Cystic transformation of the ovaries is a common disease characterized by the appearance of formations with fluid in the structure of the organ. They occur asymptomatically and are not accompanied by pathological cell growth. The most common, in about 80 out of 100% of cases, is a follicular ovarian cyst. It occurs in young women and is directly related to their reproductive function, because the pathology appears at the site of the maturing follicle.
It is necessary to distinguish between cysts and cystomas
A cyst is not a true ovarian tumor. It can be formed directly from the structure of the ovary or “accompany” it (paraovarian, endometrioid). Occurs on one or both ovaries. The shell (capsule) of the cyst consists of connective tissue, so it does not grow, but is only stretched by the accumulating contents. Therefore, cysts can rupture and twist.
Cystoma is a true ovarian tumor that can grow rapidly autonomously, germinate into other tissues, and also develop into a malignant tumor.

Ovarian cyst
By the time of birth, the ovary is fully formed and contains in the cortical layer a supply of follicles (Folliculus), which are consumed throughout the woman’s life, and in the medulla - connective tissue, blood vessels and nerve endings, which ensures the functioning of the organ.

Follicular cyst - brief diagram
With normal functioning of the ovaries, the process of folliculogenesis occurs continuously, from birth to the postmenopausal period. Some follicles undergo reverse development - atresia, while the rest undergo a full growth cycle, ovulation and transformation into the “corpus luteum”. In atresia, an important role is played by a process such as apoptosis - programmed cell death, resulting in complete resorption of the cell under the influence of the body's own factors. If this process is disrupted, then the mechanism of formation of neoplasms is triggered.
The occurrence of a cyst on the right or left ovary is most often caused by hormonal disorders in the female body, but the mechanism of the appearance of cysts has not yet been fully established.
Diagnostic methods
In order for a doctor to choose an effective and safe treatment plan, he must first confirm the diagnosis. For this purpose, a referral is given for a comprehensive diagnostic examination.
Examination by a gynecologist
During the initial examination, the specialist carefully listens to the patient’s complaints, collects all the necessary data, and asks questions that are important to answer honestly. Then the specialist performs palpation, during which a tumor is detected in the projection of the appendages, its size and location are assessed. To determine the type of cyst and exclude the presence of cancer cells in it, additional laboratory and instrumental diagnostics are performed.
Laboratory diagnostics
A blood test for tumor markers CA-125, CA-19 will help to exclude or confirm cancer processes in the cyst. The SA-125 marker is the most important, but it has its own characteristics. This tumor marker is present in the blood in some benign tumors, as well as in oncological processes in the intestines, liver, and stomach. In any case, an increase in CA-125 indicates a pathological process in the body that requires more detailed study.
Ultrasonography
A safe, painless and non-invasive method, widely used in gynecology for diagnosing various pathologies. Preference is given to transvaginal ultrasound, during which a special sensor is inserted into the vagina, thereby being located as close as possible to the suspected pathological area. An ovarian cyst looks like a hypoechoic neoplasm containing fluid inside. To exclude a malignant tumor, Doppler ultrasound is additionally used. The presence of atypical blood flow testifies in favor of oncological formation.
Laparoscopy
A surgical diagnostic method, which is prescribed when it is impossible to determine an accurate diagnosis using the above research methods. The procedure is also indicated for suspected progression of malignant processes.
During the procedure, the surgeon performs a general examination of the tumor and then excises suspicious tissue for further histological examination. If the cyst is benign, it is removed during diagnostic laparoscopy.
Types of ovarian cysts
Ovarian cysts are divided into several types, according to their origin and the nature of the contents. It must be borne in mind that cysts classified as functional (follicular and corpus luteum cysts) in the vast majority of cases disappear on their own, without requiring any intervention in the body. After the appearance of such cysts, they simply resolve within 2-3 months and do not cause any concern.
What causes ovarian cysts?
Let's look at the most common cysts:
Functional ovarian cysts
Corpus luteum cyst of the ovary is a type of functional formation. It is formed at the site where the egg leaves the follicle after ovulation. Normally, the size of the “corpus luteum” is from 17 to 25 mm; anything exceeding this size is called a cystic formation or “corpus luteum cyst.” They can reach a diameter of about 5-6 cm. During physical activity or intense sexual contact, hemorrhage into the cyst or rupture of its capsule may occur, which will require emergency surgery, as it will cause intra-abdominal bleeding and a risk to the woman’s life. In such a situation, sharp pain, nausea, vomiting, and loss of consciousness appear.
