If protein and leukocytes are in the urine
are in increased content, this may be a sign of the development of serious pathological diseases. Urinalysis is a basic laboratory test designed to diagnose various diseases. From its composition you can read about the functioning of the kidneys and the condition of the urinary tract.
When carrying out the analysis, such features as color, smell, transparency, density, and acidity are taken into account. Each of these indicators has its own norms and deviations. And they also talk about the presence of certain diseases or changes occurring in the body.
What are leukocytes, their norm in urine
Leukocytes are white blood cells that provide the body's immune system with a response to invading pathogenic agents. They are produced in the bone marrow and have a lifespan of about 7 days. Leukocytes travel with the blood and participate in the absorption of foreign elements. Having done their work, the cells die. They are removed from the body along with urine. The urine of a healthy person contains no more than 3-5 units in the field of view.
In men, the norm of leukocytes in the urine is 0-3, in women - 0-5, in girls 0-7, in boys 0-5 units in the field of view. The absence of cells is a variant of the norm.
If a large number of white blood cells (leukocyturia) are found in the urine, then an inflammatory or infectious process is occurring in the body. Any pathological conditions activate the production of leukocytes, and, as a result, an increase in their concentration.
The body signals a health problem by increasing temperature and fever, deterioration in overall health, and changes in the color and transparency of urine.
The pathological condition is detected using OAM (general analysis of morning urine). To confirm/refute the diagnosis, the doctor will additionally prescribe a Nechiporenko test and a general blood test with a leukocyte formula. A nephrologist, urologist, pediatrician or general practitioner, gynecologist or oncologist deciphers the test results.
Thrombocytopenia
HIV
Hepatitis
Iron deficiency
13119 August 12
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Thrombocytopenia: causes of occurrence, in what diseases it occurs, diagnosis and treatment methods.
Definition
Platelets are plate-shaped blood cells that participate in blood clotting processes. Their main function is to close a wound when bleeding by forming a thrombus, or blood clot. Thrombosis is a natural process of protection against massive blood loss in any injury. A deficiency of platelets in the blood is called thrombocytopenia. This condition is often asymptomatic, but can be life-threatening if the number of blood platelets decreases significantly.
In addition to stopping bleeding (hemostasis), platelets perform a number of important functions in the human body: releasing substances that constrict blood vessels during bleeding; stimulation of tissue repair in case of any injury; regulation of local inflammation and immunity processes.
These functions are activated when there is any damage to the endothelium (the inner layer covering the walls of blood vessels). A lack of platelets leads to a disruption of the blood coagulation system and, as a result, increased bleeding, hematomas (bruises) and a dark red rash on the skin and mucous membranes (this rash does not disappear with pressure).
Prolonged bleeding of the gums, large amounts of bleeding from small wounds and during menstruation are an alarming signal indicating a possible problem with the blood coagulation system.
Types of thrombocytopenia
Thrombocytopenia is understood as a decrease in the number of platelets in the peripheral blood below 150 thousand/μl. Among all thrombocytopenias, the following conditions are distinguished:
- Dilution thrombocytopenia - occurs with massive bleeding and replenishment of the circulating blood volume with solutions.
- Thrombocytopenia of distribution - often occurs with excessive pathological utilization of platelets in an enlarged spleen.
- Productive thrombocytopenia occurs when bone marrow function is impaired as a result of various diseases or radiation therapy.
- Thrombocytopenia of consumption - occurs with DIC syndrome (disseminated intravascular coagulation - a pathological condition when blood clots form in the bloodstream of many organs) or with constant autoimmune damage to the vascular endothelium. There is a pathological activation of platelets and their rapid consumption (consumption) by the body.
- Pseudothrombocytopenia occurs when the analysis technique is violated with the development of platelet aggregation.
Possible causes of thrombocytopenia
One of the common causes of thrombocytopenia is excessive platelet consumption
in the body, for example, with DIC syndrome.
Immune form of thrombocytopenia
is considered the most common immune blood pathology. It develops quickly, with a rise in body temperature and the appearance of a profuse rash on the skin of the lower extremities, buttocks, around large joints, sometimes reaching the face. The rash consists of small hemorrhages in the skin, often accompanied by joint pain, swelling, and loss of movement in the affected joints. Sometimes it manifests itself as cramping abdominal pain, nausea, vomiting and loose stools. Cases of blood appearing in the urine have been described.
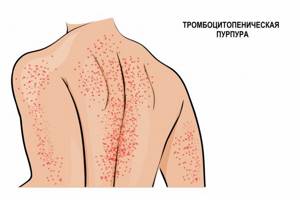
Autoimmune thrombocytopenia
(idiopathic thrombocytopenic purpura, Werlhof's disease) is caused by a decrease in platelet lifespan due to the effects of antiplatelet autoantibodies. Such thrombocytopenia can occur in waves, with alternating periods of exacerbation and remission. Often the disease makes itself felt against the background of infectious diseases: influenza, human immunodeficiency virus (HIV), Epstein-Barr virus (EBV), parvovirus B19, cytomegalovirus infection (CMV), viral hepatitis B and C.
