A blood test after chemotherapy is very worrying for the patient, but it is not the fact of collecting blood that is frightening - it is always done the same way and according to the laboratory standard; what is troubling is the possible result that determines the patient’s life for the next two weeks and the prospects for the next course of chemotherapy.
Women endure chemotherapy with more pronounced complications in the blood, the male body reacts less to the toxicity of therapy, for which no explanation has yet been found, and traditionally they have “turned the needle” on sex hormones.
- Blood after chemotherapy
- How to increase white blood cells after chemotherapy?
- How to increase hemoglobin after chemotherapy?
- How often should you have a blood test?
- How to prepare for a blood test after chemotherapy?
- Contraindications to chemotherapy
Blood after chemotherapy
The use of most cytostatics has an adverse effect on the patient's hematopoiesis; some drugs kill more blood cells, while others, like vinca alkaloids, have almost no effect on the analysis. For each anticancer drug, the percentage of probability of a severe drop in leukocytes is determined, but the use of combinations of drugs, more than once over several weeks, eliminates all predictions for a successful outcome - undergoing chemotherapy without losses to hematopoiesis.
Not all blood cells are damaged equally by cytostatics; the most affected are leukocytes, which are not prepared by nature for a long life - their lifespan is slightly less than two weeks, and therefore are not resistant to the vicissitudes of antitumor treatment.
Platelets live a little less, but an acceptable level is maintained by a large number - they are 30-40 times more numerous than leukocytes. Thrombocytopenia - a decrease in platelet count below 150 thousand develops with the use of a small number of cytostatics, for example, thiophosphamide, often begins along with leukopenia, but normalization of the platelet count is delayed for several weeks after completion of the chemotherapy cycle. The critical platelet level is 32-34 thousand, when the risk of bleeding increases significantly.
Red blood cell - an erythrocyte should live for almost 120 days, only after 3-4 months it will be replaced by a young cell from the bone marrow, so it is more resistant to chemotherapy and 2-4 million of them circulate throughout the body. Anemia - a decrease in hemoglobin and the number of red blood cells is characteristic of a very small number of cytostatics; as a rule, several cycles of chemotherapy with platinum derivatives lead to it. The consequences of anemia are fatal - not only does the quality of life deteriorate, but life expectancy decreases and sensitivity to drug treatment changes, and in case of deep anemia, chemotherapy is contraindicated even to save life. The peculiarity of post-chemotherapy anemia is the normal iron content, that is, it is not iron deficiency, but is associated with insufficient reproduction of the red blood cell population.
The resistance of the erythrocyte membrane to external influences, including chemotherapy, determines the rate of their precipitation, verified by the reaction of erythrocyte sedimentation in a test tube in 60 minutes - ESR . ESR increases with defects in red blood cells, chemotherapy can deform the red blood cell, but it is the reproduction of blood cells in the bone marrow that suffers most from cytostatics. In most cases, ESR after chemotherapy does not change very much relative to the initial indicator and often parallels the hemoglobin content in the erythrocyte. Contrary to popular belief, ESR reacts little to the course of cancer, but actively changes during inflammation or infection, which often accompany a common malignant tumor. High ESR is often combined with anemia.
Leukocytes , composed of five fractions: neutrophils, eosinophils, lymphocytes, monocytes and basophils, react most actively to chemotherapy The most sensitive to cytostatics are neutrophils ; in a blood test they are designated as band and segmented leukocytes. Normally, there should be at least 1500 neutrophils, that is, at least half of all leukocytes; they are responsible for resisting the immune system against inflammation and infection.

The decrease in the fraction of lymphocytes , represented by the main immune defenders T-lymphocytes and immune memory cells B-lymphocytes, after chemotherapy is often not obvious and not as striking as neutrophils. Severe lymphopenia is characteristic of severe immune disorders, including HIV/AIDS. After chemotherapy, patients note a slight increase in the incidence of viral respiratory infections, but no research has been conducted on the problem, and it is not known how true the personal impression is. It is assumed that with successful chemotherapy of a malignant tumor, immunity indicators only improve.
