- Primary signs of pneumonia
- Viral pneumonia
- Acute pneumonia
- Atypical pneumonia in children
- Latent pneumonia in children
- Sluggish pneumonia
- Focal pneumonia in children
- Hilar pneumonia
- Community-acquired pneumonia
- Symptoms of inflammation in children
- Prices
- Make an appointment
Primary signs of pneumonia
Like other diseases, pneumonia needs to be treated at the very beginning. This will avoid complications and sometimes save the lives of babies. But there are also difficulties here, since the symptoms of the disease are one-to-one similar to the course of the flu or an acute respiratory infection. In addition, in some children, pneumonia begins sharply, suddenly, while in others, symptoms appear slowly, gradually.
Among the most common signs of pneumonia are the following:
- severe paroxysmal cough;
- sputum discharge;
- rapid breathing (over 40 breaths per minute);
- tachycardia (fast pulse);
- body temperature rises to 38? C and above and lasts longer than three days;
- increased sweating;
- redness of one of the cheeks.
“Parents should know that if a child has suffered from an acute respiratory infection, and a few days later he has a high fever, then this is a sure sign of a complication - an inflammatory process in the lungs.”
Despite the similarity of symptoms with other diseases, a combination of two or more signs should be alarming and cause you to seek emergency medical help and a more in-depth examination. Otherwise, if the presence of pneumonia is confirmed, the disease will manifest itself in more severe forms.
Insidious “silent” pneumonia
In up to half of all cases of pneumonia, in the first stage the disease occurs without classical symptoms, and general symptoms become the main ones. In such situations, a stethoscope is used for diagnosis, and radiography is used as confirmation.
A common feature of the initial stage of pneumonia is a condition called “silent” pneumonia. It is accompanied by the filling of the lungs with inflammatory fluid and blood flow, which makes listening difficult. Experienced specialists, if a disease is suspected, carry out repeated listening after 12-14 hours, since at this time the condition of the organ can change significantly.
Forms of the disease by type of pathogen
Bacterial pneumonia: types and signs
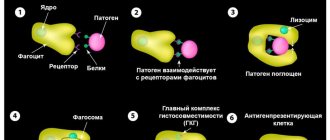
Bacterial pneumonia is an infectious disease caused by various pathogenic microorganisms. Statistics show that most often preschool children and people of retirement age suffer from bacterial pneumonia. Among the factors conducive to development, one can note a decrease in the body’s immune functions.
All pneumonias of this type are divided into nosocomial (hospital), in this case, infection occurs in a medical institution and out-of-hospital (home). The hospital-acquired disease is very severe and difficult to cure. This is due to the resistance of pathogens to antibiotic drugs.
The main causative agents of bacterial pneumonia are:
- hemophilus influenzae;
- mycoplasma;
- pneumococci (Streptococcus pneumoniae);
- staphylococci;
- Pseudomonas aeruginosa;
- chlamydia;
- Klebsiella and many others.
Symptoms and features in one-year-old children:
- In most cases, the lesion is focal, less often - lobar;
- In more than 70% of cases it is complicated by pleurisy;
- Occurs with increasing temperature;
- Accompanied by a cough - initially dry, then wet, with sputum;
- Patients experience impaired breathing;
- The disease progresses in waves.
Features of children over 5 years old:
- The disease begins gradually;
- Among the symptoms there is a cough, paroxysmal, with a small amount of sputum;
- Dry wheezing can be heard;
- Body temperature is subfebrile (from 37 to 38°C) with periodic increases to 40°C;
- Breathing is accompanied by pain in the chest;
- In one case out of five, pneumonia is not auscultated, but is detected using an x-ray.
Pneumococcus:
- Begins acutely;
- The disease is accompanied by chills and weakness;
- The temperature can be very high, or, conversely, drop to critical levels;
- When inhaling, the child feels pain;
- The cough is accompanied by the release of “rusty” sputum;
- There is redness of the cheek on the side of the affected organ;
- When exhaling, the child groans;
- Heart rate increases;
- Patients refuse to eat;
- Blood pressure decreases;
- The skin turns bluish, especially in the area of the nasolabial triangle and fingertips.
Staphylococcus:
- Affects infants;
- Accompanied by frequently recurring chills;
- Often becomes a symptom of sepsis;
- The course of the disease is severe;
- High temperature;
- Severe signs of intoxication;
- Dyspnea;
- Lung tissue is in most cases significantly damaged.
