The liver is the largest organ of the abdominal cavity and performs vital functions. For many reasons - poor quality nutrition, poor environment, late diagnosis of gastrointestinal diseases, etc., the number of advanced liver diseases increases every year. At the same time, almost any problem can be detected very quickly by performing an ultrasound of the liver.
Click to make an appointment, ultrasound or tests
Ultrasound of the liver - ALL ABOUT THE EXAMINATION, INCLUDING DECODING
An ultrasound examination provides the most detailed information about the condition of the liver, its functioning and changes.
Indications for ultrasound diagnostics of the liver
The content of the article
Diagnosing liver diseases on your own is a problematic process - most of the diseases of this organ are hidden in nature - clear symptoms appear only when the process of liver destruction is clearly observed, and it is already too late to change anything. Knowing this, many people regularly undergo preventive ultrasound examinations, thus maintaining their health, youth and good mood. An ultrasound of the liver is included in an ultrasound examination of the abdominal cavity, but can also be performed separately.
In addition to preventive examination, there are a number of direct indications for liver ultrasound. You need to undergo an ultrasound examination if you have:
- Abdominal injuries;
- Unsatisfactory blood tests, the results of which may suggest liver damage;
- Painful sensations and heaviness in the area of the right hypochondrium;
- Yellowish color of the skin;
- Change in sclera color;
- Hepatitis A, B and C;
- Markedly enlarged liver size;
- Suspicion of an abscess and parasitic type infestation;
- Neoplasms of various types identified based on test results;
- Gynecological problems;
- Use of hormonal contraceptives.
Moreover, ultrasound can detect cancer metastases, viral pathologies of the liver, cysts and cystic formations, and hemangiomas.
Methodology
The study is carried out both in the morning and in the afternoon. The interval between the last meal and the start of the liver ultrasound should be at least 6-8 hours. You can take napkins or a small towel with you to remove any remaining gel from the skin of the abdomen. The doctor must provide all available medical documentation (referrals, statements, test results). Before starting an ultrasound scan of the liver, the patient is placed on his back and asked to expose his stomach. Then a water-soluble gel is applied to the area of the right hypochondrium and the organ is examined by moving a special sensor over the skin of the abdomen.
If necessary, liver ultrasound is supplemented with ultrasound examination of the gallbladder, pancreas or spleen, and Doppler ultrasound of the liver vessels. The procedure is absolutely painless and does not cause any discomfort. The duration of the study is about 10 minutes. After completing the liver ultrasound, the remaining gel is wiped off the abdomen. The patient is informed when he can come for a conclusion. Depending on the specialist’s workload, preparing documents can take from 30 minutes to 1 day.
What diseases does an ultrasound scan of the liver show?
Ultrasound diagnostics detects even the slightest deviations from normal values, not to mention diseases and pathologies that threaten the life and health of the patient. The doctor, having studied the results of the ultrasound, makes a conclusion about the presence of liver pathologies such as:
- Hepatitis in acute and chronic form;
- Calcifications that occur against the background of infectious diseases (malaria, tuberculosis, amoebiasis);
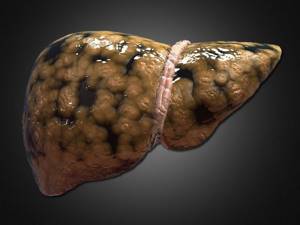
- Cirrhosis of the liver;
- Cancer metastases;
- Hepatomas;
- Hemangiomas;
- Budd-Chiari syndrome.
During an ultrasound scan of the liver, a clear picture appears on the monitor, in which the contours of the liver are clearly visible. Therefore, ultrasound diagnostics helps to accurately identify a particular disease in a timely manner and avoid possible complications.
An ultrasound of the liver is usually performed as an additional examination if problems are detected with nearby internal organs.
Indications
The method can be used both at the stage of screening studies and at the stage of final diagnosis. The purpose of liver ultrasound is to assess the condition of the liver and organ blood flow, identify diffuse and focal pathological changes, determine the severity of the disease and the extent of the pathological process, conduct differential diagnosis, and select conservative treatment tactics or surgical intervention. In addition, liver ultrasound is used to assess the effectiveness of treatment during and after therapy, as well as to monitor the course of the disease in remission.
Ultrasound of the liver is prescribed for pain in the right hypochondrium, traumatic injuries to the abdominal area, yellowness of the skin and mucous membranes, the appearance of laboratory signs of liver dysfunction, drug and alcohol abuse, and long-term use of medications that have a negative effect on the condition of the organ. Ultrasound of the liver is also performed if there is a suspicion of a liver abscess, a primary oncological process in the tissue of the liver parenchyma, or metastatic damage to the organ in tumors of other localizations.
To monitor the course of the disease, timely detect complications and relapses, liver ultrasound is regularly performed for already diagnosed diffuse lesions of the organ, previously suffered hepatitis and cancer in remission. Liver ultrasound is a highly sensitive diagnostic procedure that allows you to detect cirrhosis, chronic hepatitis, fatty hepatosis, liver abscesses, traumatic hematomas, metastases, primary liver cancer, Budd-Chiari syndrome, calcifications and some other pathological processes. There are no contraindications to the study.
Are there any contraindications to liver ultrasound?
Ultrasound is a safe and painless procedure. It is recommended for adults and children. Ultrasound examination of the liver can be contraindicated only in one case - the patient has wounds and other damage to the skin in the abdominal area, as well as dermatological diseases.
In such cases, the gel should not be applied to the skin. In all other cases, ultrasound is recommended for use, especially in acute pain syndromes. In this case, the liver is clearly visualized during diagnosis. The maximum information content of ultrasound is achieved with repeated repetitions. Often it is carried out several times every 2-3 weeks.
Contraindications

Ultrasound is a safe and accessible diagnostic method for various diseases. It does not require complex manipulations or special preparation. An ultrasound examination cannot negatively affect the patient’s health and well-being, and there will be no pain or discomfort during the procedure. Based on this, we can conclude that this method has no contraindications. Ultrasound is performed for both adults and children who have just been born, pregnant women, and seriously ill patients.
How to properly prepare for a liver ultrasound
The most accurate diagnosis is to obtain a suitable abdominal condition. Therefore, preparation for an ultrasound is of great importance. To get correct results, you need to follow a number of simple recommendations:
- Approximately three days before the procedure, it is important to stop eating fruits, brown bread, milk, carbonated drinks - those foods that contribute to gas formation in the intestines;
- A few hours before the test, it is necessary to take medications that reduce flatulence (espumisan, activated carbon, enzyme preparations);
- If the patient suffers from constipation, then before the ultrasound you need to cleanse the intestines with an enema.
Structure of the liver
Anatomically, this organ is divided into two areas:
- Left lobe.
- The right lobe, which consists of the quadrate lobe and the caudate lobe.
Segmentally, the organ can be divided into 8 parts. Each part appears as a pyramidal-shaped area of hepatic parenchyma. The segments are supplied with blood and innervated separately. Each section of the segment contains nerve endings that ensure interaction between the liver and the central nervous system.

The structure of the liver and its location in the body.
Lobular parenchyma includes:
- hepatic plates, which consist of radial rows of hepatocytes;
- intralobular blood capillaries,
- capillaries of the biliary tract.
