Take the first step
and make an appointment with your doctor!
The first image of a baby on an ultrasound is one of the most joyful moments of a woman who wants to become a mother. However, in some cases, the expectant mother, already confident in her pregnancy after passing the test, during a routine examination hears from the doctor that the embryo is not visible on ultrasound imaging. This anomaly (anembryonia) is quite common in obstetric practice. What are its causes, how does it threaten a woman and can it be avoided? To answer this question, you need to understand the mechanism of pregnancy development in the early stages.
Why is the embryo not visible on ultrasound?
It is impossible to examine even a normally developing fetus immediately after conception - it is too small for an ultrasound scanner to distinguish it from the background of surrounding tissues and organs. Therefore, the first ultrasound to confirm pregnancy is usually done 6-7 weeks after conception. Until this point, the fact that a woman will be a mother can only be judged by the level of human chorionic gonadotropin, which begins to be secreted by the chorion (fetal membrane of the embryo) 6-7 days after conception. Normally, with the successful development of pregnancy, the concentration of hCG in the body increases along with the development of the fetus.
To understand the mechanism of anembryony, it is necessary to understand the structure of the embryo itself and its early development. It happens in several stages:
- A zygote is essentially a fertilized egg formed at the moment of conception;
- Morula is the next stage, characterized by the division of the zygote into several cells of the same type;
- Blastula is an embryo in which the cells are already divided into an inner cell mass (embryoblast) and an outer layer (trophoblast);
It is at the blastula stage that the future body of the embryo and the protective membranes surrounding it are formed. When the embryo leaves the fallopian tube and descends into the uterine cavity, enzymes secreted by the outer cells partially dissolve the endometrium, and its implantation occurs. Next, the embryo and amniotic membranes develop in parallel, gradually forming a mature fetus and placenta.
With anembryonia, this process is disrupted - the outer membrane (fertilized egg) continues to grow, releasing hCG, while the embryo either does not form at all or its development stops at an early stage. Because of this, for some time the tests give false results, showing a normal pregnancy. Only after some time the chorion stops secreting hCG, the level of which gradually begins to decrease.
The reasons for embryonic growth arrest, leading to an empty fertilized sac, are not fully understood. Today these include:
- Genetic abnormalities. In most cases, anembryony is caused by pathological chromosomal mutations, either originally characteristic of the parents, or appearing as a result of unsuccessful recombination of genes in their body. Genetic disorders in the embryo itself are also possible, occurring in the early stages of its development.
- Infections. Among them, the most dangerous for embryogenesis are the diseases included in the TORCH complex - rubella, herpes, cytomegalovirus, toxoplasmosis, syphilis, hepatitis B and C, etc. Infectious pathogens can affect the maternal body, disrupting its reproductive function (for example, causing chronic endometritis) , or the embryo itself, leading to disruptions in its development.
- External factors. This primarily applies to ionizing radiation (radiation) and toxic chemicals (poisons, some medications). They cause functional disorders of the mother's reproductive system or genetic mutations in the embryo, stopping its normal development.
- Endocrine disorders. Disorders of a woman's endocrine glands can also lead to anembryonia. The appearance of a fertilized egg without an embryo is especially likely if there is a deficiency or disturbance in the metabolism of progesterone, a sex hormone that plays an important role in the decidualization (morphological change) of the endometrium at the point of implantation of the embryo.
- Immune disorders. Quite often, the cause of improper development of the embryo is damage to it by the protective system of the mother's body. This can happen indirectly - for example, when the embryo gets caught in the “crossfire” of immune cells attacking the infection. Sometimes the embryo itself is regarded by the woman’s immune system as a foreign object, because its genetic code is half composed of the genome of another person (the father).
Anembryonia can be caused by either one of these factors or their complex effects. It is impossible to predict the development of this pathology - it is observed even in absolutely healthy women who have already had experience of successful pregnancy.
This anomaly should be separated from a frozen pregnancy. With anembryony, the embryo does not form at all, and in the second case, its development stops at an early stage. Moreover, in terms of external manifestations and ultrasound, these pathologies may look the same.
Take the first step
make an appointment with a doctor!