Pseudomonas aeruginosa
- More often occurs in newborns and children under three years of age;
- Develops acutely, the patient quickly reaches a serious condition;
- High temperature with characteristic morning fever peaks;
- Symptoms of intoxication are present;
- Dyspnea;
- Blue coloration of the skin (cyanosis);
- Increased heart rate.
Klebsiella
- Affects newborns and infants;
- Has an acute onset;
- Body temperature can rise to 40°C;
- Chills;
- The cough is severe;
- Separation of viscous sputum with blood clots;
- Often combined with other infections.
Atypical pneumonia
The eleven-year-old girl had been feverish for a week. In addition to the temperature, she was tormented by a painful cough and weakness. And it all started gradually - first my throat hurt, then my ears started to bother me a little, and a few days later a fever began.
The local pediatrician acted decisively: a clinical blood test had already been obtained, which showed an increase in ESR to 30, otherwise there was no pathology. The doctor also managed to give the girl a chest X-ray to rule out pneumonia. However, the description of the x-ray stated that there were no focal or infiltrative changes in the lungs.
Thus, pneumonia was not confirmed. But, despite the normal x-ray, the local police officer prescribed antibiotics: first amoxicillin - without effect, then, since the temperature persisted, cifixime. However, there was still no effect. At the time of my examination, the temperature had already risen for eight days, the cough was indomitable and painful.
“So what we’re suffering from is completely unclear,” summed up the girl’s mother. Nevertheless, I suspected 90% of what, in fact, was the matter.
Mycoplasma respiratory infection
Oddly enough, the media sometimes helps to suspect a diagnosis. When all channels are broadcasting that there is a flu epidemic, it is stupid not to take this data into account. And now, thanks to the media, I knew for sure that there was no flu in the city yet, but online publications were filled with information about outbreaks of mycoplasma pneumonia in various regions of Russia, including our north-west, as well as in border countries, for example in Finland.
Typical, classic, pneumonia is most often caused by pneumococcus, Haemophilus influenzae type B infection. It is characterized by an acute onset, often after hypothermia, high fever, intoxication, very poor health, and a severe course. A clinical blood test usually shows clear signs of inflammation; x-rays show intense infiltration. For such pneumonia, conventional penicillin antibiotics, cephalosporins and many others work well.
With atypical pneumonia, an erased long-term course is often observed. It develops gradually, sometimes there is no temperature at all. There may be a non-obvious picture on an x-ray.
Atypical pneumonia is caused by mycoplasmas, chlamydia and legionella, which are intracellular pathogens; it is not treated with all types of antibiotics. Macrolides, tetracyclines and fluoroquinolones act most effectively on these microbes.
When you say that a respiratory infection may be caused by mycoplasma, parents often become tense and scared. We have to explain that there are different types of mycoplasmas - and here we are not talking about sexual mycoplasma, but about respiratory mycoplasma, which is transmitted by ordinary airborne droplets.
Features of treatment
But let's return to our patient. It was obvious to me that pneumonia, even not visible on the x-ray, must exist. We had to try to confirm this. I usually make my patients work hard. They have to breathe long and deeply until I listen to all parts of the lungs.
After about five minutes of auscultation, my efforts were crowned with success - at the very bottom of the right lung, near the spine, I discovered a clear area of fine bubbling and creaking dry wheezing that does not disappear after coughing - a classic symptom of pneumonia. Inflammation in this place could easily have been missed on the x-ray.
Viral pneumonia: pathogens and signs
Pneumonia can be caused by various viruses, most often it is provoked by parainfluenza virus, chickenpox, measles, cytomegalovirus, viruses of categories A and B. In this case, the child’s pulmonary alveoli are filled with purulent exudate (liquid).
This form of pneumonia affects both children under one year old and older ones. Among the main signs of the disease are the following:
- in the initial stage, the cough is dry, “barking”, and with the development of inflammation it turns into a wet one;
- rapid breathing, whistling often appears;
- when coughing, the patient feels pain in the area of the shoulder blades or chest;
- the temperature is elevated;
- cyanosis of the skin of the fingertips and nasolabial triangle;
- decreased appetite;
- chills;
- dyspnea;
- headaches, muscle, joint pain.
Often, pneumonia is “masked” as a common cold and it becomes difficult to recognize. But with pneumonia, unlike a common cold, a decrease in temperature is not observed even 2-3 days after the onset of the disease.
