erythrocytosis hereditary familial
(Greek erythros red + kytos receptacle, here - cell + -osis; synonym:
benign familial polycythemia, primary erythrocytosis of children, cryptogenic erythrocytosis, polycythemia vera of childhood
) - a genetically determined group of diseases characterized by an increase in the content of hemoglobin and red blood cells in the blood, changes in blood viscosity and microcirculation disorders.
The first reports of hereditary familial erythrocytosis appeared at the beginning of the 20th century, when the mechanisms regulating the formation of red blood cells, as well as the relationship between the structure and function of hemoglobin, were not yet known. The first abnormal hemoglobin (Hb Chesapeake), causing hereditary familial erythrocytosis, was discovered by S. Charache in 1966. In our country, L.A. Polyakova, Yu.N. Tokarev and others (1974-1979) described the so-called Chuvash type of hereditary familial erythrocytosis, which is found, as a rule, in the Chuvash Autonomous Soviet Socialist Republic (about 140 patients were identified).
Etiology and pathogenesis
The etiological factors of hereditary familial erythrocytosis are gene mutations that lead to the formation of abnormal hemoglobins with increased affinity for oxygen (about 30 such hemoglobins are known), to a deficiency of the enzyme diphosphoglycerate mutase (bisphosphoglyceromutase; EC 2.7.5.4) or an increase in the concentration of ATP in erythrocytes. Hereditary familial erythrocytosis may be due to increased formation of erythropoietin (see) in the kidneys (autosomal recessive type of inheritance). In some cases, hereditary familial erythrocytosis can imitate polycythemia (see). The Chuvash type of erythrocytosis is hereditary-familial with an unclear genesis (autosomal recessive type of inheritance).
Abnormal hemoglobins with increased oxygen affinity are inherited in an autosomal dominant manner. If there is a defect in the protein part of the hemoglobin molecule, the connection of hemoglobin with oxygen becomes more stable and the release of oxygen to tissues becomes more difficult. In this case, tissue hypoxia develops, the physiological reaction to which is an increase in the number of red blood cells. The increased affinity for oxygen is due to the replacement of one of the amino acid residues of the hemoglobin protein molecule. There are several groups of amino acid substitutions that lead to an increased affinity of hemoglobin for oxygen. The affinity of hemoglobin for oxygen is significantly increased by the reduced content of 2,3-diphosphoglycerate in erythrocytes due to deficiency of the enzyme diphosphoglycerate mutase (autosomal recessive type of inheritance) and increased concentration of ATP in erythrocytes (autosomal dominant type of inheritance). In this case, as a result of poor oxygen delivery to tissues, generalized tissue hypoxia occurs, including kidney hypoxia, leading to erythrocytosis due to increased formation of erythropoietin.
What are the normal levels of red blood cells in a child’s blood?
The state of health can be judged by the decreased or increased level of these cells. That's why it's so important to know what this means.
To determine the exact indicators, you need to take tests in the morning and on an empty stomach. The content of red blood cells may vary depending on climatic conditions, age and gender. Dramatic changes occur from infancy to adolescence. Here are the standard indicators:
- in newborn babies – 4.3-7.6*10¹²/l;
- in one-month-old children – 3.8-5.6*10¹²/l;
- in one-year-old children – 3.6-4.9*10¹²/l;
- up to 13 years – 3.5-4.7*10¹²/l;
- in adolescence – 3.6-5.1*10¹²/l.
A significant number of red blood cells after birth is explained by the fetus's adaptation to intrauterine life.
From the first day, cells are destroyed and replaced with new ones. At the same time, jaundice appears in babies. During pregnancy, iron is greatly consumed and the number of red blood cells decreases.
Clinical picture
The severity of clinical symptoms varies and depends on the type of inheritance. With an autosomal dominant type of inheritance, the disease is usually asymptomatic. Clinical manifestations are most pronounced with the autosomal recessive type of inheritance, to which the Chuvash type belongs. This hereditary familial erythrocytosis is detected mainly in childhood and adolescence. The main symptoms are caused by plethora (see), increased blood viscosity, microcirculation disorders (see). The most common complaints are headache, fatigue, pain in the lower extremities and in the heart area. All patients have red cyanosis; a number of patients have moderate hepatomegaly, splenomegaly, and symptoms of “drumsticks” and “watch glasses.” The most common complications are cerebral thrombosis and capillary bleeding.