In the stromal part of the liver there are:
- outer connective tissue capsule,
- loose fibrous tissue of interlobular layers,
- blood vessels
- and nerve endings.
Interpretation of liver ultrasound results
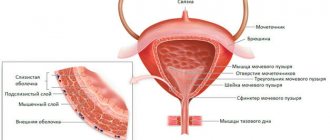
In normal condition, the liver is located on the right side of the body, in the hypochondrium. Due to its rather large size, the liver is not completely visualized. To fully examine the organs, the doctor performs several manipulations that evaluate the shape, contours and structure of the liver.
On the monitor you can clearly distinguish the lobes of the liver: left, right, quadrate and caudate. These shares include 8 segments. Their study helps to correctly determine the localization of the pathology.
If the patient has properly prepared for the examination, several small-diameter pits can be seen in the lower part of the liver. They were formed as a result of the close location of the organ to the stomach, right adrenal gland, colon and right kidney.
Ultrasound should not show the ligamentous apparatus, only the coronary sulcus. The hepatic veins, bile ducts and branches of the portal vein should normally be clearly visible.
In the process of examining the liver with ultrasound, the doctor similarly examines each part of the organ through transverse and oblique sections, measures them and records all dimensions in the examination protocol.
Fatty liver on ultrasound
Fatty hepatosis is extremely rare in completely healthy people. It develops as a consequence of existing diseases, such as diabetes mellitus, pancreatitis, gastric ulcer, alcoholism, etc. Hepatosis is characterized by extremely rapid development of the disease. Thus, after toxic damage to the liver as a result of poisoning (mushrooms, chemicals), fatty infiltration occurs within a week. Fatty liver disease can be easily detected using ultrasound. Depending on the location of fat deposits, the disease is of three types:
- Diffuse hepatosis . Fat cells are evenly distributed throughout the organ. This type also develops in completely healthy people who violate their diet. For example, in vegetarians, a lack of protein due to the refusal of animal foods disrupts the production of lipids, which also occurs after a long-term strict diet, after eating fatty and carbohydrate foods. Metabolic disorders also occur after a course of antibiotics.
Unlike a healthy organ, with diffuse hepatosis, the freedom to conduct ultrasound is reduced, which is displayed as white spots on the screen. The deep parts of the liver are poorly visualized, and the small venous pattern is not visible. The contours of the liver remain clear, but the size of the organ increases slightly.
- Local hepatosis . Fatty formations are found only in certain areas of the liver. On ultrasound, this is reflected by hypoechoic areas against the background of healthy parenchyma. focal hepatosis. Foci affected by fatty deposits are visualized as voluminous hyperechoic areas.
Common signs of hepatosis are a “light” liver - a predominance of low-echoic tissue areas that do not conduct ultrasound well. Areas affected by fat cells prevent the organ from functioning normally, which leads to serious consequences: stagnation of bile, intoxication of the body, decreased immunity. bile does not arrive in full, food is digested worse, enters the intestines not completely digested, provoking dysbacteriosis and intestinal infections.
The liver is less able to cleanse the body of toxins, reducing the supply of nutrients and vitamins. With fatty hepatosis, the cardiovascular system suffers, hypertension, myopia, and cardiac dysfunction develop. General intoxication reduces immunity, creating favorable conditions for ARVI, influenza and other infections.
Normal liver parameters detected by ultrasound in adults
| Index | Numerical value of the norm in adults |
| Cross section | 20-22.5 cm |
| Length | 15-18 cm |
| Left lobe height | up to 1 cm |
| Left lobe thickness | about 7 cm |
| Sagittal size | 10-12 cm |
| Right lobe length | 11-15 cm |
| Right lobe thickness | 11-12.5 cm |
| Oblique vertical size of the right lobe | about 15 cm |
In the process of measuring the liver, the bile ducts and blood vessels are examined. In this case, the following are considered normal indicators:
- Vena cava diameter: about 1.5 cm;
- Bile duct size: 0.6-0.8 cm;
- Portal vein diameter: 1.3 cm;
- Diameter of the hepatic artery at the porta hepatis: 4-7 mm;
- The diameter of the hepatic veins at a distance of 2 cm from the mouths: 0.6-1 cm.
The doctor compares the results obtained during the ultrasound with normal values, and also evaluates the liver tissue, its contours and structure. Based on the totality of all the data obtained, a conclusion is made about the condition of the organ and the presence of indications for drug treatment, if any.
Hepatitis and liver on ultrasound
Hepatitis is a viral infection that leads to inflammation of the organ. In the acute form of inflammation, there is an accumulation of fluid in the tissues, and it conducts ultrasound well, so inflammatory processes are characterized by hyperechogenicity.
The size of the liver also increases. Its surface becomes too smooth and even, but the contours are blurred.
For hepatitis C, Doppler scanning is used to identify areas with increased blood flow and places where it is impaired or absent. With hepatitis B and C, you can see the affected areas of the parenchyma replaced by hyperechoic connective tissue.
Indicators of normal liver parameters in children
In normal condition, the size of the liver corresponds to the height of the child. Accordingly, the older the child, the larger the liver volume.
| Age | Left lobe length | Right lobe length | Portal vein diameter |
| 1-2 years | 3.3 cm | 6 cm | 2.9-5.7 mm |
| 3-4 years | 3.7 cm | 7.2 cm | 3.5-7 mm |
| 5-6 years | 4.1 cm | 8.4 cm | 4.3-7.6 mm |
| 7-8 years | 4.5 cm | 9.6 cm | 4.5-8.5 mm |
| 9-10 years | 4.7 cm | 10 cm | 4.9-9.5 mm |
| 11-12 years old | 4.9 cm | 10 cm | 5-10 mm |
| 13-14 years old | 5 cm | 10 cm | 5.6-10.2 mm |
| 15-16 years old | 5 cm | 10 cm | 5.7-106 mm |
| 17-18 years old | 5 cm | 12 cm | 7-12 mm |
As for the structure of the liver, in normal condition it has the following indicators:
- Clear, smooth contours;
- The vena cava is presented as an echo-negative formation;
- Homogeneous structure;
- Location of portal ducts: on the periphery;
- The echoes are small and of low intensity;
- The structure is fine-grained.
If the structure changes, the doctor records in the protocol a change in echogenicity up or down.
Liver structure
It is worth starting to study granularity only after understanding what the structure of the liver is and what it is like.
The structure of the liver is the structure of its connective tissue, which lines the organ and divides it into a large number of miniature lobules. This is how the liver skeleton, the stroma, is formed. Each of its lobes looks like a hexagonal prism. Between these prisms there is a network of capillary vessels and bile ducts, clearly visible against the background of connective tissue. They gradually turn into larger channels through which the inflow and outflow of synthesized compounds occurs: enzymes, bile and bile acids.
Hexagonal lobules consist of hepatocytes - liver cells that perform the main work. They seem to be laid out in plates one cell thick and form branches, the sinusoids between which are filled with blood.