Follicular cyst
This cyst belongs to the category of functional formations. This type of ovarian cyst appears most often at a young age as a result of failed ovulation, further growth of the follicle and accumulation of fluid in its cavity. Normally, the dominant follicle is 17-23 mm in size and ovulates between days 11 and 14 of the cycle. If it exists longer, does not ovulate and its size exceeds those indicated, then we are talking about a follicular cyst (Cysta ovarii follicularis), the diameter of which can reach 8-10-12 cm.
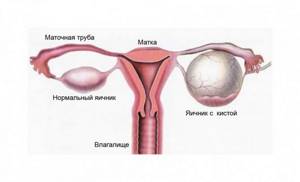
Paraovarian cyst
This type of cyst “accompanies” the ovary and can be located between the ligaments. It is characterized by the presence of one capsule (its size is usually from 2 to 10 cm), inside containing a clear liquid, which contains a small amount of protein. The development of the cyst is asymptomatic; nagging pain in the lower abdomen is less common. The cyst develops slowly, due to which its appearance can be diagnosed only by ultrasound or during a gynecological examination.
Endometrioid cyst
A cyst that is a direct consequence of endometriosis in the ovaries. These are “stray endometrial cells” that obey the general laws of regulation of the menstrual cycle. During menstruation, cells are destroyed and accumulate in a lesion limited by the capsule. Over time, the blood thickens, reduces and may resemble chocolate. Symptoms of such cysts usually include aching pain in the lower abdomen on the eve of menstruation, dyspareunia - pain during intimate relationships and fear of pain. Such cysts are benign, but can transform into malignant under unfavorable conditions (endometrioid cancer). Treatment in this case is often surgical. It is important to do this in a timely manner, since if the disease is neglected, adhesions in the pelvis and infertility may occur.
Dermoid cyst
Such an ovarian cyst extremely rarely develops into a malignant form. It represents the rudiments of adnexal tissues, which are surrounded by a thick capsule. This capsule may contain adipose tissue, the rudiments of teeth, bones, and hair. A dermoid cyst grows very slowly, however, when it reaches a large size, the cyst can put pressure on neighboring organs, disrupting their normal functioning, causing atrophy and replacement of functioning ovarian tissue.
Cytadenoma (cystoma)
Their second name is true cysts. Cytadenomas are one or a series of chambers. Depending on the contents of these chambers, true cysts are divided into serous and mucinous. Diagnosis of such a formation is often a direct indication for surgical treatment.
Cystic formations during menopause
Menopause is a special stage in a woman’s life, a time when the functions of the reproductive system gradually fade away. For most representatives of the fairer sex, menopause occurs at the age of 45–50 years, it all depends on the individual characteristics of each specific organism.
During menopause, hormonal deficiency develops, the general condition of the woman changes, and the risk of developing gynecological diseases characteristic of menopause increases. An ovarian cyst in menopause occurs due to hormonal changes. The work of the ovaries is inhibited, but ovulation occurs periodically, which becomes one of the main reasons for the formation of functional cysts, such as:
- Follicular. It is formed from a follicle that has not gone through a full stage of development and has not become dominant. As a result, the female reproductive cell is not formed, ovulation does not occur, menstruation does not occur, and in place of the follicle a capsule with liquid serous contents is formed.
- Luteal. It is formed from the corpus luteum, which, in the absence of fertilization, has not regressed. This cyst is characterized by slow growth and a tendency to self-resorption.
Functional cysts almost always resolve on their own, but sometimes they grow to large sizes, causing complications.
After a woman stops menstruating, functional cysts do not form. During this period, neoplasms of a different nature may form in the appendages:
- Serous cyst. Diagnosed more often than others. It is a dense capsule with watery contents.
- Dermoid. The beginnings of a tumor appear in a girl’s body during prenatal development. Such a cyst contains various fragments of embryonic tissue: hair, nails, teeth, nerve fibers, etc.
- Paraovarian. It occurs as a result of improper development of the epididymal tubules. This type of neoplasm does not lead to malignancy, but there is a risk of rupture and torsion of the leg. These types of cysts are not prone to self-resorption and require only surgical treatment.
Causes of ovarian cysts
What causes ovarian cysts?