Symptoms of anembryonia
The arrest of embryonic growth itself does not have its own specific signs. In the early stages of such an abnormal pregnancy, the woman’s condition corresponds to the medical norm. Moreover, a growing level of hCG in blood tests shows that conception was successful and the embryo is developing normally. The first symptom of the disorder is precisely the stopping of this growth and a decrease in the concentration of human chorionic gonadotropin in the body. The pathological process is reflected in the mother’s body at the moment when the decomposition of the embryo begins. The breakdown of its tissues is accompanied by characteristic signs of septic poisoning:
- increased body temperature;
- nausea and vomiting;
- muscle pain and constant weakness;
- pain in the lower abdomen;
- uterine bleeding or discharge mixed with blood.
Sometimes the decomposition of the embryo is asymptomatic or with signs of mild malaise. In this case, the empty amniotic membranes themselves are torn away from the endometrium and come out naturally. However, in most cases it remains in the mother’s body and causes serious consequences that threaten the health and even life of the woman.
Diagnosis of anembryonia
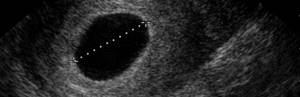
The main way to detect this pathology is ultrasound examination. It is with its help that the presence of an embryo in the fertilized egg and its normal development can be established. In a normal pregnancy, the embryo is not visible on average until 6-7 weeks after conception, so at this stage, indirect signs of pathology can be a drop in the level of hCG in the blood or a deficiency of progesterone.
To make a diagnosis of anembryonia, the following conditions must be met:
- absence of a yolk sac in a fertilized egg with a diameter of 8-25 mm;
- absence of an embryo in a fertilized egg larger than 25 mm.
There are also additional signs of anembryonia, in particular deformation of the ovum, an abnormally low increase in its size, mild decidualization of the endometrium at the point of implantation, and unregistered heartbeat at 6-7 weeks of pregnancy. Such a diagnosis may also be supported by signs of fetal rejection - changes in uterine tone, the appearance of areas of chorionic detachment with the formation of subchorionic hematomas.
Depending on the clinical picture of the pathology revealed during ultrasound examination, 3 types of pathology are distinguished:
- Anembryonia type I - the embryo is not detected on imaging, the size of the fertilized egg is usually no more than 2.5 mm, and the uterus is enlarged only until 5-7 weeks of pregnancy;
- Anembryonia type II - there is no embryo, but the size of the fertilized egg and uterus corresponds to the gestational age.
Separately, it is worth highlighting the resorption of embryos during multiple pregnancies. Most often, this condition occurs after in vitro fertilization, when several embryos are implanted into the patient at once to increase the chances of successful conception. Usually only one of them takes root, but in rare cases 2 or more embryos are successfully implanted. In this case, some of them freeze in their development, after which they resolve or are removed from the body naturally.
Take the first step
make an appointment with a doctor!
Timing of the examination
The first ultrasound is prescribed when a woman comes to the antenatal clinic to register. Usually this is a period of 10-12 weeks, if there is a positive hCG test. Then it is already possible to detect the fertilized egg along with the embryo in the uterus and identify developmental pathologies. An ultrasound can be done earlier; it will detect the embryo 14-20 days after the missed period.
The second scheduled examination is done at 20-22 weeks. Here you can identify fetal malformations. The last examination is carried out 14-21 days before birth to determine the position of the fetus and the woman’s readiness for childbirth.
Unscheduled studies are prescribed for women with suspected or existing pathologies of fetal development. An ultrasound is prescribed after IVF to determine whether the embryos have implanted. After embryo transfer, examination is carried out 21 days later.
The embryo is hard to see on an ultrasound: should I worry?
The mere absence of an embryo on ultrasound imaging does not mean anembryonia, even if the study was performed at 6 weeks or later. The equipment may not detect the embryo for the following reasons:
- Imperfection of ultrasound. Ultrasound diagnostics has long been firmly established in medical practice, but this method has its limitations. The resolution of some devices (even modern ones) is too low to detect a fetus, which in the early stages of pregnancy is only a few millimeters in size. Therefore, to clarify the diagnosis, a repeat examination is carried out after 6-8 days, which will confirm or refute the initial result.
- Excess weight. During ultrasound, an image of the organs being examined is formed using reflected high-frequency signals passing through the tissue. Some of the sound waves are absorbed, which distorts the data. Since during abdominal ultrasound the sensor is located on the surface of the patient’s abdomen, if she has a thick sound layer, the weakened signal may simply not detect the embryo. To increase the accuracy of this method, a transvaginal examination is used, in which a sensor is inserted into the patient's vagina - this reduces distortions caused by the tissues surrounding the embryo.
