Greetings to all readers on the blog!
Platelets are blood cells whose main task is to ensure normal blood clotting in order to prevent the loss of large volumes of blood and the rapid healing of wounds on the body. The success of pregnancy and childbirth depends on their quantity in a pregnant woman’s body.
A lack of blood platelets, on the contrary, can negatively affect the health of the expectant mother and her child. Today we will look at a situation where the analysis showed underestimated results and find out how to increase platelets in the blood during pregnancy with the help of medication, folk methods and a therapeutic diet.
Platelets in the blood of a pregnant woman: norms and causes of deviations
In normal conditions, in men and women, platelet levels in the blood are 180-400 g/l. These indicators may be subject to slight fluctuations throughout the day, which is due to their short lifespan - no more than 10 days.
In women during the period after menstruation, the number of blood cells drops to 100-350 g/l, and in the body of pregnant women under normal conditions they are 100-420 g/l. Under the influence of certain internal and external factors, these indicators may decrease or increase in expectant mothers.
In any case, doctors talk about a pathological condition. For comparison, you need to figure out what elevated platelets mean. This condition is called thrombocytosis and is diagnosed only when the norm of blood cells is very much exceeded.
Methods for eliminating the disease can be determined after doctors find out why the blood elements are elevated. Basically, this deviation in pregnant women is a consequence of impaired drinking, severe toxicosis and poor nutrition.
More often in gynecological practice, the other side of the pathology is encountered - low levels of platelets in the blood of girls during the period of bearing a baby. This disease is called thrombocytopenia.
The causes of the pathology may be the following:
- allergy;
- poor nutrition;
- autoimmune diseases;
- HIV infection;
- pathologies of the endocrine system;
- diseases of the circulatory system;
- taking potent medications;
- acute infectious diseases;
- chronic diseases.
If platelets are elevated in an adult in a normal state, then it is necessary to find out the physiological reason for this phenomenon, which can occur during physical overexertion, the release of large doses of adrenaline into the blood, or pregnancy. The norms of blood elements in a child in the first days of life are 100-420 g/l, and in children after a year - 180-400 g/l.
Disturbances in the hemostatic system and its correction in pregnant women with metabolic syndrome
The frequency of metabolic syndrome according to various authors is 5–20% (I. Despres, A. Marette, 1994). It should be noted that obesity is one of the main components of metabolic syndrome, and the number of obese women, including pregnant women, is progressively increasing.
There is a significant number of works devoted to the effect of obesity on the course of pregnancy and childbirth. However, a few studies have been devoted to the study of some metabolic parameters. Thus, G. A. Chernukha (1987) showed a violation of the hormonal profile in the system of hemostasis and lipid metabolism in obese pregnant women. V. N. Serov et al. (2000) noted changes in metabolic processes in pregnant women with obesity and underweight, in particular hypo- and dyslipidemia, and decreased glucose tolerance.
An important component in pregnant women with metabolic syndrome is impaired blood flow in the maternal system due to obesity, impaired placental insufficiency, altered hormonal profile: increased leptin levels, altered insulin ratio and altered water-electrolyte balance.
However, in the literature available to us, we did not find any studies that would link obesity in pregnant women with the presence of metabolic syndrome.
The purpose of our study was to study changes in the hemostatic system, the frequency of metabolic syndrome and its correction in pregnant women with metabolic syndrome and to determine the impact of these changes on the course of pregnancy and childbirth.
The task was set to find out the pathophysiological mechanism of the development of blood hypercoagulation and endothelial damage in pregnant women with metabolic syndrome. The study included 43 pregnant women with metabolic syndrome aged 27 to 37 years in the third trimester of pregnancy, including 8 pregnant women who developed moderate gestosis. As a control, 15 healthy pregnant women of the same gestational age were observed. All pregnant women underwent a clinical examination including an oral stress test for glucose tolerance. The inclusion criteria for pregnant women in the main group were: arterial hypertension, visceral obesity, hyperinsulinemia and hyperglycemia.
Laboratory research
Blood was taken from the cubital vein on an empty stomach with the addition of the anticoagulant 0.6% ethylenediaminetetraacetic acid (EDTA). The level of fibrinogen, antithrombin III (AT III), plasma tolerance to heparin, fibrinolytic activity of blood, thromboxane B2 content, cAMP in platelets and prostacyclins were determined. Quantitative indicators of platelet aggregation were assessed by spontaneous aggregation induced by adenosine diphosphate (ADP) and collagen, and blood insulin was determined. To determine platelet aggregation, blood was taken into tubes containing a 3.8% sodium citrate solution in a 9:1 dilution. The quantitative characteristics of the rate and intensity of aggregation were assessed on an automatic two-channel laser aggregation analyzer using software.