As mentioned above, the causes of ovarian cysts are not fully understood. Scientists note a significant impact of imbalance of apoptosis and the balance of sex hormones in a woman’s body. Also, in the anamnesis of patients who have been diagnosed with ovarian cysts, inflammatory diseases of the female genital organs and endocrine diseases are often noted. Additional factors that provoke the appearance of cysts include:
- smoking and alcohol abuse;
- excess body weight or, conversely, excessively low weight;
- climate change;
- depression and stress, overwork;
- early onset of sexual activity;
- serious physical activity.
It is worth noting that no one is immune from the appearance of ovarian cysts. A gynecologist can detect a cyst in both a young woman and an elderly woman, so timely diagnosis and careful attention to your body are especially important.
Causes of pathology
The exact causes of this gynecological disease have not been fully established. Doctors cannot explain why an ovarian cyst develops during menopause - a period when reproductive function fades and the appendages cease to function fully. However, experts were able to identify a number of predisposing factors contributing to the onset of the disease:
- numerous abortions, miscarriages, premature births;
- chronic infectious and inflammatory pathologies of the genitourinary system;
- complicated childbirth;
- previous surgical intervention on the pelvic and abdominal organs;
- endocrine disorders such as hypothyroidism, adrenal insufficiency;
- uncontrolled use of hormone-containing drugs that affect a woman’s hormonal levels;
- early menopause - up to 40 years;
- refusal to become pregnant at fertile age.
Symptoms and signs of ovarian cyst
If you suspect an ovarian cyst...
The most common situation is the asymptomatic process of occurrence and resorption of ovarian cysts. Such neoplasms are usually detected during an ultrasound scan or during regular preventive examinations. However, sometimes the presence of a cyst makes itself felt by a number of symptoms:
- aching and nagging pain localized in the lower abdomen;
- increased pain during sexual intercourse;
- feeling of heaviness in the lower abdomen;
- dysfunctional uterine bleeding;
- pressure when emptying the bowel or bladder;
- nausea or vomiting, especially during exercise;
- menstrual irregularities leading to amenorrhea (Amenorrhea).
In addition to the above signs, there are a number of symptoms of the development of cysts, in which a visit to a doctor should be urgent:
- an obvious lump in the abdominal cavity that can be felt with your hands;
- high temperature (above 38°C) with persistent pain in the lower abdomen;
- acyclic uterine bleeding;
- weakness, dizziness, weight loss, severe thirst with excessive urination.
The above symptoms may be a sign of a ruptured ovarian cyst. This can be a real threat to life.
Clinical features of ovarian cysts in menopause
In the initial stages of development, cystic neoplasms do not cause any alarming symptoms. As they increase, disruptions in the menstrual cycle are observed. But during menopause, this symptom does not always cause concern, since at this time, irregular and periodic delays in menstruation do not frighten a woman.
Another symptom indicating the progression of the pathology is the appearance of spotting, not associated with menstruation. But even this symptom often goes unnoticed, since during menopause such discharge can appear periodically. You should be wary of symptoms that develop simultaneously with the above symptoms. It is better not to delay visiting a doctor if you are additionally concerned about the following symptoms:
- Pain in the lower abdomen. Discomfort indicates that the cyst has reached a large size - more than 5 cm and is compressing nearby nerve endings. A gradual increase in pain is an alarming sign indicating the development of complications.
- Problems with urination and bowel movements. A large tumor puts pressure on nearby organs - the bladder and intestines, disrupting their normal functioning. As a result, the urge to urinate becomes more frequent, and incontinence is possible. When the colon is clamped, chronic constipation is a concern, which cannot be eliminated with diet and special medications.
- Abdominal asymmetry. Giant cysts cause bloating and asymmetry of the abdomen.
Diagnosis of ovarian cysts - what tests and studies are performed?
A doctor can make an assumption about the occurrence of an ovarian cyst even with a routine manual examination. However, to make an accurate diagnosis of a cyst, an ultrasound examination is always prescribed. Ultrasound of the ovaries allows you to accurately determine the location and size of the cyst, make assumptions about its type and the need for surgical intervention or the use of conservative therapy. Typically, on ultrasound, an ovarian cyst appears as an anechoic formation - a dark spot.
As additional measures for diagnosing ovarian cysts, modern medicine uses:
- laparoscopy;
- computed tomography of the ovaries;
- magnetic resonance imaging;
- tests for sex hormone levels;
- tests to identify the tumor marker CA-125, reflecting the activity of the process, HE-4 preclinical form of cancer;
- puncture of the pouch of Douglas, used in cases of suspected cyst rupture and internal bleeding.