There is a significant increase in hemoglobin content and the number of red blood cells in the blood. The hematocrit number (see) in some patients can reach 90% (the so-called hard blood syndrome). Blood viscosity usually exceeds 8.0. ROE is sharply slowed down and is often not recorded.
Trepanobiopsy of the ilium reveals hyperplasia of the erythroid lineage of hematopoiesis, elements of bone tissue restructuring with increased bone resorption and osteoblastic reaction, as well as focal growths of fibrous substances against the background of massive microcirculation disorders.
Erythremia (polycythemia vera, erythrocytosis, Vaquez disease)
In the early stages of the disease, there are usually no symptoms. However, as changes in the blood supply system increase, patients complain of a vague feeling of fullness in the head, headaches, and dizziness. Other symptoms appear depending on which body systems are affected. Paradoxically, hemorrhage can be a complication of erythremia.
The advanced stage is characterized by more pronounced clinical symptoms. The most common and characteristic symptom is headaches, sometimes in the nature of painful migraines with blurred vision.
Many patients complain of pain in the heart, sometimes like angina pectoris, pain in the bones, in the epigastric region, weight loss, blurred vision and hearing, unstable mood, and tearfulness. A common symptom of erythremia is skin itching. There may be paroxysmal pain in the tips of the fingers and toes. The pain is accompanied by redness of the skin.
Upon examination, attention is drawn to the special red-cyanotic color of the skin with a predominance of dark cherry tone. Redness of the mucous membranes (conjunctiva, tongue, soft palate) is also noted. Due to frequent thrombosis of the extremities, darkening of the skin of the legs and sometimes trophic ulcers are observed. Many patients complain of bleeding gums, bleeding after tooth extraction, and bruises on the skin. In 80% of patients, there is an enlargement of the spleen: in the advanced stage it is moderately enlarged, in the terminal stage severe splenomegaly is often observed. Usually the liver is enlarged. Often in patients with erythremia, increased blood pressure is detected. As a result of malnutrition of the mucous membrane and vascular thrombosis, ulcers of the duodenum and stomach can occur. Vascular thrombosis plays an important role in the clinical picture of the disease. Thrombosis of the cerebral and coronary arteries, as well as the vessels of the lower extremities, is usually observed. Along with thrombosis, patients with erythremia are prone to the development of hemorrhages.
In the terminal stage, the clinical picture is determined by the outcome of the disease - liver cirrhosis, coronary thrombosis, a softening focus in the brain due to thrombosis of cerebral vessels and hemorrhages, myelofibrosis accompanied by anemia, chronic myeloid leukemia and acute leukemia.
The prognosis depends on the patient's age at diagnosis, treatment, and complications. Mortality is high in the absence of treatment and in cases where erythremia is combined with leukemia and other cancers.
Diagnosis
The diagnosis is established on the basis of anamnesis, clinical picture, hemogram results (see), histological examination of the bone marrow. To identify abnormal hemoglobin with increased affinity for oxygen and deficiency of 2,3-diphosphoglycerate, the oxygen dissociation curve and blood P50 are determined (see Hemoglobin). Abnormal hemoglobin can be detected using electrophoresis (see). Differential diagnosis is carried out with polycythemia, usually observed at the age of 55-60 years, which is characterized by severe splenomegaly, leukocytosis, thrombocytosis and three-line hyperplasia of the bone marrow (see Polycythemia), and with secondary erythrocytosis (see), the clinical picture of which is determined by the underlying disease .
What are red cells for?
First, let's learn how red blood cells are made. They are formed under the influence of the kidney hormone, and the material for their construction is hemoglobin.
It is a structural protein that binds oxygen and carbon dioxide. Red blood cells travel throughout the circulatory system and enrich its structure.
These cells live for 120 days and then they are destroyed in the spleen or liver. An analysis with elevated values does not always mean some kind of disease. Changes may occur due to dehydration, poisoning, or drinking poor quality water. Here are the main functions of these cells:
- The functioning of the body's defenses.
- Stable level of acid-base balance.
- Filling tissues with oxygen.
- Transport of amino acids from the digestive organs to tissues.
- Movement of carbon dioxide to the lungs.
Treatment
Treatment is symptomatic, aimed at removing excess red blood cells and reducing blood viscosity. For this purpose, bloodletting is recommended, which is advisable to combine with the prescription of anticoagulant agents (acetylsalicylic and nicotinic acids, chimes), as well as plasmapheresis (see).