Initially, a viral infection develops in the first 2-3 days, and then, from 3-5 days, an infection of bacterial etiology occurs. Pneumonia becomes viral-bacterial.
Detailed description of the study
Chlamydia pneumoniae is a pathogen that occupies an intermediate position between a virus and a bacterium, which causes the development of pneumonia - respiratory chlamydia. The source of infection is sick people, infection occurs by aerosol, susceptibility is high. Pathogens have a special specificity for the epithelium of the respiratory tract and cause severe pneumonia that does not leave lasting immunity. The infection can persist in the body for a long time, aggravating the course of bronchial asthma and chronic asthmatic bronchitis. There is evidence of the damaging effect of chlamydia on the vascular endothelium, which is the trigger and driving mechanism for the formation of atherosclerotic plaques.
Antibodies of the IgM class to the causative agent of respiratory chlamydia (Chlamydia pneumoniae) are specific immunoglobulins produced in the human body primarily after infection with the pathogen. The presence of IgM antibodies to chlamydia pneumonia indicates an acute stage of the disease. Antibodies of the IgM class begin to be detected no earlier than 10 days after the onset of the disease, indicating an acute form of infection, disappearing after 1-1.5 months. They are an early serological marker of this infection. C. pneumoniae causes lesions of the upper respiratory tract (laryngitis, pharyngitis, sinusitis, otitis media, bronchitis) and pneumonia in children and youth, as well as recurrent infectious diseases of the respiratory system in older age groups. The participation of C. pneumoniae in the development of atherosclerosis, bronchial asthma, sarcoidosis and Alzheimer's disease is being studied. Due to the fact that the body’s immune response to chlamydia antigens produces antibodies, this microorganism is likely to play a role in the development of autoimmune diseases. C. pneumoniae is transmitted only from person to person. Outbreaks of respiratory diseases of chlamydial etiology often occur in close groups. In 70% of infected people, the infection can persist asymptomatically in the respiratory organs. The incubation period has not been precisely established. Sometimes the disease manifests itself many months after infection, and bacteria can persist for a long time on the mucous membranes of the upper respiratory tract even after a person has recovered. Detection of respiratory diseases caused by C. pneumoniae has certain difficulties. C. pneumoniae is very difficult to detect by bacteriological culture, so the basis of diagnosis is to determine the increase in the amount of antibodies in paired sera taken during the acute period of the disease and 2 weeks after it. The sensitivity of diagnosing the disease using the paired sera method is 92%, specificity is 95%.
Acute pneumonia: features of the course and symptoms
Acute pneumonia (pneumonia acuta) is a disease that has different etiologies and, depending on the pathogen, different symptoms. Most often, this form of the disease occurs in children under 3 years of age. It is characterized by the presence of infiltrates in the lung tissues (accumulations of cellular elements with the addition of blood and lymph particles) and filling of the alveoli with exudate containing neutrophils (leukocytes that protect against infectious pathogens).
Acute pneumonia can be caused by:
- viruses;
- bacteria;
- atypical pathogens.
Pneumonia in its acute form can be either an independent disease or a complication of previously suffered diseases. Depending on the pathogen, symptoms of acute pneumonia may include the following conditions:
- signs of intoxication - fever, lack of appetite, weakness, etc.;
- when listening, changes are detected - noises, wheezing, short breathing, etc.;
- X-ray reveals areas of infiltration in the form of darkening;
- the disease in most cases is accompanied by a cough;
- respiratory failure is observed (shortness of breath, rapid breathing, etc.)
The main predisposing factor for the development of pneumonia is hypothermia.
Types of research
Parents know their child well and therefore, at the slightest change in his general condition, they begin to worry. And in some cases you should take a closer look at the baby. Pneumonia is caused in 90 out of 100 cases by bacteria (for example, streptococcus or chlamydia), and in 10 by viruses and fungi.
You need to go to a clinic to diagnose pneumonia if you have several symptoms, which are presented in detail in this article.
Any diagnosis of pneumonia contains two types of research - laboratory tests and radiation diagnostics.
Laboratory tests include the following diagnostic procedures:

Sputum examination
- clinical blood test;
- Analysis of urine;
- blood biochemistry;
- sputum microscopy.
The following procedures are included in radiation diagnostics:
- X-ray examination;
- fluorography;
- fluoroscopy;
- tomography.
In this case, the appointment of one or another diagnostic procedure is carried out depending on the age of the child and the severity of the disease.