Expert opinion
In addition to the above research methods, if a pathological cyst is suspected, a CT or MRI with contrast is performed. The accumulation of contrast agent in a cyst may indirectly indicate its atypical nature. In this case, additional studies are carried out - for example, on tumor markers.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
It is worth keeping in mind that when diagnosing an ovarian cyst in a woman of reproductive age, watchful waiting is most often used. Of course, it is permissible only if there is no suspicion of the formation of malignant cysts.
If there is no dynamics of reduction in the size of the cyst, the doctor may prescribe medications for a course of conservative therapy or prescribe surgery to remove the ovarian cyst.
Symptoms of polycystic ovary syndrome. The tip of the iceberg
Are you worried about very irregular menstruation that periodically disappears completely? Or maybe you already consider this your norm? This is not the norm, but a symptom of many serious diseases. And one of them is polycystic ovary syndrome.
“Polycystic ovary syndrome” sounds very scary. The imagination pictures many huge cysts growing on the ovaries and monstrous suffering. “Wow, so young, and already with polycystic disease,” those around her shake their heads sympathetically.
In fact, everything is completely different. With PCOS, cysts do not form at all, as you might think, but only immature follicles accumulate due to disruption of their normal maturation. These follicles are located along the periphery in the form of a “pearl necklace” - a typical ultrasound sign of the syndrome. PCOS, according to most researchers, is a hereditary disease that occurs shortly after the onset of menstruation. Therefore, it is not surprising that most patients diagnosed with this syndrome are quite young.
However, the main clinical signs can seriously worry women - periods are irregular, the skin is oily with acne, hair grows in a male pattern (from a thin dark stripe on the stomach to a well-defined mustache and beard), not everyone gets pregnant right away. However, this is only the visible part of the iceberg; the syndrome has quite large-scale hidden manifestations and associated risks.
Background*
In 1935, American gynecologists Irving Stein and Michael Leventhal clearly identified a syndrome in which amenorrhea is combined with multiple small cysts in both ovaries. For several decades this condition was called Stein-Leventhal syndrome.
However, until the end of the twentieth century, the diagnosis of PCOS was a “garbage dump”, which included all patients with menstrual irregularities without specific causes. This situation persisted until 2003, when leading European experts gathered in Rotterdam and formulated rules for establishing this diagnosis.
It was decided to diagnose PCOS if any two of the following criteria were present:
- Menstrual dysfunction with anovulation: rare menstruation, absence of menstruation for a long time, constant scanty bleeding, absence of pregnancy for a long time Note: This criterion is not applicable for teenage girls and premenopausal women, since the formation and decline of menstrual function, even normally, is not uncommon accompanied by irregular menstruation and lack of ovulation.
- Clinical and/or biochemical signs of excessive secretion or activity of androgens - “male” sex hormones (increased body hair growth according to the male type, increased oily skin, acne on the face, back, acanthosis nigricans - dark areas of skin in the perineal area, inguinal folds and axillary region).
- The presence of polycystic ovaries according to ultrasound examination - at least 12 follicles with a diameter of 2–9 mm in one ovary and/or an increase in the volume of at least one ovary (more than 10 mm³) in the absence of a dominant follicle with a diameter (more than 10 mm³).
But if disorders with PCOS were limited only to cycle disorders and hairiness, it would not be so scary.
Back in 1921, French doctors Emile Achard and Joseph Thiers described metabolic disorders in polycystic ovary syndrome as “diabetes of bearded women.” Indeed, in addition to other symptoms, PCOS is also characterized by impaired fat and carbohydrate metabolism with the development of obesity and type 2 diabetes.
And, unfortunately, this is not all. Women with PCOS have a significantly increased risk of developing atherosclerosis, vascular complications (strokes and heart attacks), venous thromboembolism, depressive disorders, including full-blown psychiatric symptoms, as well as endometrial cancer.
What does it look like?
If PCOS is suspected, the doctor follows a certain diagnostic algorithm and discards the “wrong” ones.
1. It is very easy to work with patients who have a menstrual calendar. So, if a woman has had less than 10 menstruation in a year, we can talk about oligomenorrhea. If there has been no menstruation for more than 3 months - secondary amenorrhea.