Blood transaminases - ALT and AST do not reflect the effect of antitumor drugs on cellular fractions of the blood, but the damaging effect of cytostatics and immuno-oncological drugs on liver tissue. Chemotherapy drugs lead to toxic hepatitis, and immune antitumor drugs lead to autoimmune hepatitis. Hepatitis can be asymptomatic and manifest only by changes in transaminase levels, and depending on the severity of liver damage, ALT can increase three times and even more than 20 times the upper limit of normal.

Symptoms of thrombocytopenia
Thrombocytopenia increases the risk of life-threatening symptoms for the patient. Symptoms are more pronounced if the level of platelets is reduced, more than three times the standard. The norm is 180-320 x 109/l for men and women. A sudden and noticeable decrease in components in the blood is characterized by the indicator:
- gum bleeding for a long time;
- blood oozes systematically and intensely from the nose;
- increase in the duration of menstruation in women;
- increased size of the spleen;
- sudden formation of bruises;
- the appearance of petechiae - small red dots on the epidermis;
- there are feces with bloody manifestations, urine with blood clots;
- pain in the muscular and joint systems;
- cough and vomiting with blood;
- secretion of blood in hemorrhoidal areas;
- bleeding in the stomach and intestines.

The patient is not always notified of the development of thrombocytopenia while taking potent drugs. At the initial stage, the problem does not show symptoms. Due to the chemotherapy procedure, platelets and white blood cells drop, increasing the likelihood of developing diseases. Complications lead to a poor prognosis. The outcome in such cases is often fatal. Knowledge of methods for increasing hemoglobin in the blood if platelet volumes have fallen will help the patient prevent an unpleasant list of consequences.
How to increase white blood cells after chemotherapy?
White blood cells, namely neutrophils, after chemotherapy can decrease to a critical level, which results in severe infections. A special form of a generalized inflammatory reaction after chemotherapy is febrile neutropenia, when nothing but a high temperature and a serious condition is found in the patient: there are no objective signs of sepsis, pneumonia and inflammation of other organs. The blood test does not find any pathological microflora - everything is sterile, only there are fewer neutrophils than normal, and the percentage may remain the same.
Neutropenia is divided into degrees as follows:
- the absolute number of cells is from one and a half thousand to a thousand, which does not exclude the development of febrile neutropenia after chemotherapy, that is, a single increase in temperature of more than 38.5℃ or twice in one day more than 38℃
- average degree from a thousand to 500 cells;
- severe neutropenia or agranulocytosis, that is, the absence of granulocytes - a drop in the neutrophil level below 500.
Stimulation of leukopoiesis is necessary only for febrile neutropenia; an asymptomatic decrease in the leukocyte fraction requires correction only in patients weakened by multiple chronic diseases.
The only effective drugs are colony-stimulating factors (CSF), there are several types of them, primarily aimed at stimulating the sprouts of white hematopoiesis. The drugs activate an increase in fertility and the rate of maturation of neutrophils in the bone marrow; with the initial use of CSF in a blood test, the result is visible within a few hours.
No other drugs, except CSF, affect the reproduction of leukocytes, but only promote the rapid removal of deposited leukocytes from the bone marrow, depleting hematopoietic resources. The number of white blood representatives is not affected by the patient’s diet or any procedures.
The use of hematopoietic stimulants is not only accompanied by unpleasant side reactions, but over time also depletes bone marrow reserves, so strict indications have been defined for CSF. CSF is never combined with chemotherapy; the drug is administered the next day after the cytostatic.
Treatment/prevention
First of all, you need to determine the cause of your thrombocytopenia. As you understand, in addition to chemotherapy, a decrease in platelet levels can be caused by other reasons that require a different treatment approach. For example, if the thrombocytopenia is caused by chemotherapy, the treatment plan usually includes delaying the next administration of anticancer drugs, whereas if the drop in platelets is due to immunology, corticosteroids are usually prescribed.
Whether or not your doctor recommends one way or another to correct low platelets depends on the severity of your thrombocytopenia and whether you have any symptoms. Options:
Transfusion of platelet concentrates
Platelet transfusion is the most common method of correcting chemotherapy-associated thrombocytopenia, especially short-term drops in platelet levels. Blood transfusions can be used as treatment (to increase platelet counts in those who are actively bleeding) or as a prophylaxis (for those who are low but are not bleeding).
The most common side effect of the procedure is an increase in body temperature. Also possible: blood transfusion reaction or transmission of infections, such as hepatitis C.
