Mediastinal biopsy - what is it?
The mediastinum is a complex of organs surrounded by fatty tissue, which are located between the cavities of the pleura, right and left. It is limited in front by the sternum and behind by the spine. The upper boundary is the upper aperture of the chest, the lower is the diaphragm.
In some cases, it is necessary to perform a biopsy of the mediastinum.
A mediastinal biopsy is understood as a diagnostic procedure, during which a biopsy sample (biological material) of tissues altered by pathology is removed for further study in the laboratory.
This procedure is indicated when the spread of atypical cells to the lymph nodes is suspected, which happens when enlarged lymph nodes are detected in cancer of the lung or other organs.
Who is at risk?
Mediastinal tumors are quite rare. They can develop at any age and from any organs and tissues that are located in the mediastinum, but in most cases they are diagnosed in patients between 30 and 50 years of age. Tumors of the posterior mediastinum are more common in childhood. They usually originate from nerve tissue and, in most cases, are not cancerous. In the adult population, tumors of the anterior mediastinum predominate - lymphomas and thymomas are usually located there.
Mediastinum in X-ray image
Transcript of a video lecture by Professor Igor Evgenievich Tyurin on the mediastinum in an X-ray image from the series of programs Radiation diagnostics for therapists.
Igor Evgenievich Tyurin, Doctor of Medical Sciences, Professor:
- Good afternoon! Good day, dear colleagues and those who listen to us!
We are pleased to begin today a new project, which is announced as: “Radiation diagnostics for therapists.” For attending physicians, I would call this topic this way.
Today in the studio, Candidate of Medical Sciences Irina Aleksandrovna Sokolina. Head of the Department of Radiation Diagnostics, Clinic of Propaedeutics named after Vasilenko, Perm State Medical University.
My name is Igor Evgenievich Tyurin. I head the Department of Radiation Diagnostics at the Russian Academy of Postgraduate Education.
Today is our first seminar, the first lesson on radiation diagnostics. It will be devoted to diseases of the thoracic cavity organs, pathologies of the thoracic cavity organs.
We discussed for a long time in what format and in what form to start this seminar, what could be taken up as the first topic for discussion. We decided that a combination of issues of normal anatomy, issues of interpretation of X-ray images with fairly common pathology is the best option for initial studies.
Today we are talking about the pathology of the mediastinum. Moreover, we will talk about this both from the point of view of x-ray anatomy and from the point of view of the pathology of the lymphatic system of the chest cavity. In conclusion, here is a short review of mediastinal neoplasms, since this is one of the most common pathologies in this area.
We will start in the following order. First, I will talk very briefly about the normal x-ray anatomy of the mediastinum and the general principles of interpreting x-ray images. This is important for all doctors - not only radiologists, but also doctors of all specialties. We encounter chest x-rays probably every day.
Next, Irina Aleksandrovna will talk about the pathology of the lymph nodes and the condition of the roots of the lungs during an X-ray examination.
As I already said, the third (final) lecture will be devoted to mediastinal neoplasms.
Let's start. In this case, I will start: with issues of normal anatomy and principles of interpretation of mediastinal pathologies.
02:47
(Slide show).
Naturally, we begin with what we can do and how we can examine the mediastinum.
It is clear that the initial examination in the vast majority of cases is an x-ray examination. Minimum volume: anterior direct projection and right lateral projection. If necessary, additional images are taken, although this is now quite rare. But in some cases you still have to do this.
(Slide show).
However, the main way to obtain primary information is, of course, two standard x-rays. In these pictures we see an image of the mediastinal shadow (or middle shadow). On the sides of the middle shadow is an image of the roots of the lungs. This, in fact, is the subject of our discussion today.
(Slide show).
How can radiologists and attending physicians interpret the condition of the mediastinum and identify pathological changes there?
Two main points. The contours of the middle shadow, which are formed by the vascular structures and chambers of the heart, first of all. Secondly, this is the structure of the median shadow, which makes it possible to identify pathological changes in this anatomical region.
It is clear that the bulk of the middle shadow consists of the heart and large vessels. In front is the chest wall. Behind – the spine, posterior segments of the ribs, soft tissues. This is all summarized on a survey radiograph. But still, the bulk is, of course, an image of the chambers of the heart.