If menstruation is regular, but pregnancy does not occur after 12 cycles, it is assumed that there is no ovulation. When it comes to infertility, the optimal diagnostic method is ultrasound folliculometry - monitoring the life of follicles using ultrasound. If no signs of ovulation have occurred in two cycles in a row, then their absence is considered proven. Looking ahead, I will say that such patients still ovulate 1-2 times a year, so spontaneous pregnancies are possible and even not uncommon.
2. The activity of “male” sex hormones is usually visible to the naked eye and is assessed using the Ferriman-Gallway scale. Only dense guard hairs can be counted; fluff can be neglected.
In representatives of the Caucasian race, a score of 8 or more allows us to talk about hirsut syndrome. It is widely known that acne is also associated with “male” hormones, but hirsutism is important for diagnosing the syndrome.
If there is no “male” hair growth, you will have to take “male” hormones. There are certain difficulties here, since precise determination methods do not yet exist, and large studies have not been carried out to clarify the boundaries of the norm. Therefore, the results of these analyzes and their interpretation should be treated with a great deal of skepticism.
It is important to understand that, according to the updated recommendations of the Endocrine Society, the “building block” for the diagnosis of PCOS is considered to be both clinical manifestations of excessive activity of “male” hormones (even if their level in the blood is normal) and their increased content in the blood serum (without acne, hairiness and acanthosis nigricans). Therefore, tests for testosterone are more often done in patients without clinical manifestations of hirsutism, or with very severe symptoms, to exclude the tumor nature of the disease.
What can be confused with
To definitively verify the diagnosis, the doctor must exclude other conditions that are characterized by the same symptoms: hirsutism, oligogmenorrhea/anovulation and polycystic ovaries.
There are many such conditions: alimentary obesity, hyperprolactinemia, pathology of the thyroid gland, congenital adrenal hyperplasia (CAH), Itsenko-Cushing disease or syndrome, hormone-producing tumors of the ovaries or adrenal glands, family characteristics of hair growth, acromegaly, premature ovarian failure, taking drugs that cause androgenization ( anabolic steroids, androgens, valproic acid).
It sounds quite impressive, but in reality everything is not so complicated. Some diseases have characteristic features that are visible to the doctor literally “from the door.” Nevertheless, among the mandatory tests it is worth noting TSH (to exclude thyroid pathology) and prolactin (to exclude hyperprolactinemia). And taking 17-OH-progesterone on days 2–4 of the cycle is the easiest way to rule out CAH (congenital adrenal hyperplasia).
With severe hirsutism, which rapidly progresses, hormone-producing tumors of the ovaries and adrenal glands can be suspected. Tumors can be small in size; ultrasound does not always find such formations. In order not to send everyone for an MRI, the doctor can look at the level of testosterone and DHA-S. If the level increases by 3–5 times, a tumor must be excluded.
When patients with the classic picture of PCOS additionally experience severe obesity, type 2 diabetes mellitus, purple stretch marks appear on the skin, and blood pressure rises, the doctor has to rule out Cushing’s disease.
But determining the level of cortisol in the blood, which is so popular in our country, is completely meaningless here.
Underwater part of the iceberg
The wishes of the patients are simple and understandable: they want hair to not grow where it shouldn’t, for menstruation to come regularly and predictably, and for pregnancy to occur on demand at the desired time.
The doctor's tasks are much more difficult, because only the doctor knows what is hiding in the underwater part of the iceberg, the tip of which is so accessible to study. I will tell you more about approaches to treating polycystic ovary syndrome, as well as how to get pregnant with such a diagnosis, in my next article.
Oksana Bogdashevskaya
Photo: main thing - thinkstockphotos.com, in the text - provided by the author
PCOS: a new look at the problem. Variety of symptoms, differential diagnosis and treatment of PCOS. Newsletter / I.G. Shestakova, T.S. Ryabinkina; edited by V.E. Radzinsky. - M.: Editorial office of the magazine StatusPraesens, 2015. - 24 p.
Treatment of ovarian cyst
Considering that many ovarian cysts go away on their own, to treat them it is usually enough to normalize the patient’s hormonal levels. To eliminate cysts, the attending physician, based on tests and ultrasound, prescribes certain hormonal drugs or contraceptives, anti-inflammatory, antibacterial therapy, physiotherapy, enzymatic drugs, which over the course of several menstrual cycles lead to the resorption of cysts. If resorption of the ovarian cyst is not observed, surgery is prescribed.