Delaying chemotherapy
Sometimes chemotherapy may need to be delayed or the dose adjusted.
Medicines that stimulate platelet production
There are drugs whose action is aimed at stimulating the bone marrow, which allows raising platelets, although they are often used to correct thrombocytopenia in cancer patients (at present there is insufficient data on the benefits of their use in oncology). Your doctor may recommend Neumega, Nplate, or Promacta to restore platelet levels.
Clinical researches
The search for other methods of correcting chemotherapy-induced thrombocytopenia continues.
Complementary medicine methods
There is currently no proven evidence that alternative medicine or dietary supplements have any effect on platelet recovery. However, vitamins such as vitamin B12 and folate and minerals such as iron are essential for the production of healthy platelets, so a balanced diet rich in these nutrients is important in restoring platelet levels that have been reduced by chemotherapy.
How to increase hemoglobin after chemotherapy?
As a rule, anemia develops after multiple courses of chemotherapy and in most cases does not require urgent measures in the form of red blood cell transfusion, as is necessary in case of heavy bleeding.
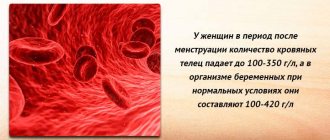
According to the severity of anemia, it can be:
- mild - hemoglobin at a level of 100-119 grams per liter, as a rule, has almost no effect on well-being if the patient does not have a very common cancer process;
- average degree with hemoglobin 80-99 g/l, the lack of oxygen transported to the tissue is manifested by a decrease in the functional capabilities of the body, shortness of breath during physical exertion and weakness with rapid fatigue are possible;
- anemia becomes severe when the hemoglobin level decreases beyond 80 grams per liter of blood; well-being mainly suffers, but objective disorders of the cardiovascular system are also possible.
Hemoglobin levels are increased with injections of erythropoietins; treatment is started in severe cases. An increase in hemoglobin is noted after several months of treatment in only 60-70% of patients; erythropoietins are especially effective for anemia during chemotherapy with platinum derivatives.

Treatment of anemia is long-term - several months and often involves injections of iron preparations. There is no clear understanding of whether erythropoiesis stimulants change the quality of life for the better, but the use of erythropoietin is also associated with side effects, especially unpleasant and dangerous - increased blood clotting with the formation of blood clots. Due to the likelihood of thrombosis, the stimulator is contraindicated in patients with limited physical activity and a history of thrombosis, and cannot be combined with CSF and some cytostatics.
How to raise platelets
• Prednisone. This drug belongs to the class of steroids and has some similarities with another hormone - cortisone. It has a large number of indications, one of which is immune thrombocytopenic purpura. The positive effect in this case is caused by the calming effect of prednisone on an overactive immune system, which helps to raise platelets. The use of this drug by patients with HIV infection is problematic, since it suppresses the already reduced activity of their immune system. • Gamma globulin. This drug is usually used in combination with prednisone, but can also be prescribed as an independent drug. Its drip administration is carried out over 4-6 hours, once every 1-3 days. • Anti D globulin is prescribed only to some patients suffering from thrombocytopenic purpura. It is used in the form of intravenous injections, its mechanism of action is that it prevents the destruction of Bizzocero plaques by the spleen. • Removal of the spleen or splenectomy. In cases where platelets are attacked by autoantibodies, the spleen has to destroy them. But this method is used only in extreme cases, when less radical methods of treatment have not brought results.
How often should you have a blood test?
Blood tests - general with leukocyte count and platelets, as well as detailed biochemical tests - must be done before each cycle of chemotherapy. With a long cycle with weekly drug administration, the neutrophil level should be checked on the eve of administration, because the leukocyte level begins to decrease 7-10 days after the first injection of the cytostatic.
The time for performing a control blood test after chemotherapy is based on the initial state and the combination of cytostatics used, that is, always individually, but no later than 5-7 days after completion of chemotherapy. Further monitoring depends on the depth of neutropenia; daily monitoring of indicators is not excluded. If your white blood cell count is normal, the next test is scheduled before starting chemotherapy.
General recommendations
Often, after completion of chemotherapy for cancer, an independent process of tissue restoration, especially platelets, is possible. However, it will take a long time for the cells to fully recover. Regarding long-term adverse reactions, including changes in blood structure, the consequences of the procedure persist in patients until the end of their lives.