The heart is located symmetrically in the chest cavity, as you well know. It makes up the lower, widest part of the middle shadow. Above are large vessels that originate from the chambers of the heart or bring blood to the chambers of the heart.
(Slide show).
If we talk about how the contours of the mediastinum are formed (the contours of the middle shadow), then radiologists usually call them arches - according to the tradition formed in the middle of the last century in our classic manuals. These bulges or contours of the middle shadow are formed by various vessels and chambers of the heart.
If you move from right to bottom and further to the left (also from top to bottom), then the uppermost part of the middle shadow on the right is formed by the superior vena cava. A slightly intense shadow running parallel to the thoracic spine. Next is the right atrium. Between them is the right atriovasal angle, which normally is, as you can see, one third of the height of the chest on an x-ray.
At the very bottom, sometimes on plain radiographs we see a low-intensity contour of the inferior vena cava, which flows into the right atrium.
05:42
If we talk about the left circuit, then this is the left subclavian artery coming from the aorta. Below, in fact, is the aortic arch. Even lower is the pulmonary artery. The contours of these two vessels create a characteristic, typical crossover on plain radiographs (well visible normally).
Below these two lines you can clearly see a light gray, fairly clearly defined air strip in the lumen of the left main bronchus, which here separates the vessels from the chambers of the heart.
Below is the left atrium (below the left main bronchus).
Finally, the left ventricle, which goes behind the shadow of the diaphragm.
(Slide show).
This is how the contours of the mediastinal shadow (middle shadow) are normally formed. If you depict this on a diagram... We deliberately left this as a slide so that it remains and can later be studied and viewed in a calm atmosphere. All the so-called arcs or contours of the heart shadow or middle shadow are depicted here. They form a normal x-ray picture.
(Slide show).
But besides this, there is also the so-called middle shadow structure. This is due to the fact that the heart and large vessels that form shading in the center of the chest cavity are not an ideal round cylinder, but a rather complex structure in the axial plane. It borders on air-containing lung tissue. Where this or that anatomical structure comes into contact with the air filling the lung tissue, we see the outline of this structure.
The contour of the descending aorta, for example, is clearly visible here. Or the outline of the thoracic vertebrae.
Why?
The adjacent lung tissue is airy. Thus, since air is a natural contrast agent, it creates a peculiar structure of the middle shadow.
Naturally, in the center (at the top) you see the air strip of the trachea and the two main bronchi, which cross the upper part of the middle shadow from top to bottom.
We will now look more specifically at those anatomical structures that may be of interest when we talk about pathology - the border between normal and pathological.
08:10
(Slide show).
What are these lines?
These could be lines, they could be contours, they could be stripes. They will be formed depending on what exactly borders, as I already said, the air-containing lung tissue.
This may be the connection of the mediastinal pleura. These can be the contours of the descending aorta, paravertebral lines, and the contours of the azygos vein. All this can be shown now on separate slides so that it is clear.
(Slide show).
The simplest example. One of the typical components of the mediastinal structure is, of course, the right paratracheal strip. It crosses the mediastinum from top to bottom (this is shown by arrows).
Why does it occur?
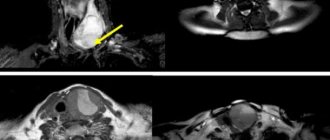
Inside the trachea there is air as a natural contrast agent. In the upper part you see the computed tomography reformation in the frontal plane. The main bronchi of the trachea are filled with air. From the outside, if you look at the axial sections, the right wall of the trachea is always normally adjacent to the air-containing lung tissue, which is located in the upper lobe of the right lung.
While the lung tissue remains airy and is located next to the trachea, we see the wall of this trachea in its natural form - in the form of a strip, which is located from top to bottom in the right half of the mediastinum.
Further – above the right main bronchus – is a cross-section of the azygos vein. Next begins the root of the right lung, which will be discussed later.
09:43
Another example from the same area.
Why is this fundamentally important?
(Slide show).
Where pathological changes occur, the normal anatomical structure is altered. On the right on the slide is a patient who has an enlargement of the paratracheal group of lymph nodes. This is shown by an arrow on the axial section.
You can clearly see: expansion of the mediastinum to the right naturally leads to the disappearance and replacement of the right paratracheal strip due to the fact that in this place it is no longer air that is adjacent to the mediastinum, to the right wall of the trachea, but enlarged lymph nodes.