Ovarian cyst
Even the most harmless neoplasm requires constant monitoring and therapy to avoid complications.
In an urgent situation, the attending physician decides on the type of operation: laparotomy (open) or laparoscopy (endoscopic), since an inspection of the organs and an early stop of bleeding is required.
Expert opinion
When removing a cyst in young women, operations are performed aimed at maximizing the preservation of reproductive function. If we are talking about borderline formations that are prone to malignancy, mature or elderly patients can undergo removal of the ovary.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
Elective surgery is most often performed laparoscopically in the absence of other contraindications. The advantage of this operation is less trauma to the anterior abdominal wall, cosmetic effect, and a short recovery period after surgery.
In order for the operation to remove an ovarian cyst to be as successful as possible, you need to properly prepare for it. To do this, it is necessary to pass preliminary blood and urine tests, biochemical blood tests, tests for the absence of AIDS, syphilis (Syphilis), hepatitis B (Hepatitis B) and C (Hepatitis C), coagulogram, ECG and ultrasound of the pelvic and abdominal organs, fibrogastroduadenoscopy , colonoscopy. Immediately before surgery, bowel preparation is performed.
The extent of the operation is determined by the type, location and diameter of the formation. It may come down to enucleation of the cyst, resection (excision) of part of the ovary, or removal of the ovary completely.
The rehabilitation period after surgery usually takes from 10 days to a month. During this time, you need to abstain from sexual intercourse, physical activity, and sports. It is better to adhere to the diet developed by your doctor and exclude some spicy and particularly allergenic foods from your diet. At the end of this period, the woman can return to a full life.
In addition to laparoscopy, it is possible to prescribe abdominal surgery to remove an ovarian cyst with opening of the abdominal cavity. Usually, such a radical method is resorted to only in case of suspicion of a malignant nature of the ovarian cyst, when the size of the formation is larger than average, ruptures and torsion.
Considering that the development of ovarian cysts is often accompanied by various hormonal disorders, evening primrose oil can be used as an aid to normalize hormonal levels to reduce the negative consequences. The product was developed by specialists from a pharmaceutical company and has the necessary package of documents and quality certificates.
Ovarian cyst during menopause
Ovarian cysts during menopause are a common phenomenon that affects every fifth patient at this age. Treatment tactics, if the diagnosis is confirmed, is determined not only by age, but also by the size of the tumor, its location, the nature of the pathological process, and the presence of associated complications. A gynecologist will be able to decide on a treatment plan and select the most effective regimen, based on the results of a comprehensive diagnosis. If the cyst is stable in size and does not cause any pathological symptoms, treatment is not prescribed. In case of tumor enlargement, complex drug therapy is selected. If medications are ineffective and the cyst continues to grow, the doctor decides to surgically remove it.
Traditional treatment - how to treat ovarian cysts with herbs?

Many women who find out that they have a cyst ask a logical question: how to treat an ovarian cyst without surgery and is it possible? Yes, indeed, in some cases you can do without surgery. However, in no case should you decide on your own whether you need surgery or whether you can limit yourself to other methods. This decision can only be made by your attending physician.
Despite the fact that traditional drug therapy is the most effective today, traditional medicine also includes effective methods for treating ovarian cysts. We are talking about herbal medicine - the treatment of cysts with herbs. However, herbal preparations act on the cyst much more slowly than pharmaceutical drugs, so it takes longer to treat a disease such as an ovarian cyst. Usually the first positive changes in the condition of the cyst occur after a couple of months.
Remember that some herbs have contraindications and can also cause allergic reactions. Therefore, when choosing a remedy for the treatment of ovarian cysts using traditional methods, you need to take into account the characteristics of your own immune system. If inflammation and pain occur with an ovarian cyst, herbal treatment should be stopped.
About the disease
The need for treatment of endocervicosis can only be realized by understanding the course of the disease. The pathology is a replacement of the cylindrical epithelium on the cervix. Changes occur on the part of the cervix that enters the vagina. During the disease, the mucous membrane is replaced by the epithelium of the cervical canal, which is not adapted to function under these conditions. It does not withstand the natural environment of the vagina well and is not intended for mechanical impact. Constant trauma to the epithelium significantly increases the risk of oncogenic neoplasms. That is why pathology requires the prompt intervention of a specialist.