Forecast
for life with an autosomal dominant type of inheritance, in most cases it is favorable; with an autosomal recessive type of inheritance, the prognosis is less favorable, since vascular complications are possible.
Prevention
not developed.
Bibliography:
Gudim V.I., Moskaleva G.P. and Ivanova V.S. Level of erythropoietin in patients with endemic familial erythrocytosis, Probl. hematol. and overflow, blood, vol. 23, no. 7, p. 15, 1978; Dmitrieva M. G. et al. Oxygen transport and acid-base balance in patients with endemic hereditary erythrocytosis, ibid., vol. 24, no. 11, p. 8, 1979; Efimova N.K. and Polyakova L.A. System of hemostasis and hemocoagulation in patients with endemic familial erythrocytosis, ibid., t. 23, no. 7, p. 11, 1978; Hereditary anemias and hemoglobinopathies, ed. Yu. N. Tokareva et al., p. 312, M., 1983; Polyakova L. A. Familial erythrocytosis in residents of the Chuvash Autonomous Soviet Socialist Republic, Probl. hematol. and overflow, blood, vol. 19, no. 10, p. 30, 1974; Tokarev Yu. N. et al. Hereditary erythrocytosis, ibid., vol. 24, No. I, p. 3, 1979; Adamson JW Familiae polycythemia, Semin. Hematol., v. 12, p. 383, 1975; Charache S., Weathe-g a 1 1 DJ a. With 1 egg JB Polycythemia associated with hemoglobinopathy, J. clin. Invest., v. 45, p. 813, 1966.
Yu. N. Tokarev.
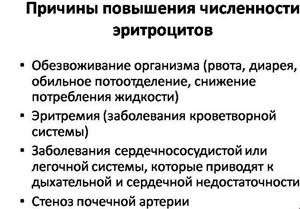
Symptoms of high red blood cell count

Now let's figure out how to determine erythrocytosis by symptoms. With a viral or intestinal infection, the symptoms will be identical to those of the underlying disease. Here are the symptoms to pay close attention to:
- The skin becomes red. The color may be pinkish and then acquire darker shades. Changes also affect the mucous membranes.
- Pain appears in the toes. This occurs due to deterioration of blood flow.
- With oxygen starvation, paroxysmal pain appears.
- Frequent headaches occur as blood circulation in small vessels deteriorates.
- The spleen enlarges due to an excess of red blood cells.
- Renal pathology causes an increase in blood pressure.
A general blood test will help determine the exact level of red blood cells. With such symptoms, children become lethargic, exhausted and play little. The analysis also allows you to determine the shape, size of red blood cells, as well as their saturation with hemoglobin.
Diagnostic methods
The most frequently held events are:
- Ultrasound diagnostics of the kidneys, blood vessels and heart.
- Analysis to determine platelet and leukocyte counts.
- Intravenous pyelography.
- Measurement of hemoglobin, hematocrit and erythropoietin levels.
- General blood test and blood gas composition.
Modern medicine uses erythrocyte indices to diagnose diseases with changes in red blood cells.
This could be the average volume of red blood cells or their hemoglobin content. If the width of the cell distribution is exceeded, the problem may be hidden in bleeding, liver disease or folate deficiency anemia.
Reasons for reducing an important indicator
You also need to know why your red blood cell count may be decreasing. The reasons may be:
- anemia and blood loss;
- liver diseases;
- insufficient formation of red blood cells occurs with a deficiency of folic acid or iron;
- genetic diseases;
- infectious diseases such as diphtheria, whooping cough or parasites;
- oversupply of medications, such as antibiotics.
Diseases at high rates

The relative form of the disease also manifests itself in severe burns. In this case, the blood thickens, and the amount of proteins and plasma decreases.
In newborns, high red blood cell counts are associated with hypoxia that occurred in the womb. True erythrocytosis is provoked by the following diseases:
- With erythremia, all cells in the bone marrow are overproduced, but especially red blood cells. The disease occurs as a result of radiation, toxic lesions or gene mutation.
- Chronic respiratory diseases.
- Congenital heart defects that cause circulatory failure.
If you do not pay attention to the excess of such cells in the body in time, there can be serious consequences.
Over time, disruption occurs in all tissues of the body, systems and organs. The blood becomes thicker, which can affect breathing and blood supply to cells.
And disturbances in blood supply can cause problems with the cerebral cortex. of the kidneys, liver and spleen increases .