(Slide show).
Another anatomical structure is the so-called line or stripe of the anterior mediastinal joint. On axial sections, the arrow shows how the mediastinal pleura anterior to the aortic arch is connected into one whole structure and is located perpendicular to the sternum and the anterior chest wall.
The display of this structure on x-ray films is a typical perfect line that crosses obliquely the region of the tracheal bifurcation. If it is present, we can almost certainly say that there are no pathological formations in the mediastinum or any changes in this area.
On the other hand, in addition to such stripes or lines that exist in the mediastinum, there are also contours of natural anatomical structures. The most understandable and simplest in this regard are the contours of the arch of the descending aorta (here they are shown with red arrows - you see them on axial tomograms).
Since the arch in its distal part and the descending aorta along its entire length border with air-containing pulmonary tissue, mainly in the lower lobe of the left lung, we always clearly see the left contour of the descending aorta against the background of the vascular structures of the mediastinum, against the background of the heart.
11:40
On the other hand, we can always see the contours of the thoracic vertebrae (the so-called paravertebral lines) next to the contour of the descending aorta. Here they are indicated by pink arrows. Since the thoracic vertebrae are also in contact with the air-containing lung tissue, they are also normally visible on x-rays very well.
On the other hand, a long, fairly intense vertical line that crosses the spinal column almost in the middle is a line that is formed by the retraction of the cardiac silhouette behind the heart. Where the azygos vein is located. The esophagus is located somewhere there. Hence the name - (inaudible, 12:27) - esophageal pouch.
The pulmonary tissue here extends beyond the right atrium deep into the mediastinum and forms a kind of inversion. We can clearly see this on a survey X-ray in the form of a stripe. Many people, by inertia, perceive this as the right wall of the aorta, hoping to see an aortic aneurysm or some other pathological changes in this place.
But if you look at the axial sections, you can clearly see that the left wall of the descending aorta borders the pulmonary tissue, and the right wall of the aorta is located in the thickness of the mediastinum, bordering the fatty tissue. Therefore, of course, we cannot see it in any way on a survey x-ray.
On the left, along the right contour of the middle shadow, you see the contours of the thoracic vertebrae. They are indicated by the same pink arrows. The vertebral bodies on the right border in the same way with the lung tissue.
(Slide show).
What practical significance does this have?
Here is a young man whose mediastinal configuration is almost normal, we would say. There is nothing special here, perhaps in terms of the width of the middle shadow or the image of the arcs of the middle shadow. However, we see a clear, perfectly defined double outline to the right above the aperture. It's like there are two chambers of the heart.
Where did this circuit come from?
Obviously, there are some additional formations here, in addition to the normal vascular structures. In the lateral view, we see that this additional shadow is projected into the retrocardial space near the spine.
If we now look at the same thing in axial sections on a tomographic image, we can clearly see that behind the heart (near the spine), in the paravertebral region, there is a large cystic formation - an enterogenous cyst.
The addition of two contours - the contour of the right atrium and the contour of the cyst - forms two contours on the overview image. We can clearly and accurately assume immediately from the survey radiographs that this additional formation is located in the posterior part of the mediastinum - near the spine.
14:42
(Slide show).
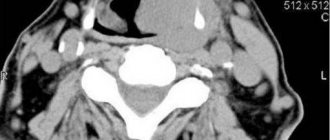
Another example. A clear widening of the mediastinum (middle shadow) to the right in a woman aged 60 years.
Could there be a heart pathology?
Yes, may be. On the X-ray in the lateral projection, you see that this low-intensity shadow is projected onto the front part - onto the region of the heart, onto the shadow of the heart.
What is this?
It immediately attracts attention that we do not see the contour of the heart, or separately the contour of the right atrium, as we should see normally. The image you see in the axial plane on the CT scan is the same cyst. The same racemose formation. In this case, it is a pericardial cyst, but only located in the anterior mediastinum.
Since it comes into contact with the chambers of the heart, naturally, we can no longer see the contours of the heart chambers here.
15:34
(Slide show).
This is a common radiological technique for recognizing pathological changes in the mediastinum. Pulmonary changes can also introduce peculiar changes into the normal structure of the mediastinum. You see here an intense, sharp, clear line that crosses the shadow of the mediastinum almost from the bifurcation and towards the diaphragm, towards the chest wall.