Ovarian cyst is not a reason to despair
If you notice symptoms of a cyst, make an appointment with your doctor.
Usually, a cyst can be easily dealt with: the main thing is not to delay the start of treatment and follow the doctor’s instructions. Sources:
- FEATURES OF THERAPY OF OVARIAN ENDOMETRIOID CYSTS. Sidorova I.S., Unanyan A.L. // Obstetrics, gynecology and reproduction. – 2011. – No. 1. – pp. 29-31.
- ISSUES IN THE MANAGEMENT OF PATIENTS WITH OVARIAL LOCATIONS. Khairutdinova M.R., Egamberdieva L.D. // Practical medicine. – 2015. – No. 4 (89). – pp. 191-196.
- Clinical expression of leptin and interleukin-6 in ovarian endometriosis. Davydov A.I., Strizhakov M.A., Orlov O.N. // Issues of obstetrics, gynecology and perinatology. - 2004. - vol. 4, no. 2, pp. 40-46.
- Once again about the terminology of endometrioid formations of the ovary. Savelyeva G.M., Solomatina A.A., Mikhaleva L.M., Pashkova A.V., Vorobyova N.N. // Obstetrics and gynecology. — No. 6. - 2005. - P. 33.
- Clinic, diagnosis and treatment of endometriosis (textbook). Peresada O.A. // Minsk. - 2001.- P. 274.
- https://research.omicsgroup.org/index.php/Ovarian_cyst
- https://www.medicalnewstoday.com/articles/322476.php
- https://emedicine.medscape.com/article/255865-overview
- https://rarediseases.info.nih.gov/diseases/3934/1
Popular questions
I have inflammation of my left ovary.
The doctor prescribed me several injections and suppositories. Can I replace injections with tablets? I recommend that you consult your doctor regarding this issue to select adequate therapy and change the method of administration.
How to treat an ovarian luteal cyst if I’m pregnant, what should I do?
During pregnancy up to 16 weeks, such cysts require only dynamic monitoring and ultrasound control once a month.
I have a cyst, but I want to get pregnant, please help me.
Hello! Before planning a pregnancy, you need to understand the nature (genesis) of the ovarian cyst and how much it will affect conception and pregnancy. Therefore, you should immediately consult a specialist.
I suspect inflammation and cysts. The doctor prescribed IV thiosulfate, IM ceftriaxone, and Diclovit suppositories. I just didn’t explain, do you need to apply everything at the same time or what?
Hello!
Most often, this complex of treatment is carried out simultaneously, but it is better to check with your doctor. For an accurate diagnosis, contact a specialist
General ideas about pathology
Every month, a woman’s body goes through a certain hormonal cycle, preparing it for the possible conception and bearing of a child. From the first days of a new cycle, a woman’s body actively produces a hormone that stimulates the development of the egg. In the cavity of each of the two ovaries there are many follicles ready to respond to its influence. But in the end, only one or two will ripen and form a graphite bubble.
Correct and timely production of LH contributes to the opening of the most developed follicle. Under its influence, a mature egg is released into the tubes, ready for fertilization. If for some reason the opening does not occur, a pathology is formed.
An ovarian follicular cyst in women is a small, benign neoplasm localized in the ovary. It is rare in size - it exceeds 7-10 centimeters. The main feature of the neoplasm is that it has virtually no tendency to become malignant.
The structure of the body is one-chamber or two-chamber; there is an accumulation of fluid inside it. A single-chamber cyst looks like a round cavity and occurs in 90% of cases. Two-chamber consists of two neoplasms combined into one. Its development is possible with the simultaneous maturation of several eggs. When performing an analysis, you can see that the liquid inside the bladder is oversaturated with estrogens.
Pathology is rarely diagnosed, because it tends to reverse transformation and disappear. Cysts occur with different frequencies in different ovaries. In the left tumor appears rarely. This is due to the fact that the gland is supplied with blood primarily through the renal artery. Due to the long passage of blood from the heart on the left, the bubbles mature less frequently. But nevertheless, the appearance of a cyst in the left ovary is possible. The reasons for its development lie primarily in hormonal disorders. But only a doctor can determine exactly why the bubble did not open.
The right side has a different nutrition system, as it is inextricably linked with the aorta. Good blood supply leads to the fact that the follicles on the right ripen more often. In the course of studying this phenomenon, experts also discovered that the cysts localized on this side are larger in size than the tumors on the left.