Online test for pneumonia detection
Atypical pneumonia in children: symptoms and signs
Atypical pneumonia, or otherwise acute respiratory syndrome, is a certain form of pneumonia caused by atypical microbes - chlamydia, mycoplasma, coronaviruses, legionella. The peculiarity of atypical microorganisms is that they can multiply intracellularly. Moreover, unlike other bacteria, they are not able to exist outside the “host” cells.
Symptoms of atypical pneumonia depending on the pathogen:
Mycoplasma
More often diagnosed in children over 5 years of age. Rarely, but still there are cases of mycoplasma pneumonia in newborns.
- The disease begins gradually;
- Among the symptoms there is a cough, paroxysmal, with a small amount of sputum;
- Dry wheezing can be heard;
- Body temperature is subfebrile (from 37 to 38°C) with periodic increases to 40°C;
- Breathing is accompanied by pain in the chest;
- In one case out of five, pneumonia is not auscultated, but is detected using an x-ray.
Chlamydia
Most often affects children over 5 years of age; the first obvious symptom is a dry cough, which then turns into a wet cough.
- Occurs simultaneously with pharyngitis;
- The temperature is often subfebrile, a significant increase is possible, but without chills;
- The disease is accompanied by headaches, muscle pain, and general weakness;
- Auscultation reveals dry rales;
- Often there are no clear signs of damage on x-rays.
Coronavirus
It can affect the body of children of any age, but it is more severe in children under 2 years of age. The incubation period lasts 2-3 days
- Runny nose;
- Pain when swallowing;
- General malaise, muscle weakness;
- Headache;
- Bronchial obstruction (a form of respiratory failure that occurs due to obstruction of the bronchial tree).
Legionella
The disease is recorded in children of all ages, including infants. Average incubation period 3-5 days
- The onset of the disease is acute, with fever, chills, muscle pain and headaches;
- Initially, the cough is dry, which over time develops into a wet cough with mucus discharge;
- Pain appears behind the chest;
- When listening, fine bubbling rales are detected;
- Severe signs of intoxication (loss of appetite, vomiting, weakness, etc.);
- Tachycardia;
- Decreased blood pressure.
The first case of legionellosis was recorded in 1976 in the city of Philadelphia. During the Congress of Legionnaires - participants in military operations in Indochina, more than two hundred participants fell ill. The cause turned out to be contaminated water entering the hotel where the congressmen were staying. 34 cases of infection resulted in death.
Indicators and standards
When diagnosing pneumonia in children, an important point is a blood test. For example, knowing the indicators of leukocytes and lymphocytes, you can determine the etiology of the disease: viral or bacterial.
The most significant in diagnosing pneumonia are serological, biochemical and general blood tests. Let's look at each of them in more detail.
Determination of the etiology of the disease by blood parameters
Serological
Allows you to quickly identify microorganisms and infectious agents in cases where the results of other tests are called into question. It is done quite rarely. It is used to diagnose atypical pneumonia caused by chlamydia or mycoplasma. This study makes it possible to determine what was the source of the disease and correctly prescribe a course of antibiotics for treatment.
Polymerase chain reaction (PCR)
This test is the most effective tool for identifying atypical pathogens and viruses (mycoplasma, chlamydia). The study allows you to determine the DNA of any microorganism. The advantage is the ability to quantify the microbe in the body and the ability to detect several infections or viruses at once.
Enzyme-linked immunosorbent assay (ELISA)
Unlike PCR, this test does not detect viral agents or bacteria, but measures the amount of antibodies produced by the human immune system. Antibodies, in turn, fight the pathogen. For example, in the first 10 days of illness, the test shows the presence of class “M” immunoglobulins, later with the development of the disease – class “A”. A protracted course of infection may be indicated by the body’s production of class “G” immunoglobulins.
Biochemical
It is of great importance in diagnosing the disease. Blood biochemistry indicators are nonspecific, but enable the doctor to determine the severity of the inflammatory process and the functional activity of internal organs during pneumonia.
It is important to pay attention to the following blood parameters:
- Total protein. In the normal state of the body, the protein content is 65-85 g/l. With pneumonia, it does not increase or decrease and is within acceptable limits.
- Alpha and gamma globulin . The value of these indicators significantly exceeds the norm. This is evidence that the body is fighting inflammation.
- Fibrinogen. Slightly exceeds the norm.
- C-reactive protein . This indicator is above the norm.
- Lactate dehydrogenase (LDH) . The presented figure is slightly higher than normal.