(Slide show).
In the lateral projection image, this is all localized in the posterior part. A typical picture of atelectasis of the lower lobe of the right lung with corresponding changes in the configuration and configuration of the structure of the mediastinal shadow.
(Slide show).
The same thing in the form of computed tomography reformation. We see a collapsed, airless lower lobe of the right lung and a pathological formation that completely blocks the lumen of the intermediate bronchus in this patient.
(Slide show).
In the lateral projection, the middle shadow breaks up into several components: the aorta, heart, elements of the pulmonary artery, and the root of the lung. The image of the mediastinum (middle shadow) here, of course, is completely different.
If you start from below and in front and move around the circle, then the most anterior lower part of the contour of the mediastinum is the right ventricle. Just above is the ascending aorta. Even further is the aortic arch. Even further is the descending aorta.
In the lateral projection we see almost the entire aortic arch along its entire length.
The posterior contour of the heart is formed in the upper part by the left atrium, and in the lower part by the left ventricle. The esophagus runs along this posterior surface, as you remember well, so contrasting of the esophagus in many cases was used before and is now still used for indirect assessment of the condition of the left chambers of the heart.
Finally, in the lowest part is the contour of the inferior vena cava, which flows here into the right atrium and crosses the contour of the left ventricle.
17:35
(Slide show).
This is how the middle shadow looks in lateral projection. Several sections of the middle shadow and mediastinum are distinguished in radiology.
One of them is the aortopulmonary window. Since we are talking about side projection images, it is clearly visible in side projection images. This space, which is located between the aortic arch and the common trunk of the pulmonary artery, is filled with air.
Why is it important?
The clearing between two large vessels is filled with fatty tissue in the mediastinum. It can be clearly detected by tomographic examination between the ascending and descending aorta and trachea.
Pathological processes often occur in this place when the normal image of the aortopulmonary window disappears. The reformation clearly shows the relationship between the pulmonary artery and the aortic arch, the reason for the appearance of such a window on an x-ray in the lateral projection.
18:42
(Slide show).
Pathology.
- Enlarged lymph nodes.
- Neoplasm of the bronchus.
- Aneurysm of the aortic arch.
- Pericardial cysts.
- Variants of vessel arrangement located here.
(Slide show).
All this can be detected already on a regular x-ray. Here you can clearly see that in the projection of the aortopulmonary window there is an additional formation. The air-containing lung tissue is practically invisible here. This is an indication to do additional research: in this case, computed tomography.
(Slide show).
You see that between the ascending and descending aorta there is a huge pathological formation emanating from the bronchus of the upper lobe of the left lung.
(Slide show).
Other sections that are traditionally identified during X-ray examination.
This is usually the retrosternal space. Enlightenment, say radiologists. The air-filled part behind the sternum, which is usually clearly visible on a plain film.
This is the retrocardial space. The same air-containing area behind the heart.
Finally, there is the retrotracheal space behind the air column of the trachea.
All these areas are filled, one way or another, with airy lung tissue. If pathological formations appear there...
(Slide show).
For example, the restrosternal space. Intrathoracic goiter or some kind of tumor of the anterior mediastinum, aneurysm of the ascending aorta, and so on. In this case, we naturally see pathological changes on a plain radiograph.
(Slide show).
In this situation, the retrocardial space: we see in the direct projection image an additional shadow that is adjacent to the descending part of the aorta. In this case, the contour of the descending aorta disappears. In the lateral projection, this formation is located against the background of the shadow of the vertebrae in the retrocardial space, we would say.
Naturally, this requires the use of additional research methods to identify the very formation that is located to the left of the descending aorta and requires appropriate treatment.
(Slide show).
Retrotracheal space. The air column in the center of the chest cavity is clearly visible. The anterior wall of the trachea and the posterior wall of the trachea. Here is an image of the scapula in lateral projection. But everything that is located behind the posterior wall of the trachea (naturally, normally this is air that shines through the mediastinum) - there should be no pathological changes here.
21:21
(Slide show).
If we see such a picture, when behind the trachea - it is pushed towards the front, curved - there is such a formation, of course, these are pathological changes that require the use of additional research methods.