Heterogeneity of any type is in any case a deviation
Signs of liver disease detected by ultrasound
A particular disease can be determined by its reaction to ultrasound. Each pathology has its own characteristics.
| Pathology | Signs |
| Chronic hepatitis | Reduced echogenicity, noticeable increase in liver size |
| Calcifications | Dense structure |
| Acute form of hepatitis | The structure of the liver is heterogeneous, there are areas with low echogenicity, the liver is enlarged, the tissues are edematous |
| Cirrhosis of the liver | Different sizes of lobes, vessels are clearly visible, the surface is uneven, regenerating nodes larger than 5 mm are visible |
| Tumor metastases | Increased echogenicity |
| Hepatoma | Uneven structure, increased echogenicity |
| Budd-Chiari syndrome | The lumens are narrowed, the hepatic veins are not visible, formation in the parenchyma |
| Hemangioma | Symptoms are not pronounced |
At the end of the liver examination, the doctor records all echo signs. This is not yet a definitive diagnosis. The interpretation of the ultrasound results is carried out by the attending physician, who, based on the studied data, tests and examination of the patient, makes a conclusion about the patient’s state of health.
What do changes in the liver indicate?
If the patient begins to feel pain in the right side, periodically vomits, the color of urine (darkened) and stool (lightened), then an ultrasound scan is required, since these symptoms indicate a malfunction of the liver.
Hepatomegaly with a homogeneous fine-grained structure
When the gland is larger than normal in size, and its structure is homogeneous and no foreign inclusions are found, this indicates diseases:
| Disease | Explanation |
| Heart failure | Additionally, ultrasound visualizes pathological dilatation of the hepatic veins, which are normally not visible. The diameter of the inferior vena cava does not change during the patient’s inhalations/exhalations (normally it should). |
| Acute form of hepatitis | As a rule, nothing is found other than hepatomegaly. The general picture is within the normal range for adults. |
| Tropical form of hepatomegaly | Simultaneously with the enlargement of the liver, an increase in the size of the spleen is observed. |
| Schistosomiasis | Against the background of hepatomegaly, thickening of the walls of the portal vein and its large branches is noticeable, while the surrounding tissues are bright. Sometimes the spleen increases in size, fibrosis of the liver tissue is determined. |
Hepatomegaly is not normal. Even if there are no other morphological signs on ultrasound, additional research is required.
Hepatomegaly with heterogeneous structure
An increase in liver size with heterogeneity of structure is detected in a number of diseases and pathological processes:
- Hepatomegaly, heterogeneity of structure, absence of focal neoplasms - all these are signs of cirrhotic processes, chronic hepatitis or fatty infiltration of the organ. Ultrasound shows an increase in echogenicity, a decrease in the number of visible branches of the portal vein. Sometimes there is a significantly reduced sound conductivity, which is why the deep-lying parts of the gland are not visualized at all.
- Hepatomegaly and structural heterogeneity, the presence of multiple or single focal formations of different sizes, shapes and structures, indicate a macronodular type of cirrhosis, abscesses, hematomas or lymphoma. In the macronodular type of cirrhosis, ultrasound shows a transformation of the vascular pattern, normal stroma and neoplasms of different sizes. And with an abscess, an increase in echogenicity, single or multiple inclusions that have unclear contours are recorded.
With lymphoma, in addition to hepatomegaly and heterogeneity, the diagnostician sees hypoechoic areas with unclear contours.
Shrinking liver and causes
A decrease in organ parameters is characteristic of large-nodular cirrhosis. At the same time, the study shows an increase in echogenicity, deformation of the gland due to the formation of scars. The portal vein, unchanged or collapsed inside the organ, has an increased size outside the gland. Sometimes structures that are blood clots can be visualized inside the vein.
Single formation in the gland

This could be a hemangioma, abscess, cyst with suppuration, metastases, hepatoma. Ultrasound cannot differentiate these formations, therefore, if a serious pathology is suspected, it is recommended to perform a biopsy - the collection of biological material for the purpose of further research and differentiation in the laboratory. According to statistics, a single formation in the liver in 75% of clinical pictures appears as a hemangioma.
Cystic neoplasms
The etiology of cysts is different. With a solitary cyst, the specialist sees a light, round-shaped neoplasm, the edges are clear or uneven, the diameter is up to 3 cm. Typically, cysts of this type are congenital, they are not given to clinics, and do not pose any danger. However, doctors recommend a biopsy, since ultrasound cannot differentiate a congenital cyst from a parasitic inclusion.
Multiple cysts in the gland are visualized as light-colored neoplasms of various diameters, the contour is clear, and acoustic enhancement is observed. With such a picture, examination of the spleen, kidneys and pancreas is required, since the probability of cyst formation in these organs is over 70%.
With a parasitic cyst, the ultrasound picture is different, since the morphological signs are determined by the stage of development of the parasite, the condition of the cyst walls, and cavities.
How much does a liver ultrasound cost?
An ultrasound examination of the liver will have different costs in different clinics. At the Diana Clinic in St. Petersburg, examinations can be performed at an optimal cost. Liver ultrasound price:
| Comprehensive ultrasound examination of the abdominal organs (liver, gall bladder, pancreas, spleen) | 1000 rub. |
| Ultrasound examination of the abdominal cavity + kidneys | 1600 rub. |
| Liver examination (separate examination) | 1000 rub. |
We recommend that you sign up for a comprehensive ultrasound of the abdominal cavity, because the cost of the examination will be exactly the same as the cost of examining one organ.
If you find an error, please select a piece of text and press Ctrl+Enter
How to decipher the results
Taking into account the physical basis of ultrasound examination, it is possible to decipher the results of ultrasound of the liver and gall bladder. How intensely ultrasound will be reflected depends on the organ’s density, structure, elasticity, and tissue resistance. In the presence of a pathological process in the organ being studied, the risk of changes in such indicators increases.

For example, if a person has a “porcelain” gallbladder, its walls will be saturated with calcium salts. Also, there will be an increase in tissue density.
When conducting an ultrasound examination of the liver, a lot of attention is paid to its size, shape, structure, and condition of the blood vessels. Normal liver size is 6-8 centimeters (left lobe), and 11-13 centimeters (right lobe). The edge of the organ is smooth, the structure should be uniform.
In addition, ultrasound examination determines the size of the gallbladder. It is considered normal if the gallbladder is from 6 to 10 cm long, 3 to 5 cm wide, the wall thickness is no more than 3 millimeters, the internal diameter of the lobar ducts is no more than three millimeters, and the common bile duct is from 6 to 8 millimeters.
Relevance of the diagnostic method
The relevance of liver ultrasound is that this study is the first and most important imaging method for suspected liver disease, this method is the first-line indication method in assessing liver function and cholestasis, for the differential diagnosis of jaundice (diagnosis/exclusion of cholestasis), for monitoring complications of cirrhosis (ascites, portal hypertension), to detect, exclude a tumor and to monitor it. Ultrasound enhancement with contrast agents is useful, especially for tumor detection and characterization.
Content:
- Relevance of the diagnostic method
- Application of ultrasound
- Ultrasound of the liver is normal
- Preparing the patient for the procedure
- What happens during the procedure
- Ultrasound in children
Sonography is necessary to guide liver or biliary interventions, such as biopsies. Sonography is the most important imaging modality for cancer.