Biochemical blood test standards
General blood analysis
The CBC has the greatest diagnostic value and contains the following indicators:
- Leukocytes. If bacterial pneumonia is present, the white blood cell count will be higher than normal. With viral pneumonia, there is a significant decrease in the number of leukocytes (leukopenia). In children, the leukocyte norm depends on age. For newborns - 9.2-13.8 x 10 to 9 degrees U/l, from one year to 3 years 6-17 x 10 to 9 degrees U/l, from 3 to 10 years - 6.1-11.4 x 10 to the 9th degree U/l.
- Leukocyte formula and its shift. When the disease is caused by bacteria, pronounced granular neutrophils are found in the blood. A significant amount of their immature (band) forms indicates bacterial pneumonia. This is the so-called shift of the leukocyte formula to the left. When there are few neutrophils in the blood and more lymphocytes than normal, this indicates the viral nature of pneumonia in a child.
- Red blood cells. With a mild course of the disease, their slight decrease is possible; with a more severe degree of pneumonia, the number of red blood cells is increased. The norm of erythrocytes for children up to one year is 4-5.3 x 10 to the 12th power g/l, from one to three years old – 3.7-5.3 x 10 to the 12th power g/l, up to 12 years – 3.7 -5.0 x 10 to 12 degrees g/l
- Lymphocytes. With a reduced number of lymphocytes, we can talk about the bacterial nature of pneumonia.
- Platelets. With pneumonia, they are within acceptable limits characteristic of age.
- Erythrocyte sedimentation rate (ESR).
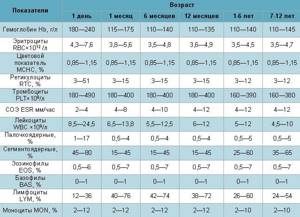
Norms of general blood test in healthy children
Erythrocyte sedimentation rate (ESR) - norm and deviation
In acute pneumonia, one of the most important signs of the presence of the disease in a child’s body is the erythrocyte sedimentation rate.
In children, this indicator varies depending on age. An increase in ESR is one of the most characteristic signs of pneumonia. At the same time, the erythrocyte sedimentation rate in the child’s blood is increased and can exceed 30 mm/h .
For comparison, ESR norms in children depending on age are as follows:
- for newborns – 2-4 mm/h;
- children under one year old - from 3 to 10 mm/h;
- children aged from one to 5 years - from 5 to 11 mm/h;
- children aged 6-14 years - from 4 to 12 mm/h.
Latent pneumonia in children: features and symptoms
This form of pneumonia is the most dangerous, as it often occurs without the symptoms characteristic of pneumonia. However, children's lungs are affected and the condition can lead to significant complications. The main reasons for the absence of obvious signs are a significant decrease in immune functions and the body’s addiction to certain drugs.
This type of pneumonia can affect children of any age, but increased danger threatens children under three years of age who cannot talk about their feelings. Parents need to be more attentive to the baby’s condition, since unexpressed signs of the disease are still present:
- drowsiness, weakness, lethargy;
- mood swings, tearfulness;
- pale skin;
- shortness of breath during physical activity;
- lack of appetite;
- pain in various parts of the body;
- increased sweating;
- increased thirst.
Statistics show that about 1,500 children die annually due to undetected latent (silent) pneumonia.
Sluggish pneumonia: symptoms and features
This type of pneumonia, which is classified as a separate category, is in most cases focal and occurs in a mild form without pronounced clinical signs. Pneumonia of this type is a complication of acute respiratory viral infection or influenza virus and has a favorable outcome. It is treated at home; difficulties can only be caused by primary diagnosis, which only includes examining the patient and collecting information.
In case of prolonged colds, the following symptoms should alert you:
- an increase in temperature two to three days after a decline;
- During the recovery period, a sudden deterioration in condition.
If there is a second “wave” of the disease, then this is a signal to seek advice from a doctor. Even without visible signs characteristic of pneumonia, such a phenomenon can be alarming and cause an x-ray to be prescribed.
Do not confuse the two concepts - sluggish and prolonged inflammation; in the second case, the disease begins acutely, and then the symptoms subside significantly.
Focal pneumonia in children: signs of the disease
Focal pneumonia, or bronchopneumonia, is most often a complication of ARVI. It develops within 5-7 days after infection. The disease is characterized by localization of the lesion in a limited area of the lung. This can be a single lesion, the minimum size of which is 10 mm. When infected with chlamydia, the lesions can be multiple. The primary symptoms of bronchopneumonia are very similar to those of a cold - cough and runny nose.