In this case, it is an intrathoracic goiter, which is clearly visible during a tomographic examination.
(Slide show).
Of course, the right paratracheal space, which we already talked about today. Most often these are the lymph nodes of the mediastinum, which will be discussed later today. They enlarge and lead to modification of this area, to the disappearance of the paratracheal strip, to the expansion of the mediastinal shadow to the right, as in this patient with sarcoidosis and enlarged paratracheal lymph nodes.
Here is what concerns normal anatomy, the initial analysis of the mediastinal condition, which is usually performed by radiologists. It is very useful for all specialists who in one way or another deal with the pathology of the thoracic cavity.
This is due to the fact that even a survey X-ray (sometimes even in one projection, when it comes to examinations in intensive care conditions in the intensive care ward) in many cases makes it possible to very accurately, very reliably determine, firstly, the presence or absence of pathology. Secondly, guess where it is and what it could be.
In our conditions, of course, it is fundamentally important to decide whether something else needs to be done for this patient (some additional research). If necessary, then which ones?
I would like to stop here.
Classification of mediastinal formations
The mediastinum is anatomically divided into 3 zones. Mediastinal tumors are classified according to these zones.
- Tumors of the anterior mediastinum: lymphoma (Hodgkin and non-Hodgkin), thymoma. germ cell tumors, substernal goiter.
- Tumors of the central mediastinum: bronchogenic cyst, lymphadenopathy, pericardial cyst, tracheal tumors, esophageal tumors, esophageal anomalies (achalasia, hernia, diverticulum).
- Posterior mediastinum: neurogenic tumors, lymphadenopathy, neuroenteric cysts.
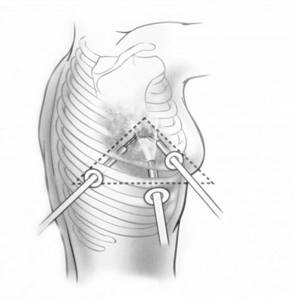
How does the da Vinci surgical robot work?
The operation of the da Vinci surgical robot is fully controlled by an experienced surgeon through small incisions no larger than 2 cm in size. An endoscope video camera inserted through one of the incisions transmits to the doctor a detailed three-dimensional image of the organ. As a result, the doctor can carefully plan the operation. The surgeon controls the instruments, which have 7 degrees of freedom of movement, thanks to EndoWrist technology and controls their movements inside the patient’s body remotely using special joysticks. Performing an operation using the da Vinci robot requires a highly qualified surgeon and special skills.
Clinical picture
Most often, mediastinal tumors are an incidental finding during X-ray examinations, since up to 40% of tumors are not clinically manifested. The clinical manifestations of a mediastinal tumor will depend on the following factors:
- location and size of the tumor;
- malignant or benign nature of the formation;
- growth rate.
Depending on the factors described above, the clinical picture may be different. The most common symptoms can be divided into two groups:
- Local: cough, hemoptysis, hoarseness, shortness of breath, difficulty breathing, chest pain, flushing of the face and upper half of the body, dilation of the veins of the face, neck, rhythm disturbances.
- General: Fever, chills, night sweats, weight loss.
How is mediastinal cancer diagnosed and treated?
Radiation diagnostic methods—radiography of the chest organs in two projections and computed tomography—help to detect a tumor. A definitive diagnosis can only be made after a morphological study of a tumor fragment. To obtain material for research, a biopsy is performed using one of the following methods:
- Transbronchial biopsy. In this case, material is collected during bronchoscopy.
- Transthoracic biopsy - the tumor is punctured through a puncture of the chest under ultrasound or CT guidance.

Video-assisted thoracoscopy and mediastinoscopy are also highly informative diagnostic methods. With their help, you can examine the chest and mediastinal cavity and, under direct visual control, take material for research.
Treatment methods for mediastinal cancer are determined by the histological type of tumor, its location and size.
Surgery
Surgical removal of the tumor is the key treatment method for mediastinal tumors of non-lymphogenic origin. During the operation, all malignant tissue, lymph nodes and fatty tissue are removed.
The complexity of surgical treatment lies in the fact that vital organs, main blood vessels and nerve trunks are located in this anatomical zone. Therefore, in an effort to radically remove the tumor, it is necessary to perform complex combined operations with resection and plastic surgery of these organs (pericardium, lungs, blood vessels).