To study spontaneous platelet aggregation, an aggregation curve recorded for 10 minutes without induction was analyzed. An ADP solution at concentrations of 1×10-5 M, % and 1×10-7 M, %, collagen, platelet activating factor, adrenaline 10-4 M, aggristin was used as an aggregation inducer. The protocol for studying platelet aggregation in platelet-rich plasma included measuring the maximum aggregation rate as a percentage. NO was determined using the method for determining NO2 nitrites and nitrates as products of nitric oxide metabolism in human serum using high-performance liquid chromatography on a Shimatsu device. Blood serum was frozen and stored at -70 degrees. During the analysis, the serum was thawed, diluted with an equivalent amount, the buffer and proteins were removed by filtration through an UltraFree Units filter in a centrifuge at 5 thousand rpm for 15 minutes. Quantitative analysis was performed by comparison with an external standard at a wavelength of 214 nm, followed by dilution.
Research results
Physiological pregnancy is accompanied by significant changes in the hemostatic system. To address the issue of the development of blood hypercoagulation in conditions of complicated pregnancy, we conducted a study of the hemostatic system and functional activity of the blood in pregnant women of the main and control groups. From the table 1 shows that in the control group the level of fibrinogen is 2.36, and in the main group 3.74, plasma tolerance to heparin in the control group is 948.0, and in the main group 724.0. A very important indicator is the AT III level. In the control group it is 37.6, and in the main group - 27.3. An increase in the level of fibrinogen in the main group is one of the important links in the microcirculation disorder, which is accompanied by a blockade of the transport of substances, in particular a disruption in the delivery of oxygen, glucose, lipids, and proteins to the fetus. Violation of membrane permeability is accompanied by a change in the nature of oxidative processes, in particular an increase in the level of anaerobic oxidation, the development of ischemic and dystrophic changes in fetal tissues.

Clinically, this is manifested by a decrease in fetal weight and asphyxia. A great danger of developing thrombosis during pregnancy is the combination of high levels of fibrinogen and a reduced AT III level. It is known that the anticoagulant activity of blood is ensured by a number of biochemical factors. One of the most active anticoagulants is the plasma cofactor of heparin AT III. It is a universal inhibitor of almost all enzyme coagulation factors (especially thrombin and factor Xa). A critical decrease in the level of AT III in pregnant women in the main group causes a preeclamptic state. Comparing the quantitative indicators of platelet aggregation in healthy women and in pregnant women with metabolic syndrome, we noted significant differences. What are the reasons for these changes? An important role is played by changes in the physicochemical properties of platelets during pregnancy and insulin resistance.
The resulting ischemia in organs and tissues disrupts the energy potential of platelets with the development of membrane depolymerization, corresponding to the loss by the cell of one of the forms of “free energy,” i.e., the energy of the transmembrane potential. Platelet aggregation in patients with metabolic syndrome, induced by ADP, increases significantly - up to 79.1% (in healthy individuals 61.0%). Platelet aggregation stimulated by collagen significantly increases - up to 69.0% (57.0% in healthy individuals). Collagen-induced aggregation is very important, since in the case of a slight morphological change in the vessel wall, conditions arise for the formation of an intravascular platelet thrombus.
Endothelial damage with collagen exposure is an important trigger for platelet aggregation. With metabolic syndrome in pregnant women, platelet aggregation changes significantly under the influence of adrenaline. If in healthy women with physiological pregnancy it is 13.4%, then with metabolic syndrome it increases to 30.2%. Adrenaline-induced platelet aggregation in pregnant women with metabolic syndrome indicates a sharp increase in the sensitivity of the platelet receptor apparatus to adrenaline.
It follows from this that even minor emotional stress and moderate physical activity can provoke activation of platelet aggregation with possible progression to the development of a preeclamptic state. The pathophysiological basis for changes in platelet aggregation during gestosis is a violation of the cell's cAMP activity. It is the high level of platelet cAMP that allows it to maintain functional viability: metabolism, energy and information exchange.
In pregnant women in the control group, the platelet cAMP level is 4.1 pmol (3×108 cells); in women with metabolic syndrome, the cAMP level decreases to 3.0 pmol (3×108 cells). Preeclampsia is characterized by increased levels of fibronectin, which constantly interacts with platelets. Normally, its content is 4 mg × 109 cells. In platelets, it associates with alpha granules and is released from them after stimulation with thrombin or collagen, promoting cell adhesion by collagen. This plays an important role in the activation of the hemostatic process. Also, with gestosis, a low content of AT III is detected, which accounts for about 80% of the total primary anticoagulant activity of the blood.