What happens during the procedure
Once placed on the patient's table, the doctor will apply a warm water-based gel to the area of the body being examined. The instrument used during ultrasound is called a transducer, or transducer. The sensor is placed on the body, on top of the gel, and moves back and forth to capture images. The transducer emits high-frequency sound and records echoes that determine the size, shape and consistency of soft tissue and organs.
The transducer sends sound waves and receives echoes to develop ultrasound images inside the body, which are displayed in real time on a computer screen.
Ultrasound examinations are painless.
What can you expect after an ultrasound?
After a high-quality image is captured during the ultrasound, the doctor will help remove the gel from the surface of the skin. The patient can then put on clothes. The entire standard ultrasound procedure usually takes up to 30 minutes. Once the ultrasound is done, the patient can leave and return to their normal lives.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
The doctor will then analyze and interpret the images to check for any abnormalities.
Preparing the patient for the procedure

It is recommended that the patient fast before undergoing abdominal ultrasound, that is, ultrasound is preferably performed on an empty stomach for better visualization, to maximize distension of the gallbladder and to reduce food and gas debris in the upper digestive tract, which can reduce image quality or make it impossible to visualize the liver. This is necessary for complete visualization of the liver and associated bile ducts, but in an acute situation such as trauma where imaging of the gallbladder is not immediately necessary, it may not be necessary. The patient may drink a small amount of water before the scan, especially if taking any medications. There is some evidence that smoking may reduce image quality in upper abdominal scans, and it is advisable for the patient not to smoke for 6-8 hours prior to the ultrasound scan. Smoking increases the movement of gas into the upper gastrointestinal tract and may reduce image quality. In addition, certain chemicals in tobacco are known to cause contraction of GI smooth muscle and this may cause gallbladder contraction, even when tested on an empty stomach.
Ultrasound examinations of the liver in pediatrics
Introduction
Liver diseases often manifest as nonspecific complaints and in some cases are detected by chance. This applies, first of all, to children, in whom the proportion of congenital pathologies is higher than in adults. The reserve capacity of the liver is high, so the doctor’s task is to identify pathology before it becomes clinically significant.
Clinical anatomy of the liver
There is a well-known saying that compares ultrasound examinations (ultrasound) with a magic flashlight, which allows you to look into a dark room and examine its contents. Ultrasound provides us with the “living anatomy” of an organ, allowing us to make a topical diagnosis for focal liver damage or objectively characterize the dynamics of a diffuse process.
The right and left lobes of the liver are separated by a groove running from the bottom of the gallbladder to the inferior vena cava.
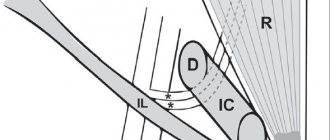
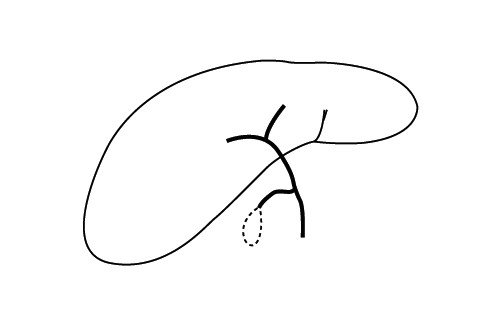
Each lobe of the liver has 4 segments: in the left lobe the first four, in the right - from V to VIII. The segments are distinguished based on the portal vein branch at their center and the hepatic vein at the periphery. Segment I (Fig. 1) is known as the caudate lobe (Spiegel's lobe). Rice.
1. Segmental structure of the liver.
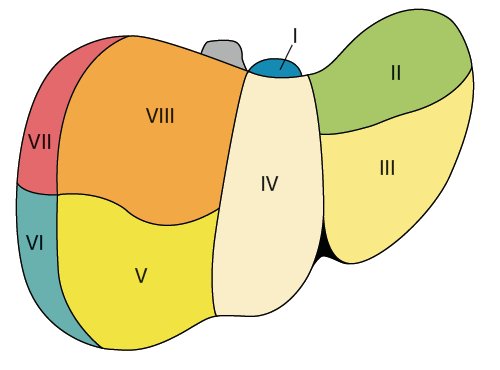
A)
View from the diaphragmatic surface.
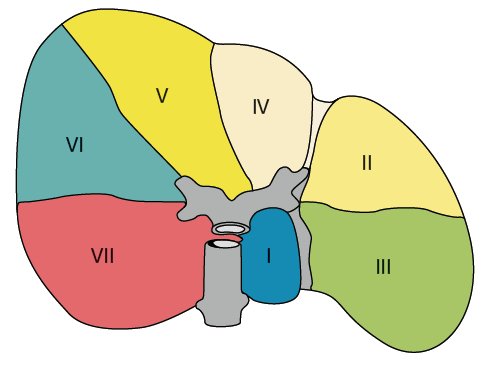
b)
View from the abdominal surface.
The branches of the portal vein arise in a shape resembling two lateral “H” letters, one of which supplies the left lobe (segments I-IV), the other the right (segments V-VIII). The “H” of the left lobe is best visualized using an oblique subxiphoid approach (Fig. 2). The falciform and venous (lesser omentum = hepatogastric ligament) ligaments are attached to this lateral “H”. The ligamentum venosum is the fibrous remnant of the ductus venosus, through which the fetus discharges blood from the left umbilical vein into the inferior vena cava. The venous ligament separates segment I from II, and the falciform ligament separates segment III from IV. Segment I (caudate lobe of the liver) is located behind the inferior vena cava, on the side of the venous ligament and in front of the left branch of the portal vein. A feature of segment I is the blood supply to the right and left branches of the portal vein (due to their small diameter, they are poorly visualized on ultrasound) and drainage directly into the inferior vena cava, bypassing the 3 main large hepatic veins. The portal vein, supplying segment II - a direct continuation of the left branch of the portal vein, forms the lower "stick" of the horizontally located "H". Another horizontal line is formed by the branches to segments III and IV. Segments II and III are located to the left of the venous and falciform ligaments. Segment IV, the quadrate lobe, is located to the right of the falciform ligament and is separated from segment I by the left branch of the portal vein [1].
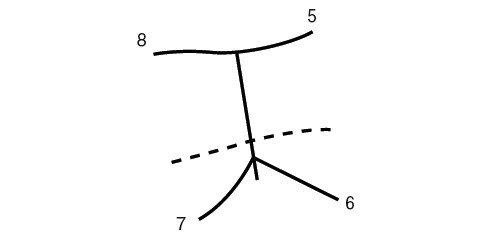
Rice. 2.
Schematic representation of the segmental branches of the portal vein of the left and right lobes of the liver.
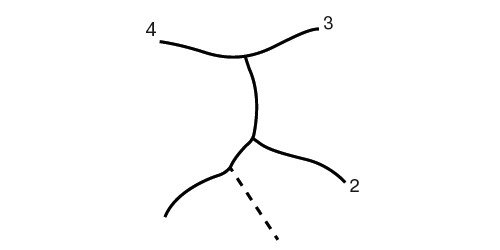
A)
Left lobe of the liver.
b)
Right lobe of the liver.
