MRI scanning is a highly informative diagnostic procedure that is not associated with the effects of ionizing radiation. The method is based on the principle of magnetic resonance and computer data processing. Images of internal organs and structures of the region of interest consist of many cross-sections with a thickness of 1 mm. The radiologist can examine a photo of the pathological area in an enlarged form, in different planes.
Magnetic resonance imaging of a woman's reproductive organs
MRI of the pelvis is harmless for people who do not have metal implants in the body. In gynecological and urological practices, magnetic resonance imaging is performed to diagnose a number of diseases with different pathogenesis. According to indications, mainly to identify tumors, the study is performed with contrast. Intravenous administration of a gadolinium-based drug improves imaging capabilities.
Magnetic resonance scanning, compared to CT scanning, is more informative for detecting the slightest changes in soft tissues.

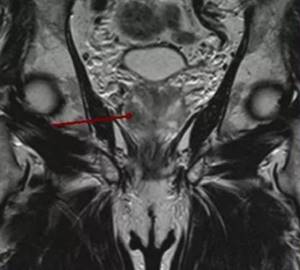
Polycystic ovary syndrome (arrows)
What does a pelvic MRI show:
- benign, malignant neoplasms, metastases;
- cysts;
- stones in the prostate, bladder;
- inflammation and complications;
- foreign bodies;
- injuries and damage during medical procedures;
- developmental anomalies of the internal genital organs and lower parts of the urinary system;
- circulatory disorders;
- lymphadenopathy;
- changes in the musculo-ligamentous apparatus;
- pathologies of bone structures (hip joints, pubic symphysis, sacrum, etc.).
Diseases of the pelvic organs
Uterine cancer on MRI
A number of pathological processes accompany persistent pain in the lower abdomen, in the perineum. The initial method of examination in gynecological and urological practices is ultrasound sonography. Magnetic resonance scanning is prescribed:
- with unsatisfactory results of ultrasound, radiography, CT;
- for differentiating benign and malignant processes, staging cancer;
- before preparing for surgery;
- to assess the effectiveness of treatment;
- as part of dynamic monitoring of the disease/early detection of relapses of tumor processes;
- to determine biological sex in case of ambiguous genitalia.
What does MRI of the pelvic organs show in women? The study is often used to exclude/determine the stage of malignant tumors of the uterus and cervix, ovaries, and bladder.
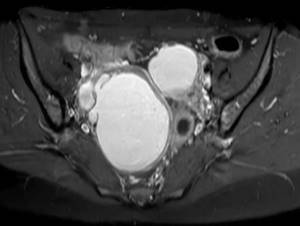
Ovarian adenocarcinoma
MRI scan demonstrates:
- cysts of the appendages and the nature of the origin of the formations;
- endometritis, salpingoophoritis, pelvic abscesses;
- urgent conditions - cyst rupture/torsion, ectopic pregnancy;
- endometriosis, spread of pathological foci;
- fibroids;
- large endometrial polyps, etc.
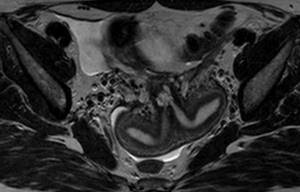
Bicornuate uterus on magnetic resonance scan
In case of infertility, MRI of the pelvis in women shows:
- anomalies and malformations of the internal genitalia:
- absence/underdevelopment of the uterus;
- organ duplication;
- atypical shape - one-, two-horned, saddle-shaped uterus;
- presence of septa (Asherman's syndrome);
- adhesions, etc.
MRI of the pelvic organs for infertility is considered as part of a comprehensive diagnosis; scanning does not replace endoscopic methods of examination.
Tumor node in the right lobe of the prostate on an MR photo (arrow)
In men, magnetic resonance imaging of the pelvis shows:
- neoplasms - cancer, prostate adenoma (the final diagnosis is formulated after a histological conclusion), the degree of obstruction of the urethra;
- inflammatory processes - prostatitis, vesiculitis, epididymitis, cystitis, proctitis;
- cysts;
- atypical location of the testicle in the inguinal canal with cryptorchidism, tumor of the gonad;
- prostate, cystolithiasis (stone formation);
- hernias;
- diverticula, bladder tumors, etc.
Preparation
MRI of the uterine cavity and adjacent organs cannot be performed during menstruation. The best days of the menstrual cycle are considered to be from 5 to 12. In certain cases, it becomes necessary to conduct an MRI of the uterus in the second half of the cycle. It is extremely important to have a menstrual cycle calendar when scheduling an examination.
When preparing for the procedure, the following recommendations must be followed:
- proper nutrition for 2-3 days to reduce the impact of gas-filled intestines;
- cleanse the intestines with laxatives or an enema on the morning of the procedure;
- the last meal before the examination no later than 4 hours before the start of the procedure;
- take painkillers in case of abdominal pain;
- moderately full bladder.
It is necessary to prepare yourself for a long stay in a motionless state, since the procedure takes quite a long time.
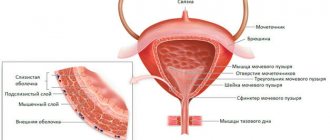
MRI of the pelvis: which organs are checked?
During the diagnostic procedure, women are scanned:
- uterus with cervix;
- vagina;
- the fallopian tubes;
- ovaries.
For men they look:
- prostate;
- seminal vesicles;
- inguinal canals;
- vas deferens.
MRI of the pelvis in individuals of both sexes includes assessment of:
- bladder, urethra, ureteric orifices;
- terminal parts of the intestine;
- lymphoid tissue;
- neurovascular bundles;
- fatty tissue.
Magnetic resonance imaging of the uterus and ovaries
Today MRI of the uterus and ovaries
is considered the most informative and safe method of studying a woman’s reproductive system. This type of diagnostics allows you to obtain data on the condition of certain organs and tissues without introducing any medical instruments or devices into the patient’s body. In addition to the uterus and ovaries, MRI images can be used to see and evaluate the condition of the fallopian tubes, as well as determine how correctly the female organ system as a whole functions.
Indications for MRI of the pelvic organs