Pregnant women with preeclampsia had high titers of beta-thromboglobulin and platelet factor IV. Clinicians attach an important role to the condition of the endothelium in preventing the development of excessive blood coagulation during pregnancy. The antithrombogenic properties of the vascular wall are ensured by the influence of a number of components: 1) prostacyclin, which is an inhibitor of platelet aggregation and provides a pronounced vasodilation effect; 2) anticoagulants (AT III and alpha-2 macroglobulin); 3) plasminogen proactivator produced in blood vessels; 4) thrombomodulin, formed on the surface of endothelial cells. In healthy individuals, platelets do not adhere to intact endothelium. When the endothelium is damaged, platelets easily adhere to the subendothelium, which is due to a decrease in the content of glycosaminoglycans and prostacyclin synthesized by the endothelium. The level of prostacyclin in healthy individuals during pregnancy is 65.0 pg/ml; in pregnant women with metabolic syndrome it decreases to 51.0 pg/ml.
The discovery of NO production by endothelial cells in the 80s once again confirmed the enormous morphofunctional importance of the endothelium, which was previously considered as a passive dividing surface between the blood and the extravasal space. NO has many functions, the main ones being the maintenance of normal vascular function and the full adaptation of the cardiovascular system to pregnancy. NO has vasodilating antiplatelet activity and is also an inhibitor of mitogenesis.
To determine the significance of NO levels in pregnant women in the development of blood hypercoagulation, we compared its quantitative indicators in pregnant women of the main and control groups. In individuals in the control group, the NO level is 23.2, and in individuals in the main group its value decreases to 21.16. It is very important to note that the NO level increases only 6 months after birth to 25.57. This indicates that the disruption of endothelial function is caused specifically by pregnancy. In patients with gestosis, significant damage to the endothelium occurs, hypoxia and the circulation of free radicals, as well as aggressive forms of oxygen, increase. In this case, NO is spent on binding free radicals, as a result of which one of its important functions, vasodilating and antiplatelet, suffers.
The level of AT III is significantly reduced, and this makes it possible to increase the thrombotic activity of the blood (Table 1). Added to this is a decrease in the fibrinolytic activity of the blood: if in the control group it is 20.3%, then in metabolic syndrome it decreases to 11.2%. Of particular importance is the increased sensitivity of platelets to various aggregates (collagen, adrenaline and ADP), which in various types of pathology, such as gestosis, can lead to thrombotic complications. It is also important that cAMP in platelets is reduced in pregnant women with metabolic syndrome to 3 × 108 cells pmol, while in the control group this figure is 4.1 × 108 cells pmol.
The reduced level of prostocycline (6-keto-PGF1-alpha in plasma - pg/ml) is important in matters of platelet activity; if in the control group the production of prostocycline is 65 pg/ml, then in pregnant women with metabolic syndrome the level of prostocycline is reduced to 51 pg/ml. The von Willebrand factor increases in the blood; in pregnant women with metabolic syndrome it is 2.18 units/ml, and in the control group it is 1.04 units/ml, thus enhancing the aggregation ability of platelets. Thus, the combined effect of high levels of fibrinogen and an increase in platelet aggregation activity, combined with reduced indicators such as AT III and prostacyclin, contribute to the development of thrombohemorrhagic syndrome in pregnant women with metabolic syndrome and is one of the triggers for the addition of preeclampsia.
In order to reduce perinatal risk and the incidence of other pregnancy complications, a number of patients with metabolic syndrome underwent complex therapy, which included:
- hypochloride protein diet with the inclusion of foods rich in “natural” antioxidants (prunes, raisins, blueberries, black currants);
- one of the drugs from the group of “synthetic” antioxidants: vitamin E (300 mg/day), ascorbic acid (100 mg/day), glutamic acid (3 g/day);
- preparations of the membrane stabilizer group containing polyunsaturated fatty acids: Essentiale Forte H 2 capsules - 3 times, Lipostabil 2 capsules - 3 times and the food supplement Eikonol 1 capsule 1-2 times a day;
- anticoagulant therapy (Fraxiparin 0.3 or 0.6 ml/day s.c. depending on the hemostasiogram parameters);
- antiplatelet therapy - Cardiomagnyl 75 mg/day.
The patients were treated with Cardiomagnyl 75 mg once a day and Fraxiparine 0.3–1.2 times a day. The mechanism of action of acetylsalicylic acid is based on irreversible inhibition of the enzyme cyclooxygenase (COX-1), as a result of which the synthesis of thromboxane A2 is blocked and platelet aggregation is suppressed. Fraxiparine exhibits a high ability to bind to the blood plasma protein AT III. This binding leads to accelerated inhibition of factor Xa, which accounts for the high antithrombotic potential of nadroparin. The antithrombotic effect of nadroparin includes activation of tissue factor conversion inhibitor (TFPI), activation of fibrinolysis through direct release of tissue plasminogen activator from endothelial cells and modification of the rheological properties of blood (decreasing blood viscosity and increasing the permeability of platelet and granulocyte membranes). Nadroparin calcium is characterized by higher anti-factor Xa activity compared to anti-factor IIa or antithrombotic activity and has both immediate and prolonged antithrombotic activity.