Among productive thrombocytopenias
Aplastic anemia, tumor processes in the bone marrow, and radiation injuries occupy a special place.
All of these conditions are characterized by a sharp decrease in the hematopoietic (hematopoietic) function of the bone marrow due to certain structural changes.
Aplastic anemia
is characterized by a decrease in the production of all three hematopoietic lineages: red blood cells, leukocytes and platelets. Each germ is responsible for specific functions in the body, and a decrease in the cells produced leads to the appearance of corresponding symptoms. A decrease in platelets leads to increased bleeding, a decrease in the number of red blood cells indicates signs of anemia (pallor, fatigue, brittle hair, chest pain), and a decrease in leukocytes leads to infectious complications in the form of recurrent sore throats, pneumonia, etc. In some cases, the bone marrow is replaced by fatty tissue tissue, which also disrupts the formation of blood cells.
For B12 and folate deficiency anemia
the maturation of future platelets is disrupted; they die even before the maturation stage. The disease is manifested by pale skin, rapid heartbeat, and shortness of breath. With a severe deficiency of vitamin B12, sensory disturbances, paresis and paralysis are possible.
Different types of leukemia
lead to the appearance of tumor cells, which divide at tremendous speed and soon replace the bone marrow. In this case, the function of all three hematopoietic germs is disrupted. Immature cells appear in the bone marrow and blood, unable to perform their function.
Drug-induced thrombocytopenia
may develop as a result of taking certain medications, for example, cytostatics, which inhibit platelet formation in the bone marrow.
Diseases accompanied by an increase in the size of the spleen
(splenomegaly) can lead to increased destruction of platelets, or hypersplenism (increased platelet utilization by the spleen). In addition to platelets, red blood cells are also destroyed, which leads to the development of not only a thrombocytopenic state, but also to hemolytic anemia.
Such diseases include liver cirrhosis, including alcohol etiology, chronic heart failure, and lymphoproliferative diseases.
Which doctors should you contact if you have thrombocytopenia
? The diagnosis of thrombocytopenia is established using laboratory tests. Most often, patients who subsequently develop thrombocytopenia come to us with complaints of increased bleeding, rash, malaise, and fatigue. If a decrease in platelet count is detected, the therapist will prescribe a consultation with a hematologist. In some cases, consultation with a hepatologist or rheumatologist is required.
Diagnosis and examinations for thrombocytopenia
If signs of thrombocytopenia are detected, the doctor will prescribe a set of laboratory and instrumental research methods:
- clinical blood test: general analysis with platelet count, leukoformula, ESR (with blood smear microscopy in the presence of pathological changes);
When to determine the number of leukocytes in urine
General indications for taking a urine test are:
- examination for infectious diseases and inflammatory processes;
- the need to establish an accurate diagnosis if diseases of the urinary system are suspected;
- examination of pregnant women before registration at the antenatal clinic, routine examinations;
- the occurrence of complications during pregnancy, suspicion of gestosis;
- the need to evaluate the effectiveness of prescribed treatment, including antibiotic therapy;
- undergoing routine medical examinations;
- diagnosing diseases in children;
- monitoring the condition of patients with cancer.
White blood cells in urine should be checked if the following symptoms occur:
- acute pain in the lower abdomen, under the right rib or in the lower back;
- frequent urination;
- a feeling of incomplete emptying of the bladder;
- discomfort, pain, burning and itching when urinating;
- darkening of urine, appearance of an unpleasant odor;
- the appearance of foreign inclusions in urine (blood clots, mucus, flakes);
- increased temperature and fever of unknown origin;
- increased blood pressure.
Sluggish or chronic disease of the urinary organs can be suspected when yellowish spots are found on underwear.
How urine is formed

Urine formation occurs in the kidneys as a result of blood filtration. The process takes place in 2 stages. At the first stage, primary urine exits through the walls of the glomerular capillaries. Essentially, it is water with amino acids, vitamins, minerals, uric acid and urea (about 150 l/day).
In the renal tubules, reverse absorption (reabsorption) of substances necessary for the body occurs, resulting in the formation of secondary urine (about 1.5 l/day). It contains a lot of urea and uric acid, potassium, as well as toxic metabolic products. The composition of urine is determined by environmental factors and the characteristics of the body.
With organic changes in the kidneys, disturbances in the nervous and humoral regulation of their activity, the blood filtration process is disrupted. As a result, components that should not be in it (glucose, albumin, blood cells, etc.) get into the urine. Thus, by the composition of urine, you can evaluate the functioning of the urinary system and diagnose some diseases.
What amount is considered elevated?
It can be stated that leukocytes in the urine are elevated if up to 20 copies are detected. If the number reaches 85-100, then we can talk about an acute disease of the genitourinary system and the presence of pus in the urine. The pathology is called pyuria. In this case, the liquid becomes dark in color, becomes cloudy and has a purulent odor. Upon examination, impurities are detected.
In order not to distort the test result, on the eve of urine collection it is important to exclude the influence of the following factors:
- abuse of fatty, protein foods;
- diaper rash in babies;
- poor genital hygiene;
- severe dehydration;
- pathological vaginal dryness during menopause.