Patients experiencing thrombocytopenia are advised to follow these rules:
- It is important to avoid injury to the body; even small cuts are dangerous.
- Before the onset of menstruation, women will have to take medications that inhibit the onset of the next menstrual cycle.
- To enhance the protective functions of the gastric mucosa, it is recommended to take Omeprazole and similar drugs.
- Among toothbrushes, experts advise choosing models with soft bristles.
- At home, it is recommended to provide the patient with a soft environment; surrounding objects should be made of soft materials.

- It is especially important to carefully clear your sinuses. To do this, it is recommended to blow them lightly, without harsh impacts, in order to avoid damaging the integrity of the tissues.
- When shaving, it is recommended to give preference to electric razors.
- Taking aspirin and anticoagulants is prohibited.
- It is important to avoid the use of medicinal products containing acetylsalicylic acid.
- You should refrain from physical exercises that have an increased risk of injury.
- You should not leave the house during icy conditions.
- It is prohibited to consume alcoholic beverages and medications without first consulting a doctor.
If you get cuts, you need to apply a pressure bandage and use a special sponge to stop the bleeding. To stop nosebleeds, you can use Naphthyzin. Compliance with the above recommendations will help restore platelet volume in children and adults.
How to prepare for a blood test after chemotherapy?
For greater reliability of the indicators, any blood test is taken on an empty stomach and preferably in the morning after an 8-hour break for food. Before the analysis, you must refrain from smoking for a couple of hours. Other restrictions are determined by the treating chemotherapist.
In a blood test, all indicators that deviate from the norm are important, because each reflects some pathological changes in the body. Errors in the reliability of the indicators are possible, but we must take into account that changes in the number of blood cells are not only daily, but also hourly, the bone marrow does not have breaks for lunch and weekends, it works every second, giving birth to new cells and growing them for release into the bloodstream .
Fluctuations in biochemical parameters are more stable, since they reflect the state of organs and entire organ systems, so the study is done monthly, if there is no reason to look more often.
Glucocorticoid therapy
The use of glucocorticoids also helps raise platelets in the blood. Moreover, the effectiveness of a particular dose can only be determined empirically. Therefore, a dose of 1.5 mg/kg cannot be considered more effective than a dose of 0.5 mg/kg. At the beginning of treatment for an adult patient, the dose of prednisolone is 40-80 mg per day, 15 mg is administered every 6 hours.
Other glucocorticoids do not have clear advantages over prednisolone. For intravenous administration, hydrocortisone should be preferred, which is prescribed at 200-300 mg per day for 3-4 weeks until complete or partial remission occurs. Remission is partial if the bleeding has stopped, but platelets in the blood have not been significantly increased.
After achieving remission, the dose of the drug can be quickly reduced - reducing by 5 mg per day and increasing to 30-40 mg. After this, the daily dose is reduced more slowly - 2.5-5 mg per week.
Contraindications to chemotherapy
Antitumor treatment is inherently toxic - chemotherapy kills any cells, and not all normal tissues are able to resist cytostatics.
In each clinical case, the time of administration of the chemotherapy drug and its dose are determined individually, based on many criteria. Formally, chemotherapy cannot be started if the leukocyte level is below the standard norm, but with neutrophils above 1500 there is not always a need to reduce the single dose of chemotherapy. And with a lower level of neutrophils, it is possible to continue treatment, but with careful and regular monitoring of indicators and with the presence of CSF in reserve.
The lower limit for starting chemotherapy for platelets is above 100 thousand, for hemoglobin - above 90 g/l; on an individual basis, these limits can be lowered by changing the dose of the administered cytostatic and the intervals between injections. Of course, an average degree of decline, and even more so a severe one, is a contraindication for chemotherapy, but it is temporary - until recovery.
Of course, the veracity of the indicators, especially in the process of antitumor treatment, depends on the available laboratory equipment and the quality of the reagents; the speed of the study plays an important role. In our clinic, any research corresponds to the level of an expert opinion, otherwise our employees simply do not know how to work.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Lugovskaya S.A., Morozova V.T., Pochtar M.E., Dolgov V.V. /Laboratory hematology// M.: Publishing house. Unimed-press; 2002.