The right part of the portal vein and its branching to the segments are visualized using a sagittal or oblique mid-axillary intercostal approach. In children and gracile subjects, a subcostal approach is possible. The right branch of the portal vein is located obliquely forward or vertically. The branches of the right lobe of the portal vein leading to the segments also form the shape of the letter “H” located on the side (Fig. 2). The bridge between the legs of the letter “H” is formed by the right branch of the portal vein, the branches to segments V and VIII are the upper leg, the branches to segments VI and VII are located obliquely. Therefore, to visualize segment VI, the sensor must be directed towards the right kidney. The middle hepatic vein separates segments V and VIII from IV, the right - V and VIII segments from VI and VII. Segment V is located medial to the gallbladder. The right branch of the portal vein serves as the border between segments V and VIII. Segment VIII is separated from VII by the right hepatic vein, from IV by the middle hepatic vein. Segments VI and VII are separated from V and VIII by the right hepatic vein. Segment VI is directly adjacent to the kidney; its lateral border is the chest. The VII segment is separated from the VIII by the right hepatic vein, adjacent laterally to the ribs, caudally to the dome of the diaphragm.
The hepatic veins with an oblique subxiphoid coronary approach resemble the letter “W”, located with its base on the inferior vena cava. The left hepatic vein is the boundary between segments II and III, the middle one delimits the IV segment from V and VIII, the right - V and VIII segments from VI and VII. With an oblique subxiphoid approach, the right hepatic vein is clearly visualized, which makes it possible to distinguish the superficial V segment from the deep VIII.
A full-fledged ultrasound implies rigorous visualization of the branches of the portal vein, their segmental branches, and hepatic veins. This makes it possible to diagnose not only focal liver lesions, but also to detect thrombosis, compression of blood vessels by a space-occupying lesion or tumor growth into a vessel. A Doppler study completes the diagnostic procedure by determining the presence and direction of blood flow in the vessels. Next to the vascular bundle (hepatic artery and portal veins) are the bile ducts. They become visible when the outflow of bile is blocked [2].
Clinical problems
Jaundice of newborns
may be the result of parenchymal processes (hepatocellular) of an obstructive nature, hemolytic and septic origin.
The diagnosis must be established at the earliest possible date. If treatment of biliary obstruction or metabolic disorders does not begin within the next 2 months of life, fatal cirrhosis develops. Echography is the most important method for diagnosing the causes of hyperbilirubinemia in newborns. The technique allows you to speed up the differential diagnosis of intra- and extrahepatic obstruction of the bile ducts, including common bile duct cysts, spontaneous perforation of the bile duct, and atresia of the intrahepatic ducts. Other causes of obstruction of the biliary system (stones, tumors, congenital stenosis of the common bile duct) are rare in the neonatal period. Intrahepatic disorders can occur with intrahepatic atresia of the bile ducts, rarely with the development of fibrous tissue around the bile ducts due to a homozygous mutation of the cirrin gene CIRH1A on chromosome 16q22. In addition, newborn jaundice can be hepatocellular (viral, bacterial, fungal, parasitic hepatitis) or metabolic (fructose intolerance, α1-antitrypsin deficiency, cystic fibrosis). Cholestasis is accompanied by hemolysis, heart failure, shock, sepsis, and neonatal lupus [3, 4].
Jaundice is an indication for ultrasound. Dilatation of the intrahepatic ducts indicates extrahepatic obstruction of the bile ducts. If the cause of obstruction remains unclear, percutaneous cholangio or cholecystography is performed. Provided that the function of hepatocytes is preserved, the patency of the common bile duct can also be established by hepatobiliary scintigraphy [5]. Studies aimed at clarifying the nature of bile secretion, or scanning the gallbladder, are carried out after 3-5 days of prescribing phenobarbital as a stimulator of bile secretion [6]. At the final stage of diagnosis, a liver biopsy is possible. An echographic sign of biliary atresia is a cone-shaped compaction, visualized during transverse or longitudinal scanning and extending upward from the portal vein, especially in combination with a small gallbladder (longitudinal
Cysts of the biliary system.
The cause of jaundice in newborns and infants can also be an expansion of the common bile duct of varying degrees of severity and localization, known as common bile duct cysts. Common bile duct cysts can also be detected in older children. In this case, they manifest themselves as pain, jaundice, cholangitis, and very rarely - a palpable formation. As the cyst exists, the intrahepatic ducts may expand or stones may form in it. Echographically, cysts appear as thin-walled round formations in the area of the liver hilum or inside its parenchyma (Fig. 3). The gallbladder is visualized separately, which is very important for differential diagnosis [8]. For accurate mapping of the biliary system and the actual communication of the cyst with the bile ducts, scintigraphy, percutaneous cholecystocholangiography, and endoscopic retrograde cholecystopancreatography are performed before surgery.
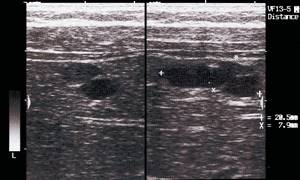
Rice. 3.
Echogram of congenital liver cysts in a 3-month-old child.
There are 5 types (Fig. 4) of bile duct cysts [9]:
- Type I Isolated extrahepatic cyst, cylindrical or saccular dilatation of the common bile duct. 80-90% of all cases of bile duct cysts. Possible spread of the cyst into the pancreatic duct with the formation of a common channel into the duodenum, flow of bile into the Wirsung duct, activation of pancreatic enzymes with pancreatic necrosis. Common bile duct cysts can sometimes be visualized in 15-week-old fetuses, when amylase is not yet secreted. Removal of the cyst is justified in a newborn, when the inflammatory reaction is minimal and chronic pancreatitis does not form. A common bile duct cyst appears to be a more realistic cause of chronic recurrent pancreatitis than the long-standing common bile-pancreatic duct theory. Other options for expansion (cysts) of the common bile duct are its partial atresia with expansion of the upstream part and atresia of the small intestine with the duct flowing into its blind part [10].
- Type II (2-3%) looks like multiple diverticula of the common bile duct.
- Type III (1-5%) - expansion of the intraduodenal segment.
- Type IV (10%) - multiple extra- and intrahepatic cysts.
- Type V - Caroli syndrome, cysts of small intrahepatic ducts [11]. Fibrosis is often one of the manifestations of polycystic disease. Echographically, cysts are detected around the branches of the portal vein. They are distinguished from veins based on Doppler ultrasound data (Fig. 5). Possible suppuration and liver abscess formation.
Rice. 4.
Schematic representation of diverticula of the biliary system.
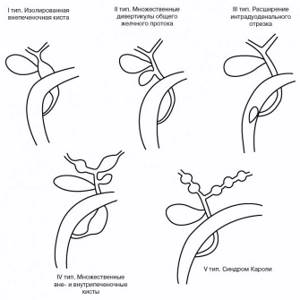
Type I - isolated extrahepatic cyst. Type II - multiple diverticula of the common bile duct. Type III - expansion of the intraduodenal segment. Type IV - multiple extra- and intrahepatic cysts. Type V - Caroli syndrome.
Rice. 5.
Echographic picture of Caroli syndrome.

A)
Dopplerography of the liver in Caroli syndrome. Blood flow in the veins is visible. At the same time, unevenly dilated bile ducts are visualized (the blood flow inside is not determined), highlighted with markers.
