clinical test. It is recommended to undergo it when visiting a doctor about a disease, as well as for preventive purposes during medical examination. The analysis may be prescribed if the following diseases are suspected:
- infections;
- inflammatory processes;
- allergy;
- tumors;
- anemia.
Abbreviated and extended blood test
In the abbreviated version of the study, the MID is necessarily determined in a blood test. What it is? If a person does not have any complaints, and OAC is carried out for the purpose of prevention, then a shortened analysis is done. In addition to MID, the following indicators are calculated:
- hemoglobin;
- ESR;
- platelets;
- red blood cells;
- total number of leukocytes.
If abnormalities were detected during the abbreviated CBC, then a more detailed study is carried out. For example, if the MID norm in a blood test is exceeded, decoding must be carried out for each type of cell separately. For this purpose, a detailed examination is prescribed to determine the leukocyte formula.
MID in a blood test: what it means and what is the norm
When deciphering a general blood test performed on a hematology analyzer, you can find the MID indicator. It combines the total number of monocytes, basophils and eosinophils.
Normally, they are found in the blood in small quantities, so these cells are combined into one general group.
The norm for men and non-pregnant women is 0.2-0.8*10 G/l.
As a percentage, this corresponds to 5-10% of the total number of all leukocytes in the analysis. In this case, there should be 3-7% monocytes, 0-6% eosinophilic granulocytes, and 0-2% basophils.
The absolute norm in women during pregnancy, during ovulation and during menstrual bleeding is slightly higher and can reach 0.3-0.9 * 10 G/l, however, the percentage of monocytes, eosinophils and basophils remains the same.
In some pathological conditions, immature forms of leukocytes are found in the blood - metamyelocytes, myelocytes, and young ones. When counting formed elements using an automatic analyzer, these cells will fall into the MID group.
The reference MID values in a blood test in a child after 5 years of age do not differ from those in an adult. From the first week of life to the second physiological crossover, this parameter may be slightly higher.
Reasons for increased MID in blood tests
The MID increases as the number of one of the groups of cells that make up its composition increases. The causes of an increase in monocytes are often viral diseases, such as mononucleosis, cytomegalovirus infection, measles, rubella, mumps, and influenza.
Monocytes may increase in some cancers, as well as blood cancer (chronic and acute leukemia). The level of immune cells also increases in severe forms of tuberculosis, syphilis and rheumatoid arthritis.
The most common causes of an increase in the number of eosinophils, and with them an increase in the MID indicator, are parasitic diseases, giardiasis, as well as allergic pathologies (atopic and contact dermatitis, bronchial asthma, urticaria), fungal pathologies.
The normal MID blood test in children is often deviated due to eosinophils due to helminthic infestations - ascariasis and enterobiasis.
Basophils may be elevated in acute and chronic leukemia, lymphoma, and some childhood viral diseases, such as chickenpox. A slight increase in the number of this group of leukocytes is observed in chronic heart pathologies, thyroid diseases, inflammatory bowel pathologies, and after removal of the spleen.
One of the common reasons for an increase in MID in a child’s blood test may be iron and protein deficiency due to poor nutrition, fasting, and disruption of the gastrointestinal tract.
Physiological reasons for increased MID
Women are characterized by a physiological increase in this indicator during the period of bearing a child, starting from the first trimester, during ovulation, during menstrual bleeding.
Also, a slight deviation from the generally accepted norm is diagnosed in women taking estrogen preparations and combined oral contraceptives. After childbirth, representatives of the fair sex experience a decrease in the number of leukocytes.
MID reduction
A decrease in MID is most often observed with a decrease in the number of eosinophils and monocytes. Pathologies such as:
- Aplastic and hypoplastic anemia.
- Leukemia (acute, chronic, hairy cell).
- Lymphogranulomatosis, lymphoma.
- Severe purulent pathologies - phlegmon, abscesses, inflammation of internal organs, sepsis.
The content of a mixture of monocytes, eosinophils and basophils decreases when taking cytostatics, steroids, immunosuppressants, as well as poisoning with heavy metals and phosphorus.
In order to determine MID, it is necessary to donate blood from a vein to a laboratory that has a hematology analyzer. The rules for donating blood remain general. You must come to the clinic on an empty stomach, after an 8-10 hour fast. The day before the test, you should give up alcohol, fatty and fried foods, allergens, and avoid heavy physical activity and stress. The result of a detailed blood test becomes known a few hours - a day after it is taken.
Reasons for the increase in monocytes, what symptoms accompany monocytosis
The MID in a blood test can be elevated due to various internal diseases. In this case, the level of formed elements increases to 1 thousand per 1 μl of blood and depends on the severity of the disorder and other physiological factors.
Symptoms for violations are practically absent. The diagnosis is made based on the manifestations characteristic of a particular disease.
The development of a disorder can be suspected based on the following indirect signs:
- weight loss (in the absence of changes in lifestyle;
- complete or partial loss of appetite;
- general weakness and fatigue;
- psycho-emotional disorders – anxiety, panic attacks;
- dislike of meat foods;
- disorders of the nervous system - insomnia, irritation, apathy;
- changes in stool - presence of impurities, irregularity, presence of foamy discharge;
- pain syndrome developing in the epigastric region;
- cough (especially dry and with the release of viscous secretions or blood);
- pain in muscles and joints;
- rash on the skin or mucous membranes, which has a specific character (in some cases, rashes can form in the genital area);
- discomfort and development of pain during sexual intercourse.
These symptoms can develop either individually or in combination, depending on the pathology that provoked a decrease in the number of blood cells.