- Orlova R.V., Gladkov O.A., Zhukov N.V., et al. /Practical recommendations for the treatment of anemia in malignant neoplasms // Malignant tumors: Practical recommendations RUSSCO #3s2, 2021 (vol.


- Oganesyan A.A., Garbatsevich M.S., Kostyukovich D.I. and others /ESR: old test, new opportunities // Lab. diagnostics. Eastern Europe; 2012; No. 4.
- Protsenko S. A., Antimonik N. Yu., Bershtein L. M., et al./ Practical recommendations for the management of immune-mediated adverse events // Malignant tumors: Practical recommendations RUSSCO #3s2, 2021 (vol. 8).
A few words from OncoInfo
A decrease in platelet count that occurs during chemotherapy can often be managed conservatively, that is, by paying attention to symptoms and avoiding situations that may trigger bleeding. However, sometimes, in order to cope with the resulting thrombocytopenia, it is necessary to resort to platelet transfusions.
List of sources used:
- Weycker, D., Hatfield, M., Grossman, A. et al. Risk and Consequences of Chemotherapy-Induced Thrombocytopenia in US Clinical Practice 2019
- Kuter, D. Managing Thrombocytopenia Associated with Cancer Chemotherapy. Oncology (Williston Park). 2015
Nutrition in the fight against cancer
The diagnosis of cancer is no longer a death sentence. Modern treatment is more successful than what it was 20-30 years ago.
Oncological diseases are accompanied by many changes in the human body. These changes may be the body's response to the tumor and the side effects of drug treatment. In addition, side effects of treatment, such as nausea or changes in taste, often cause loss of appetite or inability to eat enough food. In this regard, products for oncology must be carefully selected and, in some cases, prepared in a special way.
Cancer patients face the problem of not being able to eat enough food to meet the nutritional needs of the body, which leads to weight loss.
Most often, weight loss is a consequence of lack of appetite and/or a side effect of treatment.
In overcoming cancer, the main goal is to maintain an adequate weight and consume healthy foods that provide the body with calories and nutrients.
Eating a balanced diet that includes essential foods before, during and after treatment will help you feel better and recover better. This explains why it is important to eat only healthy foods if you have cancer.
Insufficient intake of calories and/or nutrients such as protein, vitamins and minerals is a common problem in the nutrition of cancer patients. Protein and calories are important for providing the body with energy, fighting infection, and therefore for a speedy recovery. Your diet during chemotherapy, as well as your diet after chemotherapy, deserves utmost attention.
Specialized nutrition is specifically designed for cancer patients.
Consultation on modern specialized nutrition products can be obtained from a doctor.
In most cases, treatment of cancer is complex or includes one of the following stages - surgery, chemotherapy and radiotherapy.
During chemotherapy or radiotherapy, consumption of usual food in the same quantities may be difficult due to lack of appetite, impaired sense of taste and perception of smell.
Regular food seems less attractive to you and, as a result, you eat it less. The body no longer receives sufficient support to fight the disease. Take nutrition seriously during radiotherapy and chemotherapy: choose food that will meet the body's needs even in small quantities. Dietary problems you experienced before your diagnosis may be exacerbated by the cancer itself and intensive treatment.
Using specialized nutrition before starting any type of therapy will improve your condition, and in case of surgery, it will speed up the healing of surgical wounds and reduce the risk of postoperative complications.
Surgical intervention
- The tumor is removed surgically.
- Surgery can be combined with a course of chemotherapy or radiotherapy.
- After surgery, a recovery period is required in the hospital, and then at home.
Surgery is stressful for the entire body. The body's need for nutrients and energy increases.
The choice of food products during oncology should be adjusted. It is necessary to take increased amounts of nutrients, especially protein, which plays an important role in the recovery process, especially in wound healing and fighting infection.
Choose foods high in protein and calories (eg eggs, cheese, whole milk, nuts, poultry and fish). However, remember that even very good, complete foods can be poorly absorbed due to impaired absorption and digestion, especially after operations on the gastrointestinal tract.
An alternative or addition to your regular diet can be specialized nutrition (Nutrizon, Nutridrink, Nutridrink Compact), which ensures easy and rapid absorption of all necessary nutrients. Talk to your doctor about the specialized nutrition you need. Properly selected food products for oncology will facilitate the body’s recovery process and speed up recovery.