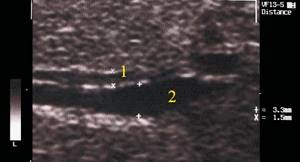
b)
Sonographic image of an unevenly dilated intrahepatic duct (2) next to a vein (1). The walls of the vein are denser.
There are other classifications that distinguish subtypes of cysts and a different number of types. But these variations are absolutely not important. Identifying cysts, their location, and answering questions about complications and prognosis are important.
Rarely, as a rule, in the area of the junction of the cystic and common bile ducts, spontaneous rupture of the bile duct is possible, which is clinically manifested by symptoms of an acute abdomen. Ultrasound examination reveals fluid around the gallbladder and free fluid in the abdominal cavity without dilatation of the ducts.
Alagille syndrome
- reduction in the number of intrahepatic bile ducts. A heterogeneous condition, transmitted autosomal dominantly with varying degrees of expressivity (heterozygous mutation of the JAG1 gene on chromosome 20p12 and, another option, mutation of the NOTCH2 gene). In various combinations and degrees of severity, it manifests itself as cholestasis, a small gallbladder (the result of bile retention in the liver), liver fibrosis, pulmonary valvular stenosis, ocular hypertelorism, skeletal abnormalities, absence of deep tendon reflexes, difficulty mastering the school curriculum, kidney dysplasia, etc. . Histologically, a sharp decrease in the number of intrahepatic ducts is detected. Echographically, the liver is enlarged, often due to the left lobe, portal hypertension is possible [12].
Atresia
intra- or extrahepatic bile ducts (1:10,000 live births, M=F) - absence or obliteration of bile ducts. Biliary cirrhosis of the liver develops rapidly. In 20% of those affected, it is combined with trisomy of the 17th or 18th chromosome, polysplenia, mirror arrangement of internal organs, segmental atresia of the inferior vena cava, and the location of the portal vein in front of the duodenum. There is an opinion about extrahepatic external causes of biliary atresia. This is supported by the absence of concomitant pathology of the pancreatic duct, which is formed simultaneously with the bile ducts, and the extreme rarity of the disease in fetuses and stillborns. It is believed that atresia occurs after the formation of the bile ducts due to infection entering the biliary system in utero with the development of inflammation and obliteration. A similar effect is known for carbamazepine. After birth, jaundice increases quickly, in the first 2-3 weeks. Echographically, the gallbladder is not visualized or its length is less than 1.5 cm, dilation of small intrahepatic ducts, a cone-shaped seal is visualized at the site of the common bile duct, spreading from the porta hepatis, polysplenia.
If atresia concerns only the extrahepatic ducts, there remains hope for surgical intervention and creation of an anastomosis to the duodenum. The operation should be performed no later than 2 months of life. Complete restoration of drainage can be achieved in 30% of cases, and partial restoration in another 30%. But even with a successful outcome of the operation, by the 20th year of life, 75% of those operated on develop liver failure, requiring liver transplantation [13, 14]. Intrahepatic atresia is fatal. Hypothetically, we can talk about liver transplantation along with the gallbladder, but in newborns such an operation is more than doubtful (Fig. 6).
Rice. 6.
Schematic representation of bile duct atresia.
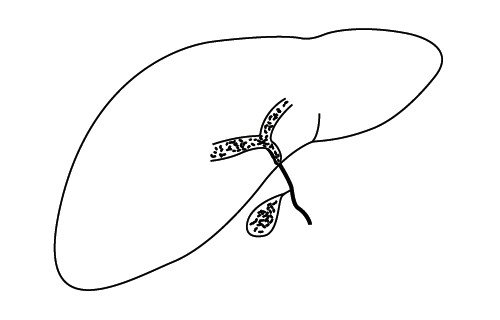
A)
Extrahepatic atresia of the bile ducts.
b)
Total atresia of the bile ducts.
Neonatal hepatitis
develops in the first 3 months of life. Bacteria and viruses penetrate the liver through the placenta, from the vagina, through an infected catheter, and during blood transfusion. Transplacental infection occurs in the last trimester of pregnancy. Bacterial hepatitis is secondary to infection from amniotic fluid, infected endometrium, placenta, and vagina. In multiple pregnancies, the fetus closest to the cervix is infected first. In this case, the most likely agents are Listeria and Escherichia coli. During vaginal delivery, the causative agents of hepatitis can be herpes viruses, cytomegaloviruses, immunodeficiency virus, listeria. Blood transfusions can cause infection with hepatitis B and C viruses, cytomegaloviruses, Ebstein-Barr, and HIV. When catheterizing the umbilical vein with an infected catheter, bacterial hepatitis and abscesses are typical. Ultrasound is low specific and is indicated for the purposes of differential diagnosis and exclusion of liver abscess. One finding may be thickening of the gallbladder walls (swelling due to hypoalbuminemia).
Sepsis, urinary tract infection and neonatal jaundice
are more often combined in boys than in girls. The younger the child, the less specific the symptoms. The infection is manifested by general lethargy, fever, vomiting, diarrhea, and hepatomegaly. Ultrasound is necessary to clarify the condition of the kidneys, bladder, and supradiaphragmatic space (pleurisy).
Congenital metabolic disorders
quickly lead to liver damage. Currently, many of them are successfully treated by eliminating certain foods, replacement diets, enzymes or medications. Therefore, pediatricians and imaging specialists should be well acquainted with the manifestations of inborn errors of metabolism. Hepatopathies accompanying congenital metabolic disorders arise as a result of the accumulation of toxins during the blockade of natural metabolism or the absence of enzymes that contribute to the destruction of toxins metabolized in the liver. With different types of metabolic disorders, the stages of liver damage may vary. For example, the most pronounced damage to hepatocytes is observed in glycogenosis type IV, galactosemia, fructose intolerance, tyrosinemia, Wilson's disease, the cytotoxic effect is less pronounced in glycogenosis types I and III, and α1-antitrypsin deficiency. The function of hepatocytes is preserved for a long time in Gaucher disease and mucopolysaccharidosis. With glycogenosis, galactosemia, tyrosinemia and cystic fibrosis, signs of steatosis prevail. The maximum risk of hepatocellular carcinoma is known with α1-antitrypsin deficiency, tyrosinemia, and type I glycogenosis. Liver adenoma is typical of tubulopathies with acidosis and nephrocalcinosis. The best treatment for tyrosinemia is transplantation. Drug therapy is indicated in the treatment of acute neurological crises due to tyrosinemia. The absolute indication for liver transplantation is the appearance of intrahepatic nodes, since hepatocarcinoma develops in 30% of children who survive the neonatal period. There are no absolute echographic signs that can reliably distinguish regenerative nodes from adenoma or carcinoma [15]. Ultrasound for suspected metabolic liver damage should include not only an assessment of the size and architecture of the liver (steatosis, cirrhosis, regeneration nodes), but also Dopplerography to exclude portal hypertension, as well as the condition of the kidneys (size, parenchyma condition).
Fatty degeneration (infiltration) of the liver (steatosis).