If significant initial tumor invasion is detected, treatment begins with neoadjuvant chemotherapy, radiation, or chemoradiotherapy. After several courses, a re-examination is carried out and the question of the possibility of performing a radical operation is decided. When planning surgery, it is necessary to take into account the scarring that occurs due to radiation.
In some cases, palliative operations—tumor resection—are performed. They are designed to eliminate compression of the mediastinal organs and prevent the development of complications. After such interventions, treatment continues with chemotherapy or radiation therapy.
Chemotherapy
Chemotherapy is the main treatment for lymphogenous tumors (lymphomas) of the mediastinum. It is used in neoadjuvant and adjuvant regimens. In the first case, chemotherapy aims to reduce the size of the tumor and transfer it to a resectable state; in the second, it is to destroy the remaining malignant cells and prevent relapse.
In addition, chemotherapy is used as maintenance treatment for unresectable tumors. In this case, it is carried out to slow down tumor growth, alleviate the patient’s condition and prolong his life.
Radiation therapy
Radiation therapy is used as part of the combined treatment of radiosensitive tumors (teratomas, thymoma, etc.). Tumors with invasion into surrounding tissues are subject to preoperative irradiation. Such treatment will reduce the volume of the tumor mass and transfer it to an operable state.
Postoperative radiation therapy is prescribed for some types of mediastinal cancer that are sensitive to radiation. This may be a macroscopically residual tumor that cannot, for some reason, be removed during surgery (tumor resection), or in the presence of malignant cells at the cutting edges detected during an urgent morphological examination.
Radiation is also carried out as part of palliative treatment; it can reduce the size of the tumor, eliminate compression of the internal organs and alleviate the patient’s condition.
Diagnostics
The X-ray method is the main one for visualizing mediastinal neoplasms. Computed tomography allows you to assess the location of the tumor and plan further examination.
Without histological verification it is impossible to make a final diagnosis. If the esophagus or trachea is involved, an endoscopic examination is performed to take a biopsy and visualize the changes.
If it is impossible to obtain a tissue sample for examination, invasive methods are used endoscopically: transthoracic biopsy, mediastinoscopy, video thoracoscopic examination. The last two methods are serious operations that are performed in specialized medical institutions.
How is the procedure performed?
There is no preparation for mediastinal radiography. There are no requirements regarding diet, drinking, or time. Before the procedure, you will need to remove and remove metal items from your pockets, including watches, jewelry and piercings, and expose yourself to the waist. The patient presses his chest against the shield in which the film is clamped; approximately 2 m from him, the tube of the device is placed, from which the X-rays emanate. To create a high-quality image, a deep breath is taken at the specialist’s signal to expand the chest. The picture is taken in several projections (direct and lateral position).
During the procedure, the patient does not experience itching, pain or other sensations; it lasts a few seconds. Decoding at the NEARMEDIC clinic and preparing the image takes 5-10 minutes, after which you can go to your doctor for an accurate diagnosis.
Treatment
Due to the variety of possible causes, mediastinal tumors are treated depending on the type of tumor:
- Thymomas require surgical treatment. In high-grade cases, surgery is followed by radiation therapy. Various approaches are used to remove the tumor: both minimally invasive and robotic surgeries, as well as open “major” surgeries (thoracotomy and sternotomy).
- Lymphomas are treated with chemotherapy and radiation therapy. Surgery in this case is used as a diagnostic method, not a therapeutic one.
- Neurogenic tumors are removed surgically.
- Some tumors, if they are not clinically apparent and are benign, can be kept under observation.
Causes
The reasons leading to the development of mediastinal cancer are unknown. The following factors are believed to play a role:
- Ionizing radiation. This theory is supported by the fact that mediastinal lymphomas more often develop in people who have undergone radiation therapy for the treatment of cancer of other localizations.
- Carcinogenic substances that are found in household chemicals, agriculture and industrial production.
- Epstein-Barr viruses, HIV, etc.
- In addition, mediastinal cancer can be a consequence of malignancy of an initially benign tumor, for example, thymoma.
Prevention and prognosis
Unfortunately, no reliable methods of prevention have been identified for mediastinal tumors. But results can be significantly improved if the disease is detected at an early stage. If the symptoms described earlier do not go away within two weeks, you may need to seek qualified medical help. In this case, it is difficult to make predictions; they depend on the type of tumor and its malignancy on the treatment performed.