The development of infection leads to damage to the epithelial cover of the bronchi, and then damage to the lung tissue. After 5-7 days, a sharp deterioration in the condition occurs, the symptoms become more pronounced:
- severe cough, it can be both dry and wet;
- shortness of breath (in infants it can be observed even during sucking, in older children - with any, even minor, load;
- the skin becomes pale;
- breathing becomes noisy, with obvious participation of the chest muscles;
- body temperature rises to 38-39? C and can last for several days;
- feverish condition;
- increased heart rate;
- vomiting and nausea;
- enlarged liver;
- pain in the abdomen.
Pneumonia
One of the serious diseases in children is pneumonia, or pneumonia. Pneumonia can be life-threatening for a child. Fortunately, modern medicine has learned to cope well with pneumonia, and in most cases this disease can be completely cured. Therefore, if your baby gets sick with fever and cough, contact your pediatrician. If pneumonia is suspected, the doctor will order an X-ray of the lungs, which can confirm the diagnosis.
What is pneumonia?
Pneumonia is an inflammation of the lung tissue, that is, the deepest part of the respiratory organs. Normally, gas exchange occurs in the lungs, that is, oxygen from the air enters the blood, and carbon dioxide is released from the blood into the environment. When part of the lung is affected by inflammation, the respiratory function in the affected part of the lung suffers, and the child develops shortness of breath, that is, rapid and difficult breathing. Substances produced when the immune system fights bacteria cause an increase in temperature (if the body temperature rises above 38 ° C, this is called a fever). The accumulation of mucus in the alveoli and bronchi and swelling of the mucous membrane stimulate the cough reflex, and a cough occurs. If the source of pneumonia is near the lining of the lung, called the pleura, you may experience chest pain when breathing and coughing.
What causes pneumonia?
There are a lot of infections that can cause pneumonia. The most common cause of so-called “typical” pneumonia is pneumococcus (Streptococcus pneumoniae). Pneumococcal pneumonia is accompanied by fever, cough, shortness of breath, lethargy and decreased appetite. Less commonly, pneumonia is caused by other pathogens - Haemophilus influenzae type b, Streptococcus pyogenes and Staphylococcus aureus. “Atypical” pneumonia, which is usually milder and quite contagious, is caused by mycoplasmas and chlamydia. Less commonly, pneumonia is caused by viruses (adenovirus, RS virus) - such pneumonia is rare and can be very severe. Pneumonia can develop suddenly or be a complication of the flu.
What are the symptoms of pneumonia?
The most important symptom of pneumonia is fever. In a young child, fever may be the only manifestation. Fever above 39.5 °C with chills and fever that does not decrease well after taking antipyretic drugs should be especially alert. Although a high fever that does not respond well to antipyretics is not always a symptom of pneumonia. This may be a manifestation of a respiratory viral infection.
The second important symptom of pneumonia is cough. The nature of the cough matters. Particularly alarming are “deep” coughs, coughs at night, and coughs leading to vomiting.
Severe pneumonia is usually accompanied by shortness of breath, which is rapid and difficult breathing. Sometimes a symptom of pneumonia is abdominal pain, which occurs due to irritation of the pleura (the lining of the lung) due to inflammation of the area of the lung adjacent to the pleura and due to frequent coughing and, accordingly, tension in the abdominal muscles.
Very important signs that speak in favor of pneumonia are symptoms of intoxication, such as fatigue, weakness, refusal to eat and even drink. At the same time, unlike pneumococcal pneumonia, with mycoplasma pneumonia the child may feel well. Coughing and wheezing in the lungs are symptoms not only of pneumonia, but also of bronchitis.
It is very important that the doctor distinguishes pneumonia from bronchitis, since bronchitis does not always require antibiotics and only if its mycoplasmal etiology is suspected.
What can happen if pneumonia is left untreated?
This is fraught with complications, which are more likely to occur if pneumonia is not treated. Complications of pneumonia include inflammation of the pleura (pleurisy) and the formation of a cavity in the lung filled with pus (lung abscess). In such cases, a longer course of antibiotics will be required, and sometimes the help of a surgeon.
How to treat pneumonia?
For bacterial pneumonia, your doctor will prescribe an antibiotic. The doctor will decide which antibiotic to choose depending on the suspected cause of pneumonia. In most cases, a child can be given an antibiotic orally (in the form of a suspension or tablets), rather than by injection. The effect of the antibiotic occurs within 24 to 48 hours. If after 1 - 2 days the child does not feel better and the fever persists, consult your doctor again.
