Basic rules for preparing for the blood drawing procedure
The following conditions must be met:
- before collecting biomaterial, you can eat food no later than 8-12 hours before the procedure, depending on the type of study;
- 2 days in advance you need to remove fried and fatty foods from your diet;
- 1 day before the test, avoid physical activity and do not go to the gym;
- in consultation with your doctor, you must stop taking medications that affect coagulation, except in cases where the analysis is carried out to monitor these indicators;
- 1 day before the procedure, a person should not undergo ultrasound, radiography, or endoscopy.
Analysis for protein fractions
Albumin is one of the fractions of total protein. A biochemical blood test for this indicator is prescribed if kidney and liver pathology is suspected. The reasons for the increase and decrease in concentration are the same as for the main substance. Albumin levels may also be reduced in pregnant or breastfeeding women or young children.
To determine the level of other specific proteins, you need to take blood tests to compile a proteinogram. The biochemical test allows you to evaluate the concentration of alpha, beta and gamma globulin fractions, as well as their qualitative composition. The level of these substances in the blood increases significantly during inflammatory processes or exacerbations of chronic diseases. Malignant tumors also cause an increase in their plasma volume.
A biochemical blood test for total protein and its fractions is taken strictly on an empty stomach. The day before the test, it is necessary to exclude fatty and heavy foods from the diet. Compliance with these requirements guarantees the accuracy and information content of the test.
FAQ
Is it necessary to donate blood from a vein on an empty stomach?
Food consumption should be no later than 8-12 hours before sampling. This is the time of assimilation, after which processes in the body are normalized.
Food intake affects the following indicators:
- glucose content
- enzyme activation;
- increasing the concentration of proteins and fats;
- change in viscosity;
- increase in hormonal saturation.
Food can cause false positive results, which is why you need to donate blood from a vein on an empty stomach. If this is not possible, collection is allowed at other times of the day, maintaining an interval of 6-8 hours from meals.
Can I drink water before donating blood?
There are no contraindications to drinking regular drinking water. Its composition has no effect unless sweeteners and dyes are used.
Is it possible to brush your teeth before donating blood?
If a biochemical analysis is prescribed, it is better to refrain from morning oral hygiene. It is not recommended to brush your teeth when testing for sugar, glucose, or urea. The paste contains triclosan, which affects the accuracy of the results obtained. Saccharin increases glucose levels. Foaming pastes can change the protein composition.
When taking hormone tests, there are no restrictions on brushing your teeth.
What time do you donate blood from a vein?
Usually the procedure is carried out from 8:00 to 10:00. This is the optimal time - 2 hours should pass after waking up. Before taking the test, a person should not experience physical exertion or become emotionally excited, so the morning is the best time. If you climbed the stairs, it is advisable to rest for 15 minutes. After the test, you can take the prescribed medications and have breakfast.
When should you not donate blood from a vein?
There are factors that distort the results. The procedure must be rescheduled if you:
- experienced increased physical activity and stress the day before or on the day of the test;
- took blood thinning medications unless specifically directed by a doctor;
- ate food less than 8 hours before the procedure.
How often can you donate blood from a vein?
This question worries people who need constant monitoring of indicators. Pregnant women and patients undergoing hospital treatment sometimes have to be tested every day. Don’t worry, the volume taken from a vein at a time is too small to have a negative effect on the body. Most patients do not notice blood loss.
Sugar analysis
The laboratory of the CDC "Health Laboratory" offers
a blood test for sugar The main tests are collected in a special profile. You can choose individual tests or undergo a comprehensive study. Doctors recommend taking a blood and urine test for sugar in the following cases:
- diagnosis and control of diabetes mellitus types I and II,
- pathologies of the thyroid gland, pituitary gland, adrenal glands,
- liver diseases,
- determination of tolerance to glucose (a component of sugar) when testing patients at risk,
- obesity,
- diabetes during pregnancy.
A blood test for glucose concentration is the main test for diagnosing diabetes mellitus. This is what you should take first when the following symptoms appear:
- excessive urination due to an increase in the osmotic pressure of urine caused by glucose dissolved in it (in a healthy person, the analysis shows the absence or minimal level of this substance),
- constant thirst associated with fluid loss,
- unexplained hunger and weight loss due to metabolic disorders.
These symptoms develop acutely and are most typical of type I diabetes. Secondary signs:
- itching,
- dry mouth,
- muscle weakness,
- skin inflammation,
- visual impairment.
A blood test for glycated hemoglobin is indicated for long-term follow-up of patients to monitor treatment and the degree of compensation. The level of this substance reflects hyperglycemia - an increase in sugar, typical of diabetics.
An endocrinologist will explain to you the expediency of the research. If your doctor has prescribed tests for sugar and other substances to assess carbohydrate metabolism, we invite you to undergo a comprehensive diagnosis with us. We use modern equipment to obtain accurate results.
Recommendations regarding fasting before a blood test
The following tips can help make fasting for a blood test easier:
- Stay hydrated . Drinking plenty of water before the test will make it easier to find blood vessels.
- Schedule your test in the morning . If you do your blood test in the morning, you will likely only need to skip one meal.