Fat accumulates in hepatocytes after they are damaged (fatty degeneration), with excess fat intake (infiltration) or with a deficiency of enzymes that mobilize fat from the liver. Many drugs (acetylsalicylic acid, valproate, warfarin, tetracycline), toxins (aflotoxin) and alcohol lead to fatty liver degeneration. Steatosis is characteristic of metabolic disorders (galactosemia, fructose intolerance), obesity, hereditary and acquired hyperlipidemia syndromes, and diabetes mellitus. In many diseases, the development of steatosis is due to several mechanisms, for example, in nephrotic syndrome, a violation of the removal of fat from the liver is combined with its increased entry into hepatocytes. In cases of parenteral nutrition in the absence of lipids, steatosis develops as a result of a deficiency of unsaturated fatty acids. Steatosis is reversible to a certain extent. Ultrasound allows you to diagnose steatosis at a subclinical level. Echographically, steatosis is manifested by an increase in the acoustic density of the liver, approaching the density of the vessel walls. The echogenicity of the renal cortex is significantly lower. Local (focal) steatosis looks like intrahepatic round or oblong formations with fairly even contours. In contrast, unchanged areas of the liver appear hypoechoic. The increased echogenicity of a steatotic liver can mask metastases and abscesses, so computed tomography is required if hepatic steatosis is suspected. Final verification of focal changes (for example, metastases) against the background of steatosis is possible only based on the results of a targeted biopsy [16]. With fatty infiltration of the liver, segments IV and V are least affected and last. This is explained by their blood supply through the branches of the cystic artery [17].
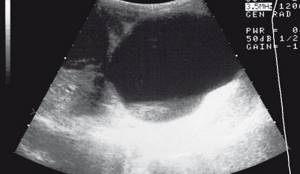
Cirrhosis of the liver
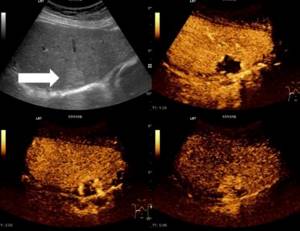
in children, as a rule, postnecrotic or biliary. Morphologically, cirrhosis looks like regeneration nodes, devoid of central veins, surrounded by fields of connective tissue. The natural architecture of the liver is altered, blood circulation is disrupted, and portal hypertension occurs. Echographically (Fig. 7), the acoustic density of the liver increases, ultrasound attenuation is clearly visible, and low-frequency transducers (2.5-3 MHz) are required to visualize the liver parenchyma. The echographic picture depends on the severity of cirrhosis. Initially, the parenchyma appears coarse-grained; as cirrhosis progresses, the liver surface becomes lumpy due to large foci of regeneration, the caudate lobe (liver segment I) increases in size, and fluid appears in the abdominal cavity.

Rice. 7.
Sonographic picture of liver cirrhosis. The liver is significantly heterogeneously compacted, the vascular pattern is deformed, and is surrounded by a rim of ascitic fluid.
Liver tumors
can reach large sizes with minimal clinical symptoms.


Rice. 8.
Sonographic image of a liver tumor (arrow).
Hepatocellular carcinoma
, the second most common malignant tumor. The maximum incidence is at the ages of 4-5 and 12-14 years. In 50% of patients, the tumor develops against the background of type I glycogenosis, tyrosinemia, α1-antitrypsin deficiency, posthepatitis or biliary cirrhosis, Alagille syndrome. The concentration of serum α-feto protein is increased. Ultrasound results reveal areas of heterogeneous echogenicity; calcification is rare. The tumor quickly grows into the portal veins. Pathological angioneogenesis in hepatocellular carcinoma, just like in hepatoblastoma, is manifested by a network of small vessels at the periphery of the tumor. There are no smooth muscle fibers in the wall of these vessels; according to Doppler ultrasound, peripheral resistance is insignificant, blood flow is rapid, its speed exceeds the aortic one [20].
Undifferentiated embryonal sarcoma
(malignant mesenchymoma) is a malignant variant of hamartoma. It is rare, mainly in children 6-10 years old. Progresses rapidly with the appearance of central necrosis and cysts. The concentration of serum α-feto protea was not changed. Echographically, a large heterogeneous formation is detected.
Biliary rhabdomyosarcoma
, a rare variant of primary rhabdomyosarcoma, originates from the biliary tract. The average age of patients is 3-4 years. Clinically manifested by dystrophy, abdominal pain, increase in its volume, hepatomegaly, intermittent obstructive jaundice. It is best visualized when localized inside the common bile duct. According to ultrasound, heterogeneous density, the upstream bile ducts are dilated. Metastasizes to the lungs and bones.
Metastases in the liver are typical for Wilms tumor, neuroblastoma, lymphomas and leukemias [21].
Slightly less than half (40%) of all primary liver tumors in children are benign. Up to 60% of all benign tumors are hemangiomas, mesenchymal gamaroma, adenomas and focal nodular hyperplasia [22].
Hemangiomas
- vascular-mesenchymal formations, characterized by intense imperfect angiogenesis, often multiple in various organs and on the skin. The resulting arteriovenous anastomosis can lead to heart failure and consumption thrombocytopenia. Infantile hemangioendothelioma echographically appears as solid masses, in some cases widespread, of varying echogenicity, sometimes with delicate linear foci of calcification [23, 24]. Dopplerography reveals intense blood flow in tortuous, randomly located vessels (Fig. 9). With massive arteriovenous discharge, the underlying aorta is reduced in diameter, the celiac trunk, hepatic artery and veins are enlarged. Along with embolization, treatment with propranolol is widely used [25]. Solitary cavernous hemangioma grows slowly and is generally more common in adults.
Rice. 9.
Ultrasound picture of liver hemangioma.

A)
echographically, against the background of parenchyma of heterogeneous density, a small cystic multi-chamber formation is visualized (highlighted with markers).
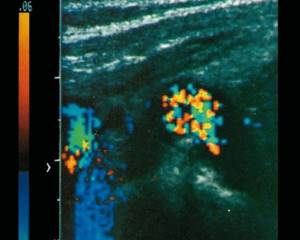
b)
Doppler sonography clearly shows a chaotic vortex-like blood flow.
Mesenchymal hamartoma
- a rare polycystic formation arising from the periportal mesenchyme. It is found more often in children during the first 2 years of life in the right lobe of the liver during random examinations [26].
Liver adenomas
, if they are not associated with glycogenosis type I, taking oral contraceptives, steroid therapy for Fanconi anemia, are extremely rare. Serum concentration of α-fetoprotein does not change. Sonographic signs of adenoma are nonspecific; the density may be hyper- or hypoechoic. Differential diagnosis of adenoma from a malignant neoplasm is possible only based on the results of a targeted biopsy.
Liver abscesses
in a previously healthy child are unlikely. They are formed during primary immunodeficiencies (for example, chronic granulomatous disease), immunodepression during chemotherapy, sepsis, cholangitis, appendicitis. Echographically, a mature abscess appears as a well-defined liquid formation, perhaps not sufficiently homogeneous due to detritus or thickening of pus. The vessels are displaced, but not invaded. Multiple small abscesses are typical of immunodeficiencies. Calcification is typical for them with successful treatment. In the diagnosis of small abscesses, CT or high-resolution MRI are more informative [27].