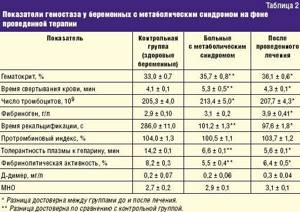
Against the background of the treatment, there was an improvement in the condition of pregnant women and a decrease in the indicators presented on the hemostasiogram, as well as an improvement in biochemical parameters in pregnant women with metabolic syndrome during the therapy (Table 2).
Thus, the functional activity of the endothelium during pregnancy (especially during gestosis) is sharply disrupted. Oxidative stress during pregnancy, especially in women with metabolic syndrome, stimulates endothelin production with the corresponding development of hypertension. Consequently, dysfunction of endothelial cells stimulates the release of endothelin, thromboxane, angiotensin II, inhibits the production of nitric oxide and leads to placental ischemia and the addition of preeclampsia (Table 1).
The outcome of pregnancy and childbirth was monitored in 58 women admitted to the department of pathology of pregnant women of the maternity hospital of City Clinical Hospital No. 70 in Moscow. The control group consisted of data from the course of pregnancy and childbirth in 15 women with metabolic syndrome.
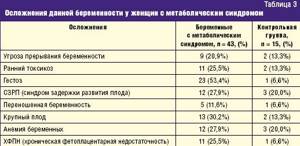
Analysis of the course of pregnancy in women with metabolic syndrome indicates that pregnancy often occurs with various complications presented in Table. 3.
Of significant interest is the analysis of the course of labor in women with metabolic syndrome. The data is presented in table. 4.
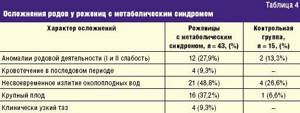
A characteristic feature of the course of labor in women with metabolic syndrome is untimely rupture of amniotic fluid, labor anomalies, a large fetus and bleeding in the third stage of labor.
Thus, in women in labor with metabolic syndrome, the average amount of bleeding was 600–900 ml (one woman in labor in this group had bleeding of 1100 ml). In all cases, the use of conservative treatment methods was ensured.
The high percentage of bleeding in parturient women with metabolic syndrome can be explained by impaired contractility of the uterus, as evidenced by the significant frequency of labor anomalies.
Of particular interest is the frequency of operative delivery in women with metabolic syndrome. If in maternity hospital No. 70 the rate of cesarean section is 22–23% over the years, then for women in our study it was 33.6%.
Indications for cesarean section were: clinically narrow pelvis, severe form of gestosis, persistent weakness of labor, not amenable to drug correction.
Thus, the incidence of metabolic syndrome in obese women was 89.2%. Metabolic syndrome adversely affects the course of pregnancy and childbirth, which is the reason for a significant increase in the frequency of surgical interventions, especially delivery by cesarean section. The analysis gives grounds to classify pregnant women with metabolic syndrome as a high-risk group for the development of gestosis and complications of labor.
conclusions
- Metabolic changes in women during pregnancy (increased blood pressure, hyperglycemia, insulin resistance) pose a risk of developing preeclampsia.
- In the pathogenesis of DIC (disseminated intravascular coagulation) in pregnant women with metabolic syndrome, damage to the vascular endothelium, increased platelet aggregation and impaired rheological properties of the blood play a role.
- To treat DIC syndrome in pregnant women with metabolic syndrome, it is necessary to include antiplatelet agents and anticoagulants in complex therapy. Carrying out complex therapy including antiplatelet agents and anticoagulants is a pathogenetically based prevention of the addition of gestosis and allows you to prevent or delay the addition of gestosis and significantly improve the outcomes of pregnancy and childbirth.
Literature
- Arkhipov V.V., Kayupova G.F., Samatova Z.A. Course of pregnancy and childbirth, condition of the fetus and newborn in obese women // Health. Bashkortostan. 1999, no. 3, p. 33–34.
- Belovitskaya N. State of the platelet-vascular link of the hemostasis system in patients with NIDDM and coronary artery disease. M., 1990, p. 144.
- Butrova S. A. Metabolic syndrome: pathogenesis, clinical picture, diagnosis, approaches to treatment // Rus. honey. magazine 2001, 2, 56–60.
- Vasilenko A. Changes in platelet and procoagulant components of hemostasis in patients with arterial hypertension // Medical Affairs. 1992, no. 8, p. 65–66.
- Ginzburg M. M., Kozupitsa Ch. S., Kryukov N. N. Obesity and metabolic syndrome. M., 2000, p. 14–15.