The doctor chooses the examination method taking into account the clinical picture, goals and limitations for diagnostics.
Symptoms indicating a pathological process in this area are similar in a number of diseases. Magnetic resonance imaging is a fundamental part of diagnosis in most cases.
Indications for pelvic MRI in women include:
- pathological discharge (bloody, mixed with pus) not associated with menstruation;
- unexplained pain in the lower abdomen, dyspareunia (discomfort during sexual intercourse);
- delayed sexual development (absence of menarche - first menstruation in a girl over 14 years of age);
- dysuric disorders - pain when urinating, frequent urge, flow, appearance of blood in urine;
- dysfunction of the pelvic organs;
- irregular menstrual cycle;
- increased levels of tumor markers, suspicious for a tumor process, etc.
Indications for MRI of the pelvic organs in men are:
- persistent urination disorders, acute retention, detection of large amounts of residual urine by ultrasound;
- repeated increase in the level of tumor marker - prostate-specific antigen (PSA);
- detection of blood in urine, semen (including in the absence of complaints), suspicious ultrasonography data;
- sexual dysfunction;
- pathological changes in spermogram, etc.
How is a pelvic MRI done?

During the examination, you must lie still and follow the instructions of the x-ray technician.
The diagnostic procedure is performed mainly on closed-type tomographs, since the information content of images using units with a powerful field is higher. The stages are standard:
- pre-registration for the study;
- registration of a medical record, questionnaires to identify contraindications to MRI;
- storage of products containing metal;
- placing the patient on the tomograph table, fixing the limbs with soft belts and bolsters to prevent accidental movements, placing a field-enhancing coil over the pelvic organs;
- catheterization of the ulnar vein, connection of an injector with gadolinium during a planned study with contrast (manipulation is carried out according to indications);
- native scanning of the area of interest;
- supply of the enhancer drug to the required diagnostic phases;
- waiting for the paramagnetic to spread through the vessels;
- continue scanning;
- removing the catheter from the vein, applying a pressure bandage to the injection site.
The patient is alone in the diagnostic room, communication is carried out via speakerphone. The medical staff monitors the patient’s condition through a window from an adjacent room. Technical sounds from the device can be reduced using headphones. The patient has a panic button at hand for unforeseen situations. There is no pain. Reactions to the administration of contrast (dizziness, nausea, palpitations, etc.) are short-term, are not a reason to stop the examination and go away on their own after a few minutes.
There are contraindications for MRI:
- first trimester pregnancy;
- mechanical/electrical implanted devices, metal in the body;
- diseases with uncontrolled motor activity;
- obesity (weight above 120 kg);
- claustrophobia (MRI can be done in a hospital setting using sedatives);
- severe renal failure, including hemodialysis and a history of gadolinium allergy (for contrast);
- acute conditions - heart attack, stroke, etc.;
- unrelieved severe pain syndrome.
Procedure
The procedure begins with the preparatory stage. The doctor should ask the patient if he has any allergic reactions if contrast is to be administered. The patient is also obliged to inform the doctor about the presence of implants and devices with metal elements. The woman must inform the doctor about the presence of pregnancy, and also say that she is in the lactation period. The doctor receives answers to these questions during a standard questionnaire, which is conducted in writing. Most clinics ask the patient to change into disposable clothing, as well as remove body jewelry, accessories and other metal items.
Next, the subject is positioned on the retractable platform of the tomograph, his limbs are fixed with special belts, and his head is secured with bolsters. This is done to ensure complete stillness; even the slightest movement can degrade the information content of the resulting images. The patient needs to be prepared for the fact that the device may make characteristic sounds during the examination - hum, noise and clicks. However, it is possible to wear special headphones or use earplugs. A characteristic feature of the tomograph is the sensation of warmth in the area being examined. A catheter for administering contrast is installed immediately before the start, the active substance is supplied automatically at the moment when the patient is in the capsule. As it moves through the bloodstream, a feeling of cold or extreme heat may occur.
What is an MRI of the pelvis?
The diagnostic procedure takes 40-60 minutes, so it is better to choose loose clothing made from natural fabrics. It is important that there are no metal parts: zippers, rivets, decorations. The above can cause blurring on the films; if the part is accidentally torn off under the influence of a magnetic field, the part can injure the patient and lead to equipment failure. For the same reason, it is necessary to check the pockets before examination. You can take a change of clothes with you from home or purchase disposable medical underwear.
Interpretation of pelvic MRI results
The interpretation of images is carried out by a radiation diagnostics doctor (radiologist); in complex cases, a collegial assessment is possible
Independent interpretation of MRI images of the pelvis is an impossible task for a patient: special knowledge and skills are required. Standard criteria:
- correct anatomical position and size of organs;
- clarity/continuity of boundaries;
- absence of focal formations, adhesions, stones, free fluid, fistula tracts, congenital anomalies, foreign bodies, enlarged lymph nodes;
- completeness of blood flow;
- preservation of the muscular-ligamentous apparatus, nervous structures, etc.
When interpreting images, the radiologist takes into account the patient's age. If a deviation from the norm is detected, in the conclusion the doctor indicates the localization and size of the pathological focus, the presumed genesis, and the features of interaction with surrounding structures. The final diagnosis is formulated by the attending physician after assessing all available data: clinical picture, test results, biopsy, etc.