Parasitic abscesses
, first of all, a complication of amoebiasis. Amebiasis is an endemic tropical disease, but due to population migration, it can occur in any geographic region. It is transmitted from person to person when hygiene rules are violated. Entamoeba histo lytica, entering the digestive system, lingers in the large intestine, penetrates the mucosa and from there is transported through the mesenteric veins through the portal system to the liver. E. histolytica produces proteolytic enzymes, which leads to rapid abscess formation. Multiple liver abscesses are the most common extraintestinal complication of this infection, manifested by hepatomegaly and high fever without jaundice [28]. There are no specific echographic signs of amebic abscesses. The disease is complicated by spread to the abdominal cavity, subhepatic space, and neighboring organs.
Echinococcosis
liver looks like a cystic, clearly circumscribed formation (Fig. 10) with a visible wall and a delicate echo-negative rim [29, 30]. Small echo-positive structures (scollexes) can be visualized inside the echinococcal bladder. The preferred localization of the echinococcal bladder in the liver is not accidental. The liver, being the most important glycogen depot, does not consume it itself, but lives through the pentose cycle. It is from five-membered sugars (pentoses) that the outer shell of the hydatid bladder is built, protecting it from the human immune system. Thus, the parasite chooses the most optimal place for its development. After the death of the parasite during treatment or after removal of the bladder, a connective tissue scar remains.
Rice. 10.
Multiple echinococcosis of the liver.
Liver granulomas
on ultrasound they look like rounded echo-positive formations and can be bacterial (mycobacteriosis, listeriosis, spirochetosis), fungal (candidiasis, aspergillosis).
Literature
- Majno P., Mentha G., Toso Ch. et al. Anatomy of the liver: an outline with three levels of complexity - a furthe step to words tailorad territorial resection // J Hepatol. 2014; 60 (3): 654-662.1,5>
- Chamberlain R. Essential functionel hepatic and biliary anatomy for surgeon. 2013. https://dx.doi.org/10.5772/53849
- Pawlowska J., Jankowska I., Gliwicz D. et al. Rare hereditary intrahepatic cholestatic syndromes in children // Exp Clin Hepatol. 2010; 6 (2): 23-26.
- Santos J., Choquette M., Bezerra J. Cholestatic liver disease in children // Curr Gastroenterol. 2010; 12 (1): 30-39.
- O'Hara S. Pediatric liver and spleen. In: Carol R. (ed.). Diagnostic Ultrasound. Foot Edition. Mosby, 2011: 1800-1044.
- Ikeda S., Sera Y., Yamamoto H. et al. Effect of phenobarbital on serial ultrasonic examination in the evaluation of neonatal jaundice // Clin Imaging. 1994; 18 (2): 146-148.
- Kendrick A., Phua K., Ooi B. et al. Making the diagnosis of biliary atresia using the triangular cord sign and gallbladder length // Pediatr Radiol. 2000; 30 (2): 69-73.
- Gupta N., Javed A., Puris S. et al. Imaging of multiple intrahepatic cysts // Oman Med J. 2012; 27 (5): 421-423.
- Todani T., Watanabe Y., Narusue M. et al. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases // Am J Surg. 1977; 143(2):263-269.
- McHugh K., Daneman A. Multiple gastrointestinal atresias: sonography of associated biliary abnormalities // Pediatr Radiol. 1991; 21: 355-357.
- Senyuz O., Yesildag E., Kuruoglu S. et al. Carolis disease in children: is it common misdiagnosed? // Acta Pediatr. 2005; 94 (1): 117-120.
- Zissimopoulus A., Cassimos D., Deftereous S. et al. Hepatobiliary scan in Alagille syndrome: arteriohepatic dysplasia // Hell J Nucl Med. 2009; 12 (2): 158-160.
- Kasai M., Suzuki H., Ohashi E. et al. Technique and results of operative management of biliary atresia // World J Surg. 1978; 2 (5): 571-579.
- Bezerra J., Balistreri W. Cholestatic syndromes of infancy and childhood // Semin Gastrointest Dis. 2001; 12 (2): 54-65.
- Dubois J., Garel L., Patriquin H. et al. Imaging features of type 1 hereditary tyrosinemia: a review of 30 patients // Pediatr Radiol. 1996; 26 (12): 845-851.
- Ozcan N., Oguz B., Hallilooglu M. et al. Imaging patterns of fatty liver in pediatric patients // Diagnostic Intervent. Radiol. 2014; 21 (4): 355-360.
- Aubin B., Denys A., Lafortune M. et al. Focal sparing of liver parenchyma in steatosis: role of the gallbladder and its vessels // J Ultrasound Med. 1995; 14 (2): 77-80.
- Dachman A., Pakter R., Ros P. et al. Hepa toblastoma: radiologic-pathologic correlation in 50 cases // Radiology. 1987; 164 (1): 15-19.
- Campenhout Van I., Patriquin H. Malignant microvasculature in abdominal tumors in children: detection with Doppler sonography // Radiology. 1992; 183(2):445-448.
- Meyers R. Tumors of the liver in children // Surg Oncol. 2007; 16 (3): 195-203.
- Fernandes-Pinedal I., Cabello-Laureano R. Differential diagnosis and management of liver tumors in infants // World J Hepatol. 2014; 6 (7): 486-495.
- Isaacs Jr. Fetal and neonatal hepatic tumors // J Pediatr Surg. 2007; 42 (11): 1797-1803.
- Kassarjian A., Zurakowsky D., Dubois J. et al. Infantile hepatic hemangiomas: clinical and imaging findings and the correlation with therapy // Am J Roentgenol. 2004; 182(3):785-795.
- Dachman A., Lichtenstein J., Friedman A., Hartman D. Infantile hemangioendothelioma of the liver: a radiologic-pathologic-clinical correlation // Am J Roentgenol. 1983; 140(6):1091-1096.
- Cavalli R., Novotna V., Boffun R., Gelletti C. Multiple cutaneous and hepatic infantile hemangiomas having a successful response to propronalole as monotherapy during the neonatal period // G Ital Dermatol Venerol. 2013; 148(5):525-530.
- Ross P., Goodman Z., Ishak K. et al. Mesenchymal hamartoma of the liver: radiologic-pathologic correlation // Radiology. 1986; 158(3):619-624.
- Salahi R., Dehghani S., Salahi S. et al. Liver abscesses in children: a 10-ear single center experience // Saudi J Gastroenterol. 2011; 17 (3): 199-202.
- Stanley S. Amoebiasis // Lancet. 2003; 361 (9362): 1025-1034.
- Czermak B., Akhan O., Hiemetzberger R. et al. Echinococcus of the liver // Abdominal Imaging. 2008; 33 (2): 133-143.
- Macpherson C., Bartholomot B., Frider B. Application of ultrasound in diagnosis, treatment, epidemiology, public health and control of Echinococcus granulosis and E. multilocularis // Pa ra si tolo gy. 2007; 127 Suppl: S21-35.

Ultrasound machine HS40
Top seller in high class.
21.5″ high-definition monitor, advanced cardio package (Strain+, Stress Echo), expert capabilities for 3D ultrasound in obstetrics and gynecology practice (STIC, Crystal Vue, 5D Follicle), high-density sensors.