Convalescence
The condition is otherwise called recovery - the period after the disease has been suffered and cured. In most cases, the process develops in children after an infection. In this case, the condition indicates the complete removal of the pathogen that provoked the development of the disease.
There are no manifestations, the form of the flow is insignificant. The process lasts up to 2 weeks and does not require any therapy.
Viral infections
MID in blood tests is slightly increased in viral infections and does not require special therapeutic measures. When infected with a virus, monocytes act as the body's first defense reaction. Heading to the lesions, they transform into macrophages and absorb microorganisms. In this case, the elements produce antigens on their surface to a specific infectious agent.
Macrophages are also responsible for the production of various mediators and cytokines and guide neutrophils to the affected areas.
In some cases, infectious viral diseases can additionally lead to enlarged lymph nodes.
Classification of violations:
- Acute viral infections. The most common diseases are influenza or ARVI. The increase in the number of monocytes is insignificant and gradually returns to normal 2 weeks after the condition improves.
- Infectious mononucleosis. Pathology develops in children when infected with the Epstein-Barr virus. The condition is accompanied by characteristic symptoms and can persist from several months to several years. In this case, a large number of lymphocytes are formed, which have properties similar to monocytes.
The exact form of the disease can be established only after complex diagnostic procedures.
Bacterial infections
An increase in the level of monocytes can be observed during chronic bacterial infections. Most often, the condition develops against the background of tuberculosis, brucellosis or syphilis. Pathology can also be observed with endocarditis and rickettsiosis. At the same time, the level of blood cells differs slightly from the number of monocytes during the development of viral infections.
The main cause of the disorder is disruptions in the processes of phagocytosis. When capturing pathogenic cells, macrophages are not able to completely destroy them, as a result of which the microorganisms remain on the surface of monocytes and are protected from the influence of other immune cells.
Against the background of the process, a chronic course of the disease occurs, which can persist for several months or years. The condition stabilizes only after appropriate therapy aimed at eliminating the underlying cause of the disease. The concentration of monocytes is moderate. The main and only disorder in children leading to pathology is scarlet fever.
Systemic granulomatous processes
The pathology is a chronic non-infectious disease of a systemic nature that develops against the background of the formation of granulomas from macrophages, lymphocytes and mast cells. These formations accumulate in tissues.
Disorders occur in children as a result of the development of ulcerative colitis and Crohn's disease.
In adult patients, the main causes of pathology are the following diseases:
- sarcoidosis;
- histiocytosis;
- Wegener's granulomatosis.

Monocyte levels are slightly elevated compared to bacterial or viral infections.
Diffuse connective tissue diseases
An increase in MID in the blood can also occur when diffuse connective tissue diseases occur. However, the disease is rare and requires additional tests to accurately determine its presence, stage of development and form.
At the moment, the exact reasons for the development of pathology have not been established. According to one of the most popular theories, against the background of the production of autoantibodies, monocytes are formed in the bone marrow tissue. The inflammatory process is directly related to the production of monocytes.
The main causes of the disease are the following disorders:
- systemic lupus erythematosus;
- systemic scleroderma;
- dermatomyositis;
- polymyositis.
The number of formed elements is associated with the stage of the disease. During remission, their levels remain within normal limits.
Malignant blood diseases
Oncological pathologies of the circulatory system can also lead to an increase in the level of monocytes. The process is associated with the transformation of bone marrow stem cells. At the same time, the concentration of formed elements is high and can reach half the level of the total number of leukocytes. The increased number of monocytes persists for a long time and decreases only after chemotherapy or surgical interventions associated with bone marrow transplantation.
Possible causes (pathologies):
- myeloid leukemia, occurring in a chronic form (observed in adults);
- Hodgkin's lymphoma (a disorder typical of children);
- acute course of monocytic leukemia (in children).
In acute forms of the disease, a so-called leukemic failure may occur.
Neutropenia
A group of diseases characterized by decreased production of neutrophils, which are produced by the bone marrow. Most often, the pathology develops in children and is caused by a congenital (genetic) predisposition.
Causes:
- childhood agranulocytosis (CAA);
- neutropenia (cyclic form of the disorder);
- chronic neutropenia (myelocachexia).
In most cases, this form of monocytosis is accompanied by an increase in the level of eosinophils in the blood.
Rare causes
MID in a blood test can also be elevated for other rarer reasons, which occur in isolated cases and are most often observed in young children.
Thus, the disorder develops against the background of the following factors:
- Parasitic infestations. These pathologies include malaria, Borovsky's disease (including the visceral form of the disorder).
- Intoxication (poisoning). In most cases, it occurs due to poisoning with tetrachloroethane or phosphorus.
- Use of medications. Monocytosis can develop as a result of prolonged use of glucocorticosteroids (injection).
The condition may also be caused by the use of chemotherapy drugs (treatment of myelosuppression).
Healing procedures
Therapy will depend on the reason that provoked the increase or decrease in mid. At low level:
- it is recommended to discontinue medications that could lead to changes;
- it is necessary to increase the rest time; during the treatment period, physical and emotional stress should be limited;
- It’s worth reviewing your diet;
- When infectious diseases are detected, symptomatic treatment is prescribed.
When the indicator is too high, it is recommended:
- Taking antihistamines for allergies.
- Prescribing broad-spectrum antibiotics and eliminating signs of infection with other drugs, depending on the symptoms.
- Parasitic treatment when helminthic infestation is detected.
- Elimination of inflammatory processes.
- Taking sorbents during intoxication.
If the mid values in the general analysis do not correspond to the norm, this may mean that there is an inflammatory process in the body or an infectious disease is beginning. But before making a final conclusion, it is necessary to compare other decoding indicators, since the content of mid in the total leukocyte mass is insignificant and does not exceed 10%.