- Mamedov M. N. Clinical and biochemical features and ways of drug correction of metabolic syndrome. Diss. Doctor of Medical Sciences M., 2001.
- Chazova I. E., Mychka V. B. Metabolic syndrome. 2004, p. 9.
- Chernukha G. E. Clinical significance of disturbances in homeostasis indicators in obese pregnant women. Diss. Ph.D. M., 1987.
- Bernardi F., Marcheti G., Pinotti M., Arcieri P. Factor VII gene Polymorphisms Contribute About One Third of the Factor VII Level Variation in Plasma // Atherosclerosis, Thrombosis and vascular Biology. 1996, v. 16, no. 1, 72–78.
- Bray GA Obesity. Part I. Pathogenesis//West J. Med. 1988, v. 194, no. 4, p. 429–441.
- Despres JP The impact of overstate on the multifactorial risk profile of abdominally obese patients // Diabetes, 1998, 48, 1, 307.
- Edwards LE, Hellerstedt WL, Alton IR et al. Pregnancy compactions and birth outcomes in obese and normal-weight woman: effects of gestational weight change // Obstet. Gynec. 1996, no. 87 (3), p. 389–394.
- Galtier-Derenze F., Bringer Y. Maternal overweight and pregnancy // Diabetes Metab. 1997, v. 23, no. 6, p. 192–195.
- Goldenberg RL, Tamura T. Pregnancy weight and pregnancy outcome // JAMA. 1996, no. 275 (14), p. 1127–1128.
- Stico-Rahm A., Niman V., Hamsten A., Nilsson Y. Secretion of plasminogen activator inhibitor 1 from cultudef human umbilical vein endothelian cells is included by very low density lipoprotein // Atherosclerosis. 1990, 10:1067–1073.
E. I. Sokolov, Doctor of Medical Sciences, Professor, Academician of the Russian Academy of Medical Sciences I. B. Manukhin , Doctor of Medical Sciences, Professor A. A. Mochalov O. B. Nevzorov , Doctor of Medical Sciences, Associate Professor
MGMSU , Moscow
Contact information for authors for correspondence
Extreme treatment: how to increase platelets in the blood quickly?
When the level of blood cells in a pregnant woman decreases, the fastest way to get the desired effect is to correctly combine medication, folk treatment and diet. But the forum dedicated to the pathology of thrombocytopathy contains many stories about how in a short time you can actually increase the levels of this element in the blood.

This can only be done by transfusing platelet mass into the body. Before increasing the indicator and carrying out extreme treatment, the doctor must thoroughly examine the patient.
Often this method, which allows you to quickly normalize the platelet count, is necessary for people after chemotherapy. In this case, a number of additional drugs are also prescribed, since patients have elevated monocytes.
Conservative treatment of thrombocytopenia: approved drugs and nuances of treatment during pregnancy
Deviations from the norm of platelets in the blood during pregnancy occur for various reasons. They can be either minor or very serious. In the first case, doctors recommend doing without drug treatment and giving preference to safe traditional methods, while adjusting the diet.
But what to do if the cause of the pathology is more serious, for example, bleeding, hormonal imbalance or neuropathy? A critically low level of blood platelets forces the physician to prescribe a corticosteroid drug to a patient who is “pregnant.” Dexamethasone is most often prescribed in injections or tablets.
If it turns out to be ineffective, then immunoglobulin injections are prescribed. If there is a threat of miscarriage, doctors may resort to surgical treatment - laparoscopy, in which the spleen is removed. It is in this organ that the largest number of platelets are destroyed.
Traditional methods of increasing blood cells during pregnancy: 3 effective recipes
Traditional medicine will help expectant mothers normalize their indicators.
The most effective medicinal recipes that can be prepared at home include the following:
- nettle infusion Take 10 grams of herb per 200 ml of water. Mix, boil and cook over low heat for 5 minutes. Divide the drink into two doses. Take morning and evening. The course of treatment is 14 days;
- milk with nettle juice. You need to chop the fresh leaves of the plant, squeeze them through cheesecloth until you obtain juice. Mix 50 ml of milk with 5 ml of the resulting nettle liquid. You will get a single dose. Drink three times a day for a month;
- Sesame oil. Drink 1 tbsp. spoon 30 minutes before meals. Course - 4 weeks.

Traditional medicine also helps well if a pregnant woman has elevated red blood cells. In this case, it is recommended to use dill seeds. They need to be ground into flour and eaten 1 teaspoon twice a day with a glass of water. Take a course of 2 months.
Therapeutic nutrition during pregnancy: normalizing platelet levels with diet
For pregnant women, the doctor will definitely tell you which foods can further increase the level of blood platelets, and which, on the contrary, should be eaten when platelets are low in order to increase their number. The diet is based on eating foods high in vitamins and microelements.