Usually, a child with pneumonia can be treated at home. Hospitalization is required for severe and complicated pneumonia, when the child needs intravenous antibiotics, supplemental oxygen, pleural punctures and other serious medical interventions. If the body temperature rises above 38.5 - 39 ° C, give the child antipyretics (ibuprofen or paracetamol). Antitussives, such as butamirate (the drug "Sinekod"), are contraindicated for pneumonia.
Can pneumonia be prevented?
There are vaccines designed to protect against pneumococcus and Haemophilus influenzae, which cause the most severe forms of pneumonia (against pneumococcus - Prevenar, Pneumo 23 vaccines, against Haemophilus influenzae - Act-HIB, Hiberix, a component against Haemophilus influenzae is included The Pentaxim vaccine contains components against pneumococcus and Haemophilus influenzae at the same time as Synflorix. Since pneumococcal pneumonia often develops as a complication of influenza, influenza vaccination is helpful. It is very important that parents do not smoke in the presence of the child, as secondhand smoke makes the lungs weak and vulnerable.
Hilar pneumonia: signs and special properties
This form of the disease differs in the location of the infection - it affects tissue at the pulmonary root, so hilar pneumonia is very difficult to diagnose. Different studies - x-ray, inspection and listening - can provide different information about the location of the lesion. If this happens, then most likely the child has basal pneumonia.
The disease is protracted; it may occur with pronounced symptoms of intoxication, but it may also not have them. Often it occurs without breathing problems or wheezing, with only a slight increase in body temperature. The presence or absence of symptoms depends primarily on the type of pathogen.
In infants, the presence of the disease can be determined if the baby often asks for the breast, but sucks sluggishly, the nasolabial triangle takes on a bluish color, and the skin in the intercostal space is retracted when breathing. If signs are present, they manifest themselves in the following conditions:
- severe, paroxysmal dry cough;
- release of large amounts of sputum;
- hard breathing;
- wheezing;
- rhinitis;
- sore throat;
- weakness and chills at the very beginning of the disease.
Community-acquired (out-of-hospital) pneumonia: signs of the disease
This form of the disease occurs in the first two days after the child’s hospitalization or outside the hospital and can affect one or both pulmonary lobes. Children under 5 years of age are at risk for this lesion.
The high incidence of community-acquired or home-acquired pneumonia in children is influenced by the anatomical features of the respiratory system and the body’s weak immune defense. Children's trachea and bronchi are narrow, and this causes retention and stagnation of mucus, in which pathogenic microorganisms actively multiply. Infants spend more time lying down, which can lead to blood stagnation.
Symptoms and course of the disease depend on the type of pathogen and the location of the infection. Common signs include the following:
- cough;
- increased body temperature;
- sputum production;
- chest pain when coughing and breathing;
- general weakness;
- increased sweating at night.
The prevalence of community-acquired pneumonia is quite high. But there are no exact statistics, since many cases of the disease are not recorded due to the low population seeking medical help.
Lobar pneumonia in children: special signs
With this form of pneumonia in children, the entire lobe of the lung is affected. Croupous inflammation practically does not occur in infants; it is most often diagnosed in children aged 2 to 5 years, while the more typical form of this disease is observed at an older age from 5 to 15 years. For some pathogens, such as pneumococcus, symptoms appear on the first day after infection.
The disease in children differs from that in adults:
- there is no “rusty” sputum;
- in most cases, not the entire lobe of the organ is affected, but one or more segments;
- When listening in the acute phase, wheezing is detected in only 15% of children, and in all of them during the period of resolution.
Features depending on age
Children under 3 years are a special category of patients, and in order to diagnose them with pneumonia, you need to follow this plan:
- Visual assessment of the baby's current condition.
- A complete, careful examination by a pediatrician, tapping the chest and listening with a phonendoscope. A qualified doctor will determine whether a baby has pneumonia without tests. Also, in most cases, the doctor additionally prescribes laboratory tests.
- Clinical (general blood test) is a standard diagnosis.
- Analysis of urine. It is carried out to diagnose the condition of the kidneys and the severity of intoxication.
- Bacteriological blood test.
- Study of the composition of a child's sputum.