- Eat before fasting . Eating immediately before the fasting period reduces the time it takes to stop eating. For example, if your test is at 9 am and you need to fast for 12 hours, you can eat dinner around 8:30 pm the previous evening.
- Avoid exercise while fasting . Exercise speeds up digestion and forces you to burn extra calories.
- Do not be distructed . Keeping yourself busy will help relieve hunger.
Reference values
The result is given in the form:
- RHD+SEX;
- RHD+SEX with additional comment - “A weak Rh antigen has been detected. For blood transfusion, it is recommended to use Rh-negative red blood cells”;
- RHD-OTR.
Erythrocytes (red blood cells) carry various proteins (antigens) on their surface. These antigens are inherited from parents.
About 236 erythrocyte antigens have been identified (most of them are rare). They are grouped into blood group systems. One of these systems, which is of great practical importance, is the Rh factor system. Among the Rh antigens, the most important is the D antigen (RhD). It is antigen D that is meant by the term Rh factor. Based on the presence or absence of the D antigen, people are divided into Rh-positive and Rh-negative.
Antigen D (Rh factor) has pronounced immunogenic properties (the ability to cause the formation of antibodies).
Rh conflict (mismatch of Rh affiliation between recipient and donor, mother and fetus) is the cause of hemolytic disease of newborns in 95% of cases, as well as a common cause of severe complications that occur after blood transfusion (post-transfusion complications).
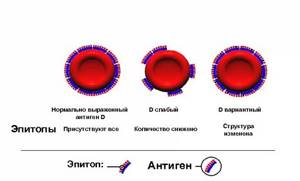
When determining Rh status, several variants of the D antigen are distinguished, which can lead to difficulties in determining it.
Most often, the red blood cells of a Rh-positive person carry all types of D antigen ( normally expressed D antigen
).
Some people have normal types of antigen on their red blood cells, but their amount on the cell surface is reduced - this variant is called D weak
.
If red blood cells do not carry all types of D antigen (they differ qualitatively), then this option is designated as D variant
.
A blood test for Rh status is an important stage in the preoperative preparation of the patient, when there is a possibility that a donor blood transfusion (blood transfusion) will be required. If a person (recipient) with Rh-negative blood is transfused with Rh-positive blood, the recipient’s immune system will recognize this antigen as foreign and trigger the production of antibodies to it (as a rule, a small amount of antibodies is formed, but so-called memory cells (B-lymphocytes) remain) who remember antigen D). Upon repeated contact with foreign erythrocyte antigens, a large number of antibodies are immediately formed, and donor erythrocytes begin to be massively destroyed. This leads to post-transfusion complications - hemolytic anemia (a decrease in hemoglobin capable of carrying oxygen to tissues and organs due to the destruction of red blood cells), acute renal failure, jaundice, post-transfusion shock.
The second possible situation for the occurrence of an Rh conflict is pregnancy, when a Rh-negative mother (there is no D antigen on her red blood cells) is pregnant with a Rh-positive child (the Rh factor is present on the fetal red blood cells). In the later stages of pregnancy, fragments of Rh-positive erythrocytes of the fetus can penetrate into the mother's blood, where they will be perceived as a foreign antigen and cause an immune system reaction - the production of antibodies to the Rh factor. These antibodies, in turn, are able to penetrate the placenta into the child’s body and destroy its red blood cells. During the first Rh-positive pregnancy, the mother’s body usually does not have time to form a sufficiently large number of antibodies, and the fetus does not experience serious complications. However, subsequent Rh-positive fetuses may experience chronic breakdown of red blood cells. Usually, if a miscarriage does not occur, such children are born premature and suffer from anemia (anemia) and jaundice. This condition is called hemolytic disease of the newborn (hemolysis - destruction of red blood cells). It can lead to the death of a child.
Thus, early examination of the mother and fetus for Rh status helps prevent Rh conflict and the death of the newborn.

Sources:
- Mineeva N.V. Human blood groups. Fundamentals of immunohematology. - St. Petersburg. 2004. 188 p.
- Dutkevich I.G. Practical guide to clinical immunohematology (group antigens and antibodies of human blood, blood groups and their clinical significance, methods of immunohematological research). — St. Petersburg: SpetsLit, 2018. 159 p.
- Connie M. Westhoff. The Structure and Function of the Rh antigen Complex. Semin Hematol. January 2007; 44(1): 42–50.
- Pegoraro V, Urbinati D, Visser GHA, Di Renzo GC, Zipursky A, Stotler BA, et al. (2020) Hemolytic disease of the fetus and newborn due to Rh(D) incompatibility: A preventable disease that still produces significant morbidity and mortality in children. PLoS ONE 15(7): e0235807.
Symptoms that may require a fasting blood test
There are many diseases and conditions that your doctor may want to test you for with a fasting blood test. Three common examples, among many, are diabetes, high cholesterol, or low iron.
The following symptoms may indicate one of these conditions:
- extreme thirst
- slow wound healing
- blurred vision
- fatigue
- frequent urination
- pale skin
- brittle nails
- headache
- dizziness