High white blood cells can be caused by the presence of a bladder catheter, as well as the use of certain pharmaceuticals: diuretics, NSAIDs, antibiotics and drugs that suppress the immune system.
How to find the exact cause - examination
If a laboratory test shows the content of blood and protein in the urine, you should urgently contact a urologist or nephrologist. After analyzing complaints, anamnesis, and physical examination data, the doctor prescribes a comprehensive examination. Typically, when blood and protein are detected in the urine of women and men, the following is prescribed:
- general analysis of urine and blood;
- Ultrasound of the kidneys, bladder, pelvic organs.
Further examination depends on the results of basic diagnostic procedures. It is possible to prescribe additional laboratory tests, urodynamics, computed tomography or magnetic resonance imaging.
Types of leukocyturia
Depending on the number of white blood cells, three types of leukocyturia are distinguished:
- insignificant (from 7 to 40 units);
- moderate (up to 100 specimens in the field of view);
- pronounced (over 100 units).
A high concentration of white blood cells in the urine may be:
- caused by diseases of the urinary system (true) or arising against the background of an inflammatory process in the genital organs (false);
- infectious or non-infectious origin. In the first case, the presence of infection is confirmed by urine culture or PCR diagnostics. Non-infectious leukocyturia is not associated with bacterial activity; it is caused by an inflammatory process due to allergic cystitis, autoimmune glomerulonephritis, and medications.
Depending on the predominant type of leukocytes, they are distinguished:
- lymphocytic leukocyturia, giving reason to suspect lupus erythematosus or rheumatoid arthritis;
- mononuclear, arising from renal pathologies;
- neutrophilic, which is provoked by tuberculosis, tonsillitis, malaria or pyelonephritis;
- eosinophilic, accompanies allergies.
What diseases cause an increase in leukocytes in the urine?
A large number of diseases can cause an increase in the concentration of leukocytes in the urine. If the analysis shows deviations from the norm, then it is necessary to undergo further examination to exclude serious diseases, and if they are confirmed, begin timely treatment.
The main diseases in which leukocyturia is detected:
- pathologies of the urinary tract: cystitis, urethritis, pyelonephritis, glomerulonephritis, stones in the bladder or kidneys, cystic formations, abscess of kidney tissue, damage to the renal vessels in diabetes mellitus;
- pathologies of the female genital organs: vaginitis, thrush, inflammatory processes in the uterine appendages, bartholinitis, endometritis;
- pathologies of the male genital organs: adenoma, inflammatory process in the prostate gland, balanoposthitis, infectious diseases;
- other diseases: autoimmune origin, cancer, gallstones, pneumonia, diabetes, various allergies, heart and vascular diseases, appendicitis.
Why does blood appear in urine?
The presence of blood in the urine is a symptom of problems with the kidneys and lower urinary tract. If blood is detected visually in urine, we speak of gross hematuria. The symptom may appear as follows:
- red, brown, pink color of urine;
- red blood clots;
- thin thread-like black inclusions.
Whole blood enters the urine when blood vessels are damaged. This happens in the background:
- infectious and inflammatory diseases of the upper and lower urinary organs, accompanied by damage to the mucous membranes;
- mechanical injuries (as a result of an impact, injury, foreign body, or when stones pass through the ducts);
- progression of tumor diseases (kidney, bladder, prostate cancer).
Blood in the urine must be distinguished from specific staining as a result of taking medications or eating certain foods. So, urine turns red as a result of eating beets, rhubarb, and some red berries.
If blood is detected in a urine test only microscopically (during laboratory analysis), we speak of microhematuria. The term means that blood cells, in particular red blood cells, enter the urine. The amount may be insignificant, so urine coloring does not occur. The symptom is often the first sign of the development of glomerulonephritis - an inflammatory lesion of the filtration system of the kidneys, in which the permeability of the capillary walls is significantly impaired and red blood cells pass through them into the urine.
If you have any questions, call us at: +7 Medical administrators are always ready to advise you.
Why do leukocytes increase in pregnant women?
OAM is a mandatory test prescribed for pregnant women. In the third trimester, indicators must be monitored weekly.
Due to the fact that the antigenic load on the body increases, a slight excess of the leukocyte norm is allowed in the tests.
A sharp increase in concentration gives the doctor reason to suspect:
- diabetes mellitus in pregnancy;
- diseases of the urinary system (cystitis or pyelonephritis);
- complication in the form of severe kidney damage;
- thrush;
- disturbance of bladder tone.
Possible pathological reasons for the presence of blood and protein in the urine

The most common reasons:
- Urinary tract infection (urethritis, cystitis). The condition is manifested by pain and stinging when urinating, and frequent urges.
- Injury. If you fall, bruise the abdomen and lumbar region, the kidneys can be injured.
- Kidney stone disease. Stones can damage the kidney tissue, which leads to the release of blood cells and proteins into the urine.
- Pyelonephritis. Infectious damage to the kidneys may be caused by the spread of infection from the lower parts of the urogenital tract.
- Glomerulonephritis. Damage to the renal filtration system is accompanied by microhematuria and proteinuria.
- Prostate pathologies. When prostate tissue is damaged, blood can enter the urinary tract and exit in the urine.