Expert opinion

Lyudmila Sokolova
Pediatrician, doctor of the highest category
Ask a Question
If the presence of community-acquired pneumonia is suspected, as well as if there are symptoms of mild pneumonia in a child under 3 years of age, X-ray diagnostics is not a mandatory study.
children aged 4 to 10 years undergo standard measures: listening to the lungs with a phonendoscope, blood tests (general clinical, biochemical and bacteriological), urine, and sputum. When, after passing these tests, difficulties in diagnosis are observed, there are suspicions of complications and signs of a severe course of the disease, children of this age are prescribed an X-ray examination.
Starting from the age of 10, all diagnostic procedures are allowed.
Sputum examination is carried out only in older children. It is difficult to collect sputum from babies because they swallow it. Using this diagnostic method, the number of neutrophils, red blood cells, and fibrin is determined. In this way, you can find out what was the cause and causative agent of the disease. But this research result cannot be called sufficiently informative, since when collecting sputum there is a high probability of bacteria and microbes entering from the oral cavity or bronchi.
Age-related features of pneumonia in children
There are several forms of the disease:
Intrauterine transplacental
The source is the mother, infection occurs in the womb. The infection reaches the fetus through the hematogenous route, that is, through the blood. The presence of a focus of infection in the maternal body is characteristic. Often this type of disease can be accompanied by sepsis. Infants in the first hours of birth, in the presence of intrauterine pneumonia, may experience the following symptoms:
- respiratory failure;
- dyspnea;
- blue discoloration of the skin;
- wet rales.
An x-ray can immediately after birth confirm the presence of lesions.
Intrauterine amniotic
The source of infection is the mother; the pathogens enter the fetus's body along with infected amniotic fluid, which the baby swallows. One of the signs of the presence of a lesion is the diagnosis of polyhydramnios in a woman.
Intrapartum
The source is the mother's body. Infection occurs during the movement of the fetus through the birth canal. The route of transmission of infection is contact - contamination with pathogens contained in the amniotic fluid (amniotic fluid) and mucous secretions. Signs do not appear immediately, but after 2-3 days after birth. The clinical picture is similar to intrauterine infection.
The initial stage is characterized by:
- respiratory failure;
- toxicosis;
- weakness, lethargy;
- the baby refuses the breast;
- foam is released from the oral cavity.
The following signs are common:
- diarrhea;
- otitis;
- conjunctivitis
Postnatal pneumonia (domestic)
The source of infection is the people around the baby at home. Infection occurs after discharge from the hospital. The route of transmission of the infectious agent occurs through the air - aerogenic method. Most often, the disease is associated with the presence of pneumococcal pathogens and massive contamination of the upper respiratory tract.
The disease begins acutely and the following symptoms are observed:
- cough;
- heat;
- sputum discharge;
- breathing may be weak or harsh;
- fine bubbling rales are heard.
Postnatal nosocomial (in-hospital)
The source of infection is medical workers and equipment. Infection occurs after birth. There are several ways of infection - bronchogenic (the disease originates in the bronchi), contact, aerogenic (rare infection through the air). More often they begin in the first week of life with general symptoms of toxicosis.
It is characterized by signs of acute toxicosis and a change in the acid-base balance towards increasing acidity. More often, the symptoms have blurred signs and can have a rapid course with a fatal outcome. Infants on mechanical ventilation (artificial pulmonary ventilation) may develop early pneumonia - in the first 5 days, and late pneumonia - in the next 5 days.
Symptoms of inflammation in children over two years of age
More often, pneumonia develops in the presence of a cold. And a sharp jump in temperature during the improvement stage should worry parents. During the same period, intoxication symptoms and cough may increase.
The child may experience prolonged, up to a week, lethargy and sleep disturbances. Shortness of breath appears, breathing becomes more frequent. Possible pale skin. A high temperature that lasts longer than 4 days and is not brought down by traditional means can also signal the presence of an inflammatory process in the lungs.
Methods for diagnosing the disease in children
The primary method for identifying the disease is an initial appointment, which includes a survey, listening with a stethoscope, measuring body temperature, examination and palpation (palpation). If certain symptoms are present, the patient is sent to confirm the diagnosis - an x-ray examination. The image will indicate the exact location of the affected source of infection. This information is especially important for repeated cases of pneumonia.
To identify the type of pathogen, a laboratory test of mucous discharge from the nose and sputum is prescribed. For these purposes, the following methods are used:
- immunoenzyme;
- immunofluorescent;
- DNA polymerase.
A general blood test shows the number of leukocytes, acceleration of ESR and toxic granularity of neutrophils.