Radiation therapy
- X-rays and other types of radiation are used to destroy cancer cells.
- Radiotherapy can be used on its own or in combination with surgery and chemotherapy.
Radiation therapy may cause problems in eating normal foods, especially when the digestive organs are exposed to radiation. Some side effects appear: dry mouth, nausea, vomiting, diarrhea, constipation.
In some cases, side effects may contribute to loss of appetite, difficulty swallowing, and the inability to eat solid food due to the development of stomatitis and mucositis.
Modern specialized nutrition (Nutrizon, Nutridrink, Nutridrink Compact) will help solve these difficulties and provide the body with all the necessary nutrients. Talk to your doctor or dietician about how to properly manage your cancer diet during radiation therapy to ensure a speedy recovery.
Chemotherapy
- Special chemicals are used to destroy cancer cells.
- Chemotherapy is often used in combination with surgery and/or radiotherapy.
- Chemotherapy can be accompanied by side effects, the severity of which depends on the type and dose of drugs used and the condition of the body.
Although the side effects of chemotherapy vary and depend greatly on the type and dose of drugs used, side effects such as nausea, vomiting, fatigue, diarrhea, and constipation are common. In addition, some medications contribute to changes in taste sensations, which leads to a complete aversion to food.
Carrying out the prescribed course of chemotherapy in full is the basis for the success of treatment. A side effect of chemotherapy may be loss of appetite.
Reducing the amount of food consumed leads to insufficient supply of nutrients to the body. The result is weight loss or other disruptions in the functioning of the entire body, which may lead to interruption of the course of chemotherapy and, consequently, a decrease in the effectiveness of treatment. Therefore, eating regularly during chemotherapy is very important.
In some cases, eating regular food becomes insufficient to meet the daily requirement. In such cases, it is important to choose the right additional nutrition during chemotherapy. Modern specialized nutrition products (Nutrizon, Nutridrink, Nutridrink Compact) will help prevent weight loss and maintain overall nutritional status, which, in turn, will help to endure the disease and recover after difficult treatment.
If you feel that you are unable to take in adequate amounts of regular food, consult your doctor or dietitian. A properly selected diet during chemotherapy will help avoid unwanted consequences that can be caused by this method of treatment.
- Eat small meals, but often.
- Reduce the amount of liquid you drink during meals, and instead drink between meals.
- Eat at a time when you have a good appetite - some patients find that their appetite is better in the morning.
- Have something on hand that you can snack on at any time.
- Drink liquids (soup, juice) instead of solid foods.
- Choose high-calorie foods (such as nuts) to increase the supply of nutrients in a small amount of food.
- Modern specialized nutrition products - Nutridrink, Nutridrink Compact, Nutrizon - will help provide complete and balanced nutrition.
- Eat food that you think looks attractive and smells good.
- If a certain type of food tastes or smells strange, choose an alternative.
- Use marinades, sauces, mayonnaise or small amounts of seasonings to impart the desired flavor to food.
- The following will help reduce the smell of food: using a lid during cooking; using a kitchen hood; serving food at room temperature.
Food products that are usual in the diet for oncology are steamed, boiled, stewed, and for mucositis they are served pureed.
Diet
Food is taken in small portions in a warm (not hot!) form (40-50°C). Eating small, frequent meals helps overcome nausea and eases the gastrointestinal tract. Ice cream, sucking on pieces of ice and lemon also help with nausea.
Below is information about which foods can be eaten during oncology, indicating the recommended method of preparation.
Bread and flour products
Recommended: dry biscuit, soft biscuits, baby cookies, cookies soaked in milk, kefir or weak tea. Excluded: rye bread, fresh bread, pancakes, pies, pies, baked goods.
Meat and poultry
Recommended: lean meats (beef, veal, rabbit) without tendons and fascia, chicken and turkey without skin, boiled or steamed, for mucositis - pureed (cutlets, dumplings, meatballs, puree, soufflé, roll, etc.), and steamed tongue and liver. Excluded: fatty and stringy varieties of meat and poultry, fried and stewed, canned food, products with dough (dumplings, khinkali, etc.).