- Too early. Often, during natural conception, a woman cannot determine exactly when it occurred. In such cases, routine ultrasound can be performed earlier than the time when the embryo reaches a size sufficient for its visualization. To accurately determine the presence or absence of an embryo in the fertilized egg, you need to undergo the examination again using more sensitive equipment.
If, when diagnosing pregnancy, ultrasound “does not see” the embryo, doctors combine it with other examination methods - in particular:
- Dopplerography is a type of ultrasound that records dynamic processes in the body of the mother and fetus (for example, blood flow, fetal heartbeat);
- With cardiotocography - the essence of this method is to record electrical impulses accompanying the heart contractions of the embryo.
In addition to these methods, a gynecological examination, blood tests for progesterone or hCG are also used. In general, at 6-8 weeks of pregnancy, doctors can already confidently state the normal or abnormal development of the embryo.
Take the first step
make an appointment with a doctor!
How to prepare for the procedure
The quality of ultrasound results at 4 weeks of pregnancy directly depends on the quality of preparation for the study. So, if a transvaginal ultrasound is prescribed, then the woman should only empty her bladder immediately before the procedure.
Transabdominal ultrasound is performed on an empty stomach and with a full bladder. To do this, in the morning before the procedure, the woman should not eat anything, and an hour before the ultrasound, drink 1 - 1.5 liters of non-carbonated and non-dairy liquid. When the urge to urinate occurs, you can conduct an examination. Some clinics recommend bringing a towel or diaper to cover the couch, and napkins to wipe off the gel from the skin of the abdomen.
The embryo is not visible in the egg: what to do?
Accurately diagnosed anembryonia is an indication for artificial termination of pregnancy. Sometimes the fertilized egg can leave a woman’s body on its own, but this does not always happen. As it decomposes, it can cause serious damage to the patient’s body. Therefore, doctors recommend not to wait for the problem to resolve itself.
Currently, three methods of artificial termination of pregnancy in anembryonics are used:
- Medical abortion. This method is used no later than 6-8 weeks of pregnancy. It consists of the patient taking mifepristone and misoprostol, drugs that block progesterone receptors in the endometrium and cause uterine contractions to expel the fertilized egg. Medical abortion is considered the most effective and safe method of terminating pregnancy, which does not damage the uterine lining and generally occurs without serious consequences for the female body. However, it is applicable only in the early stages, when the embryo is not yet securely attached to the uterine mucosa. After 8 weeks, this method can lead to incomplete expulsion of the fertilized egg and cause complications.
- Vacuum aspiration. This method is used for periods up to 12 weeks (according to WHO recommendations) or up to 5 weeks (in Russia) of pregnancy. It is based on sucking out the fertilized egg using a vacuum pump, the catheter of which is inserted into the uterine cavity and creates negative pressure in it. The advantage of this method is its safety and minimal damage to the uterine mucosa. However, when using it, the risk of incomplete abortion remains, so additional ultrasound is required after the procedure.
- Scraping (abrasion). This is the traditional and most traumatic method of artificial termination of pregnancy. It consists of mechanical scraping out the fertilized egg and part of the uterine mucosa using a special gynecological instrument (curette). Abrasion is performed at 6-12 weeks of pregnancy, while the woman needs more time to restore the endometrium. Due to the nature of this procedure, complications such as incomplete abortion, uterine perforation, cervical rupture, bleeding, infection, etc. may occur after it.
If an embryo is not visible at 6 weeks of pregnancy, this does not mean a death sentence for a woman as a mother. According to statistics, every 8 conception ends in anembryonics, so this pathology is much more common than infertility. With correct and timely diagnosis and artificial termination of an abnormal pregnancy, reproductive function is restored by the next menstrual cycle, although doctors still recommend taking a break between attempts. This anomaly is rare again, and the woman has every chance of becoming a happy mother in the future.
What happens to the fetus in the fifth week?
During the first four weeks of pregnancy, the fetus developed at an incredible rate. In the fifth week, his heart begins to beat, his cardiovascular and nervous systems develop. The formation of the spine and spinal cord also occurs, and the fetal brain now consists of two lobes.
By the fifth week, the fruit becomes pear-shaped and reaches approximately 4 mm in length. Such dimensions can already be visualized by ultrasound scanning.
The rounded part of the embryo will in the future transform into the baby’s head, and the sharp part into the spine.
Also in the fifth week, the formation of the internal organs of the fetus occurs: liver, pancreas, larynx, trachea.