Foods that increase platelets are:
- chicken eggs;
- lean meats;
- mushrooms;
- nuts;
- vegetables - carrots and beets predominate;
- fruits - especially pomegranate, bananas, apples and peaches;
- sea fish;
- seafood;
- greenery;
- legumes;
- dairy products.
It is necessary to exclude sausages and confectionery products, smoked and canned foods, and chocolate from the diet. The diet will also help the expectant mother keep in shape and even lose extra pounds if she is overweight. If you add to this high-quality care for your body and face, you will probably be able to avoid psychological problems.

The LUNA mini face brush will help you stay attractive while pregnant and after childbirth, as it effectively removes makeup, cleanses the skin of dirt, improves blood microcirculation and removes blackheads.
What foods can increase platelet levels?
Platelets are the cells responsible for the blood clotting process. A reduced platelet count can be restored with dietary changes. Thus, the coagulation process is normalized by foods rich in folic acid, vitamins B12, C, D, K and iron.
Folic acid
Folic acid is a synthetic form of folate. According to the National Institutes of Health (NIH), USA, the daily intake of folate for adults is at least 400 mcg, and for pregnant women - at least 600 mcg.
Foods containing folates:
- dark green vegetables such as spinach and Brussels sprouts;
- beef liver;
- black Eyed Peas;
- fortified breakfast cereals;
- yeast.
It is worth considering that excess amounts of folate obtained from fortified foods and supplements can negatively affect the absorption of vitamin B12.
Vitamin B12
This vitamin is involved in the process of hematopoiesis. A decrease in its level leads to a decrease in the number of platelets. According to the NIH, the daily requirement for vitamin B12 for adults is 2.4 mcg, for pregnant and breastfeeding women - 2.8 mcg.
Foods rich in vitamin B12:
- beef;
- eggs;
- fish, including shellfish, trout, salmon and tuna;
- dairy products.
Vegetarians can get vitamin B12 from the following foods:
- enriched breakfasts;
- soy milk;
- additives.
Vitamin C
This vitamin is involved in the regulation of immune processes, platelet functioning, and iron absorption.
Many fruits and vegetables contain vitamin C, including:
- broccoli;
- Brussels sprouts;
- citrus;
- kiwi;
- red and green peppers;
- strawberry.
It is important that vitamin C is destroyed at high temperatures, so it is better to consume the listed foods unprocessed.
Vitamin D
Vitamin D is responsible for the functioning of the immune system, bone, muscle and nervous tissue. Vitamin D synthesis occurs under the influence of sunlight. According to the NIH, the daily requirement for vitamin D for adults is 15 mcg.
Food sources of vitamin D include:
- egg yolk;
- fatty fish such as salmon, tuna and mackerel;
- fortified dairy products.
Vegetarians can get vitamin D from fortified breakfast cereals, concentrated orange juice, supplements, and mushrooms.
Vitamin K
Vitamin K is involved in blood clotting and bone metabolism. According to the NIH, the daily requirement for vitamin K for men is 120 mcg and for women it is 90 mcg.
Vitamin K Rich Foods:
- natto (fermented soybean dish);
- greenery;
- broccoli;
- soybeans and soybean oil;
- pumpkin.
Iron
Iron plays an important role in the process of hematopoiesis. According to the NIH, the daily intake of iron for men and women (over the age of 50) is 8 mg, for women aged 19-50 years - 18 mg, for pregnant women - 27 mg.
Iron-rich foods:
- oysters;
- beef liver;
- enriched breakfasts;
- white beans and kidney beans;
- dark chocolate;
- lentils.
What foods should you exclude from your diet?
Foods and drinks that can lower your platelet count:
- alcohol;
- aspartame, an artificial sweetener;
- cranberry juice;
- quinine.
Symptoms of a low platelet count include:
- dark red spots on the skin;
- headache after minor injuries;
- spontaneous or excessive bleeding;
- increased bleeding of the gums.
People who experience these symptoms should consult a doctor immediately.
Based on materials from www.medicalnewstoday.com
Hepatitis C and thrombocytopenia in a pregnant woman: what do you need to know?
When explaining to a patient in an “interesting situation” how to raise platelets and restore liver functionality with hepatitis C, the doctor must explain some of the associated points and list all the possible risks. Liver pathology is treated with injections based on ursodeoxycholic acid. This method is considered the safest in the current situation.
In patients with hepatitis C, white blood cells are elevated, which should also be taken into account when choosing treatment. Maintaining an optimal level of blood cells in a pregnant woman’s body is very important, especially for platelets. If there are too few of them, bleeding may occur, which poses a danger to the fetus during gestation and during childbirth.