Bibliography:
1) Clinical recommendations of the Association of Oncologists of Russia (AOR, 2020) 2) Barbolina T. D., Bychkov M. B., Allahverdiev A. K., Borisova T. N., Vladimirova L. Yu., Gerasimov S. S., Dengina N.V., Kozlov N.A., Laktionov K.K., Levchenko E.V., Malyutina D.V., Pikin O.V. Practical recommendations for drug treatment of thymic tumors (thymoma and thymic cancer). Malignant tumors: Practical recommendations RUSSCO #3s2, 2021 (volume 10). pp. 608-619. 3) Guide to chemotherapy of tumor diseases / ed. N.I. Perevodchikova, V.A. Gorbunova. – 4th ed., expanded and supplemented. – M.: Practical Medicine, 2021.-688p. 4) Rational pharmacotherapy in oncology: a guide for practicing physicians/ed. M.I. Davydova, V.A. Gorbunova. – M.: Litterra, 2021. – 880 p. (Series “Rational pharmacotherapy”). 5) Ed. HELL. Kaprina, V.V. Starinsky, G.V. Petrova. Malignant neoplasms in Russia in 2021. (morbidity and mortality) - M.: MNIOI im. P.A. Herzen branch of the Federal State Budgetary Institution "National Medical Research Center of Radiology" of the Ministry of Health of Russia, - 2021. - ill. - 250 p. 6) Pikin O.V. et al. Tumors of the mediastinum: collection ed. Academician of the Russian Academy of Sciences, Professor A.D. Caprina. M.: Young Guard, 2021. 232 p.
Symptoms of mediastinal tumors
In 40% of cases, people with tumors in the mediastinum experience no symptoms. This primarily applies to benign neoplasms. They become symptomatic when they reach a large size and begin to compress neighboring organs, and before that they are usually detected incidentally during a chest x-ray for another reason. With malignant neoplasms, the symptoms are more pronounced and increase faster. Manifestations depend on the size, location of the tumor, its growth into surrounding tissues, and the presence of metastases. Some neoplasms release substances that enter the bloodstream and affect the functioning of other organs, causing paraneoplastic syndrome.
The symptoms are nonspecific: they occur in various diseases, and it is impossible to tell for sure whether the patient has a mediastinal tumor. The diagnosis can only be made based on the results of the examination. Possible clinical manifestations: chest pain, shortness of breath, cough, difficulty swallowing, fever, chills, night sweats, hoarseness, weight loss for no apparent reason, wheezing noisy breathing (stridor), enlarged subcutaneous lymph nodes.
Some patients experience symptoms associated with compression of nerve structures and large blood vessels by a large tumor:
- Superior vena cava syndrome is a condition in which the flow of blood from the upper part of the body is disrupted. It manifests itself in the form of headaches and dizziness, swelling of the neck, face, arms, redness (erythema) or cyanosis (cyanosis) of the skin, redness of the whites of the eyes, swelling of the veins in the neck, visual impairment. If the outflow of venous blood is very disrupted, shortness of breath, difficulty swallowing, and hoarseness occurs. Fluid may accumulate in the pleural cavity.
- Horner's syndrome occurs as a result of compression of the nerves that connect the brain to the eyes in a detour, going down into the spinal cord and then back up to the head. In this case, on the affected side, the eyelid droops, the pupil narrows and dry skin occurs as a result of impaired sweating. Similar symptoms develop in some malignant lung tumors.
- Paresis of the larynx and diaphragm as a result of compression of the nerves innervating them.
Tumors of the mediastinum can reach gigantic sizes, even occupying half of the chest. In this case, the patient's condition deteriorates greatly. Large tumors can lead to chest deformation.
Tumors of the thymus gland can lead to a number of endocrine disorders: Itsenko-Cushing syndrome (in 25–30% of patients), Eaton-Lambert syndrome, hypertrophic osteoarthropathy, ectopic production of antidiuretic hormone. There are known cases of carcinoid syndrome, when severe bluishness of the skin, attacks of suffocation, and diarrhea occur. In rare cases, the first symptoms of thymic tumors are signs of metastases in the bones, skin, and lymph nodes.