Fish
Recommended: low-fat types without skin, in pieces or in the form of cutlet mass, boiled or steamed, without bones (sorted). Excluded: fatty species (sturgeon, stellate sturgeon, etc.), smoked, salted, fried, stewed, fish with bones.
Eggs
Recommended: in the form of a steam omelette. Excluded: hard-boiled, fried eggs and scrambled eggs, raw egg whites.
Dairy
Recommended: children's cottage cheese, cottage cheese in dishes (casserole, puddings), yoghurts, any dairy products intended for children (in original packaging) Excluded: dairy products with high acidity, for mucositis - fatty dairy products, sharp cheeses.
Fats
Recommended: refined olive and sunflower oils added to dishes. Butter on sandwiches and in dishes should only be consumed if there is no mucositis and should not be consumed if your child is receiving asparaginase. Excluded: other fats, overcooked butter.
Cereals, pasta and legumes
Recommended: porridges cooked in milk or water - semolina, well-cooked rice, pureed buckwheat and oatmeal. Steam puddings, souffles, cutlets from ground cereals. For mucositis, exclude: millet, pearl barley, barley, buckwheat (kernel), legumes, whole pasta.
Vegetables
Recommended: beets, potatoes, carrots, cauliflower, green peas, boiled in water or steamed and pureed (mashed potatoes, soufflé); steam puddings; zucchini and pumpkin, cut into pieces, boiled. Excluded: other vegetables, salted, pickled, pickled vegetables and mushrooms, canned vegetables.
Soups
Recommended: from pureed or very finely chopped vegetables, dairy, cereal, pureed vermicelli or homemade noodles (finely chopped) with the addition of permitted vegetables; creamed milk soups, made from vegetables, from pre-cooked chicken or meat, in weak (half-and-half) broth. Season with butter and non-acidic sour cream. Excluded: strong meat, chicken, fish broth, mushroom and strong vegetable broths, borscht, cabbage soup, okroshka.
Fruits, sweet dishes and sweets
Recommended: ripe sweet fruits and berries in the form of purees, jelly, jellies, mousses, mashed compotes; baked apples (without skin); sweet dishes with whipped proteins (mousses, sambuca), jelly, jams and preserves from sweet berries and fruits, ice cream (can only be consumed if there is no mucositis, and should not be consumed if your child receives asparaginase). Excluded: raw and unripe berries and fruits (except for mashed bananas and sour apples), chocolate, halva, and ungrated dried fruits.
Sauces and spices
Recommended: milk, sour cream, egg-butter sauces. Finely chopped dill for soups, vanilla. Excluded: other sauces and hot spices. It is recommended to limit salt intake.
Beverages
Recommended: weak tea with milk or cream, weak cocoa with milk, sweet fruit and berry juices, rosehip decoction, dried fruit compote (without whole dried fruits). Specialized ready-to-use sterile nutrition Nutridrink Compact. Excluded: kvass, coffee, carbonated drinks, juices of sour berries and fruits, homemade juices.
Children have their own specific needs for energy and proteins - they are higher than those of an adult, and therefore nutrition during treatment with chemotherapy, radiotherapy or surgery will be different. During chemotherapy, the child’s need for energy and protein increases - this is due to the fact that healthy cells, also suffering from the drugs, need material for restoration. Therefore, proper nutrition is a very important part of treatment.
| Proper feeding of a child helps the child in treating and preventing the development of many serious complications, which, at times, can suspend the progress of therapy, or even completely interfere with treatment. That is why it is extremely important to include healthy foods in a child’s diet if they have cancer. Dear parents, following these dietary recommendations is the key to your child’s well-being during chemotherapy and overcoming its complications! The liquid is consumed without restrictions (unless otherwise prescribed by the doctor). However, it should be remembered that water and tea are not food. The child's diet should contain more dairy products and natural juices. “Empty” liquid should be avoided. Try to use healthy products for oncology in cooking. It is necessary to completely exclude chips, crackers, nuts and fast food restaurant food from the child’s diet. These products irritate the mucous membrane of the gastrointestinal tract and do not contain protein and other nutrients that are beneficial for the child. They can trigger mucositis! Dried fruits and nuts must be washed and heat treated, i.e. used for making compotes, pies, etc. The use of seeds is strictly prohibited - this leads to the development of stomatitis and infectious complications in the oral cavity. |
For one serving of puree, porridge, sauce, add 1-2 tbsp. spoons of specialized nutrition Nutrizon dry mixture or 50 ml of liquid mixture Nutrini, Nutrizon, Nutridrink Compact. This will help provide the child’s body with the necessary protein and energy.