Pregnancy - III trimester
A complex test, including a group of laboratory tests to determine the general health, functioning of the main systems and organs of a pregnant woman in the third trimester of pregnancy.
Synonyms Russian
Pregnancy, III trimester.
English synonyms
Pregnancy third (III) trimester.
What biomaterial can be used for research?
Venous blood, an average portion of morning urine.
How to properly prepare for research?
- Eliminate alcohol from your diet for 24 hours before the test.
- Eliminate fatty foods from your diet for 24 hours before the test.
- Do not eat for 12 hours before the test; you can drink clean still water.
- Avoid (in consultation with your doctor) taking diuretics for 48 hours before collecting urine.
- Completely avoid (in consultation with your doctor) taking medications for 24 hours before the test.
- It is recommended to collect urine before menstruation or 2-3 days after it ends.
- Avoid physical and emotional stress for 30 minutes before the test.
- Testing for HIV infection can be carried out anonymously and confidentially. During a confidential examination, it is mandatory to present a passport.
- Do not smoke for 30 minutes before the test.
General information about the study
The third (III) trimester of pregnancy includes the period between 27 (28) and 38 (40) weeks of pregnancy. During this period, active growth of the fetus occurs, improvement of organ systems, in particular the respiratory system, development of sensory organs, and maturation of the nervous system. Clinical laboratory diagnostics are aimed at assessing the functioning of major organs and systems, in particular the kidneys, liver, blood coagulation system, endocrine system of a pregnant woman, as well as controlling infection during pregnancy.
A clinical blood test allows you to evaluate the qualitative and quantitative composition of blood according to the main indicators: red blood cells, leukocytes and their varieties in absolute and percentage terms, platelets. Detection of deviations in these indicators may indicate the presence of pathological processes and diseases in a pregnant woman. A reduced number of red blood cells and the hemoglobin content in red blood cells may indicate the presence of anemia in pregnant women. This condition can lead to placental insufficiency - the main cause of miscarriage, low birth weight babies and fetal death. Changes in the leukocyte formula may indicate a wide range of changes in the body of a pregnant woman. These may be laboratory signs of inflammatory and infectious diseases, pathologies that a woman has, but have not previously been diagnosed. The platelet count during pregnancy may be lower than normal, which must be taken into account. Significant changes in these indicators and developing thrombocytopenia require special monitoring, as they may be indirect signs of pathologies of the blood coagulation system, as well as such a severe complication of pregnancy as DIC syndrome (disseminated intravascular coagulation syndrome). Changes in ESR can be observed in the presence of acute and chronic inflammatory diseases and infectious processes. A slight increase in ESR can be observed during pregnancy. This test has high sensitivity but low specificity and is prescribed in combination with other indicators.
A general urinalysis with microscopy of urinary sediment is a set of diagnostic tests that allow one to assess the general properties of urine, its physicochemical properties, the content of metabolic products, and identify the qualitative and quantitative content of a number of organic compounds. These tests reflect the functional state of the kidneys and urinary tract, allow one to judge general metabolic processes, and suggest the presence of possible disorders, infectious and inflammatory processes. The detection of glucose and ketone bodies in the urine may indicate the development of impaired carbohydrate tolerance, diabetes mellitus, and pregnancy diabetes. Detection of protein in the urine may be a sign of developing nephropathy in pregnancy; proteinuria more than 0.3 g in daily urine may indicate the development of a severe complication of pregnancy - preeclampsia. The severity of this condition varies greatly. Thus, with the development of mild preeclampsia after 36 weeks, the prognosis is usually favorable. On the contrary, the threat to the health of the mother or fetus increases significantly if preeclampsia develops early (before 33 weeks) and is aggravated by the presence of concomitant diseases.
In the third trimester of pregnancy, it is also necessary to monitor the functional state of the blood coagulation and fibrinolysis system. The prothrombin time test is used to evaluate the extrinsic clotting pathway. The following indicators are obtained as results: Quick prothrombin time and international normalized ratio. Activated partial thromboplastin time (aPTT) characterizes the intrinsic pathway of blood coagulation. Fibrinogen is factor I (the first) factor of the blood plasma coagulation system. These indicators make it possible to assess the functional state of the liver, the main pathways of the blood coagulation system, and assess the functional state of its components. Their determination is important for predicting thrombosis during pregnancy, diagnosing a complication such as disseminated intravascular coagulation syndrome, and planning the necessary therapy during childbirth - a process accompanied by massive blood loss. It should be noted that there is a physiological increase in the levels of prothrombin and fibrinogen in the third trimester of pregnancy. But a sharp increase in these indicators requires special monitoring and prescription of the necessary therapy. The level of D-dimer also increases during the physiological course of pregnancy, especially at 35-40 weeks, but a sharp increase in the concentration of D-dimer may indicate a large number of blood clots, which is most often caused by venous thromboembolism or disseminated intravascular coagulation syndrome.