If the child refuses regular food, offer formula for specialized nutrition in small portions throughout the day. The calculation of the necessary specialized nutrition during treatment with chemotherapy, radiotherapy or surgery is carried out by the doctor, taking into account the age and weight of the child, as well as his needs for energy and protein.
| If the oral mucosa is affected, it is recommended to take the nutritional mixture in the form of a drink through a pacifier or straw. For this purpose, the optimal products are Infatrini, Nutrini, Nutridrink Compact. |
For children from 0 to 12 months.
Infatrini is a liquid ready-to-use specialized mixture, 100 ml bottle.
From 1 year to 6 years
Specialized liquid ready-to-eat products called Nutrini are registered for this age group:
- Nutrini bottle 200 ml, package 0.5 l;
- Nutrini energy bottle 200 ml, package 0.5 l;
- Nutrizon dry mixture is also approved for use in children over 1 year of age.
From 6 years and older
Ready liquid:
- Nutrizon package 1 l., bottle 0.5 l;
- Nutrizon energy package 1 l., bottle 0.5 l;
- Nutridrink Compact portion pack with straw, 125 ml;
Dry:
- Nutrizon dry mix
What is specialized nutrition Nutridrink Compact?
Nutridrink Compact is a convenient, ready-to-drink food in sterile portion packaging, in the form of a high-calorie, high-protein drink, 5-7 packages of which provide the body’s daily nutritional needs. Each package contains all the necessary nutrients and is therefore suitable as food for chemotherapy, radiotherapy and surgical treatment.
- Normalizes weight and increases physical activity due to high energy saturation (2.4 kcal/ml).
- Quickly and effectively restores damaged organs and tissues, having a high protein content (14.4 g/100 ml), which is easily digestible even with digestive disorders.
- Helps improve immunity due to its balanced composition and the presence of polyunsaturated fatty acids.
- Provides complete, balanced, sterile nutrition when the usual diet is not available or supplementation is necessary.
- Taking Nutridrink Compact before, during and after treatment helps the body prepare for treatment, increases the chances of successful treatment and recovery after treatment.
How to use Nutridrink Compact?
Nutridrink Compact should be taken in small sips through a straw, slowly, for 20-30 minutes. It can be consumed chilled, which often makes its taste even more pleasant, and, most importantly, reduces pain during stomatitis.
At what age can Nutridrink Compact, Nutridrink be used?
These products can be used from 3 years of age.
At what time of day should specialized nutrition be used?
- If specialized nutrition is a 100% replacement for regular nutrition, it makes sense to consume it during your usual meal times.
- If this food serves as a supplement to your main diet, consume it between meals or as part of your regular meals.
Are there specialized foods with a neutral taste?
Liquid, ready-to-eat products in sterile packaging Infatrini, 100 ml bottle, Nutrini, Nutrini Energy, Nutrini with PV, 200 ml bottle, Nutrizon and Nutrizon Energy, 500 ml bottle, have a neutral taste and are convenient for oral use.
How long should I use specialized nutrition?
It is recommended to continue taking specialized nutrition until appetite normalizes, eating regular food becomes easier, and indicators such as the patient’s weight, total blood protein, hemoglobin, etc. stabilize. However, the duration of taking specialized nutrition should not be less than 4 weeks. Only in this case can a stable positive effect be obtained.
The combination of ready-to-use specialized products in sterile portion packaging in the diet means a variety of diets, improved treatment results, and an improved quality of life. Choose only healthy foods to eat if you have cancer.
Use in combination
Any combination of specialized products will diversify your daily diet. Calorie and protein needs vary from person to person. Adequate compensation for your needs will lead to a positive result. Diet after chemotherapy is also an integral part of the fight against the disease.
There are contraindications: age from 0 to 3 years, increased bleeding, galactosemia, intolerance to product components. Before use, you should consult a specialist.
Nutricia is a leader in the development of nutrition for cancer.