Determination of such biochemical parameters as alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin and direct bilirubin fraction, total protein in serum allows us to assess the functional state of the liver. ALT levels may be slightly elevated, while AST levels are decreased. A significant increase in the concentration of transaminases may indicate the presence of liver damage, hepatitis, and the development of preeclampsia. A decrease in the level of total protein in the blood serum along with the loss of protein in the urine and with an increase in blood pressure more than 140/90 mm Hg. Art. is also a sign of developing preeclampsia.
To exclude the development of diabetes in pregnant women (gestational diabetes), the development of complications, in particular diabetic nephropathy, it is necessary to determine the level of glucose in the blood plasma.
To assess the functional state of the kidneys, in particular the integrity of glomerular filtration processes, several diagnostic parameters are used. The most important and characteristic is the determination of the levels of urea and creatinine in the blood serum, as well as the assessment of the glomerular filtration rate. It is important that creatinine levels are reduced by almost half in pregnant women due to increased blood volume, increased blood flow in the kidneys and, accordingly, an increased degree of filtration. Also, an increase in renal filtration causes a decrease in the amount of urea in pregnant women.
Typically, pregnancy occurs with normal levels of thyroid-stimulating hormone (TSH) in the blood. This euthyroid state is maintained by all components of the thyroid system and placental hormones, in particular human chorionic gonadotropin and human chorionic thyrotropin. The thyroid hormone systems of the mother and fetus are independent of each other and weakly penetrate the mature placenta. The TSH level in the blood of pregnant women may increase with the development of preeclampsia.
In the third trimester of pregnancy, it is also recommended to retest for hepatitis B - HBsAg, hepatitis C - anti-HCV, antibodies, HIV infection - HIV 1.2 Ag/AbCombo (determination of antibodies to HIV types 1 and 2 and p24 antigen), syphilis - antibodies to Treponema pallidum. The incubation period for some infections varies greatly and a negative result from tests taken early in pregnancy may change in the last weeks of pregnancy or remain negative. This is necessary to prevent infection of the fetus during childbirth, prescribe the necessary treatment or perform a planned cesarean section.
What is the research used for?
- For preventive examination of pregnant women in the third trimester of pregnancy.
- If there is a suspicion of deviations in the normal functioning of the systems and organs of pregnant women.
- To diagnose complications of the third trimester of pregnancy.
When is the study scheduled?
- Pregnant women in the third trimester at 27-38 (40) weeks of pregnancy.
What do the results mean?
Reference values
For each indicator included in the complex:
- [02-005] Clinical blood test (with leukocyte formula)
- [02-006] Urinalysis with microscopy
- [02-007] Erythrocyte sedimentation rate (ESR)
- [03-001] D-dimer
- [03-003] Activated partial thromboplastin time (APTT)
- [03-007] Coagulogram No. 1 (prothrombin (according to Quick), INR)
- [03-011] Fibrinogen
- [06-003] Alanine aminotransferase (ALT)
- [06-010] Aspartate aminotransferase (AST)
- [06-015] Plasma glucose
- [06-021] Serum creatinine (with GFR determination)
- [06-034] Serum urea
- [06-035] Total protein in serum
- [06-036] Total bilirubin
- [06-037] Direct bilirubin
- [07-009] anti-HCV, antibodies
- [07-025] HBsAg
- [07-032] HIV 1.2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
- [07-049] Treponema pallidum, antibodies
- [08-118] Thyroid-stimulating hormone (TSH)
What can influence the result?
- The use of medications, in particular hormonal ones.
Who orders the study?
Obstetrician-gynecologist, general practitioner, endocrinologist, therapist, infectious disease specialist.
Literature
- Dolgov V.V., Menshikov V.V. Clinical laboratory diagnostics: national guidelines. – T. I. – M.: GEOTAR-Media, 2012. – 928 p.
- Moon HW, Chung HJ, Park CM, Hur M, Yun YM1. Establishment of trimester-specific reference intervals for thyroid hormones in Korean pregnant women / Ann Lab Med. 2015 Mar;35(2):198-204.
- Angueira AR, Ludvik AE, Reddy TE, Wicksteed B, Lowe WL Jr, Layden BT. New insights into gestational glucose metabolism: lessons learned from 21st century approaches. / Diabetes. 2015 Feb;64(2):327-34. doi: 10.2337/db14-0877.
- Poon LC, Nicolaides KH. Early prediction of preeclampsia. Obstet Gynecol Int. 2014;2014:297397. Review.
- Fauci, Braunwald, Kasper, Hauser, Longo, Jameson, Loscalzo Harrison's principles of internal medicine, 17th edition, 2009.