General blood test - transcript online
Using the online test interpretation service, you can check your results in a general blood test.
We take into account both the patient's gender and age, since the results can vary greatly in these cases. All parameter maps were compiled using medical literature. To start working with the service, indicate the gender and age of the person and select the parameters that interest you. Do not self-medicate. At the first signs of illness, consult a doctor.
The reasons why platelets in a child’s blood are higher than normal can only be determined through diagnostic measures. The clinical picture for a violation of this nature will be rather nonspecific, therefore it is strongly not recommended to independently compare the clinic and therapeutic measures. This is extremely dangerous for a child and can lead not only to complications, but also to death.
Diagnostically, an increase in platelets in a child’s blood is determined by laboratory tests. Instrumental diagnostics are carried out if necessary, depending on the current symptoms.
The prognosis is entirely individual, since everything will depend on the provoking factor and the age of the child, the state of his immune system.
An increased platelet count (thrombocytosis) is another, most often normal, feature of a clinical blood test in infants.
I remember when I first encountered this problem, about 20 years ago, I was scared. The platelet count in the blood test was 700 x 109 /l, with the normal level being up to 440. Having read in the reference book that such tests are used for sepsis and a serious condition in general patient, despite the fact that the patient seemed healthy, I sent him for a consultation with a hematologist. They examined this boy up and down and found nothing... Repeated blood tests showed slight fluctuations in elevated platelet levels. The child did not have any health problems. As the year progressed, platelets returned to normal on their own...
Since this incident, I have seen hundreds of blood tests showing elevated platelets in healthy children under one year old. Record - 1200 x 109 /l.
In fact, there are many reasons for elevated platelets. Let's list the main ones.
The most common is reactive thrombocytosis . It occurs against the background or after almost any infectious disease. If a patient has elevated platelets after suffering from pneumonia, this is not surprising. After a month and a half, everything returns to normal. But if the child managed to pick up something again during this month and a half, then thrombocytosis will not end for a long time.
Thrombocytosis can occur after bleeding or with iron deficiency. At the same time, hemoglobin and red blood cells are also reduced in the blood, and the level of iron in the biochemical analysis is low. After prescribing iron supplements, platelets return to normal within a couple of weeks.
Reactive thrombocytosis also occurs after operations, injuries, burns, against the background of severe allergies, and even after intense physical activity.
There are dangerous diseases in which thrombocytosis also occurs. For example, these are various oncohematological diseases (leukemia, lymphoma, thrombocythemia). Here symptoms such as fever, weight loss, and other pathological changes in the blood test (blasts, anemia, high ESR) are observed.
Hereditary is also described (analyze information about relatives with a similar problem, bleeding, history of thrombosis).
Thrombocytosis also occurs in diseases with systemic inflammation : rheumatoid arthritis, celiac disease, Kawasaki disease, nephrotic syndrome, inflammatory bowel diseases.
Platelets often increase after spleen removal .
***
But let's return to children under one year old. So, we have a healthy baby, he hasn’t been sick in the last month, he doesn’t have iron deficiency anemia. Before the scheduled vaccination, a clinical blood test was taken and 500 platelets were found. Let's assume that all of the above causes of thrombocytosis have been excluded, the child's hematologist examined him and found nothing wrong. What is the possible reason for this situation?
I have repeatedly looked for the answer to this question in Western literature, hoping to find information that elevated platelets up to a year are normal, but I have not found any mention at all that such a problem exists.
And this is apparently the reason - Western doctors do not require healthy children to undergo blood tests, including before vaccination. And we demand), although this probably makes no sense.
In any case, reactive thrombocytosis in children does not require treatment, goes away on its own and does not cause complications. This means you can not pay special attention to it in the absence of obvious health problems.
That is, it must be admitted that with normal health and the absence of other complaints and symptoms, elevated platelets in infants are a variant of the norm, do not require treatment, and are not a contraindication to vaccination.
Share on social media networks
RќСЂР°РІРёС‚СЃСЏ
Functions of platelet cells
A specific feature of blood platelet cells is their ability to stick together and attach to the vascular intima due to special outgrowths (pseudopodia).
As a result, primary platelet clots are formed, which play an important role in the process of stopping bleeding.
Normally, the number of platelet cells in the blood can change significantly due to stressful situations, physical activity, exposure to a painful stimulus, viral and bacterial diseases (high platelets in a child under one year old are often associated with a past infection), etc.
It should be noted that in the implementation of the main function of platelets (participation in hemostasis processes), the presence of platelet cells on the granules and membrane surface plays an important role:
- specific platelet factors (partial thromboplastin, antiheparin factor, thrombostenin);
- vasoconstrictor factors (serotonin, adrenaline, norepinephrine);
- thromboxane;
- circulating immune complexes, etc.
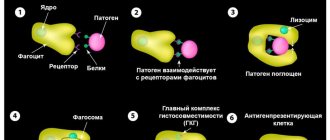
The participation of platelets in the formation of immune responses is due to their phagocytic activity, the content of IgG, lysozymes and beta-lysines (lysozyme and beta-lysine are capable of destroying the membranes of some bacterial cells).
- Platelets - their role in the body and what threatens a deviation from the norm (increase or decrease in platelets)
Platelets also contain specific peptide factors that can stimulate the transformation of “null” lymphocyte cells into mature T- and B-lymphocyte cells.
Due to this, in case of vascular injuries, platelet cells not only help stop bleeding, but also prevent pathogenic microorganisms from entering the body.
Watch this educational film about platelets with your child:
Thrombocytosis
Thrombocytosis is a significant increase in the number of platelets in the blood, which disrupts the properties of the blood and increases the likelihood of thrombosis (blockage) of blood vessels. Platelets are cells that are responsible for blood clotting.
Thrombocytosis can be either an independent disease or a consequence of a number of diseases of the blood or any organs.
Primary thrombocythemia occurs most often in people over 60 years of age. The prognosis is favorable - the life expectancy of patients with primary thrombocytosis with proper observation and treatment is practically no different from that of healthy people.
Young children are more susceptible to secondary thrombocytosis. The platelet count usually returns to normal after recovery from the underlying illness.
Synonyms Russian
Essential thrombocythemia, primary thrombocythemia, secondary thrombocythemia, thrombocytophilia, chronic thrombocythemia, chronic megakaryocytic leukemia, idiopathic thrombocythemia.
English synonyms
Primary thrombocythemia, essential thrombocythemia, idiopathic thrombocythemia, primary thrombocytosis, essential thrombocytosis, secondary thrombocytosis, reactive thrombocytosis, secondary thrombocythemia.
Symptoms
Symptoms usually develop gradually and may be absent in the initial stages of the disease. The main manifestations of thrombocytosis are caused by two factors: the formation of blood clots in blood vessels and increased bleeding. With secondary thrombocythemia, the likelihood of these disorders is lower, since the number of platelets is lower than with primary thrombocythemia.
The main symptoms of thrombocytosis:
- headache,
- pain in the hands and feet, their numbness,
- weakness, irritability,
- visual impairment,
- bleeding gums,
- nosebleeds,
- blood in the stool.
General information about the disease
Platelets are small, colorless plates that do not contain a nucleus. They are formed in the bone marrow and are “fragments” of megakaryocytes - giant multinucleated cells. From the bone marrow, platelets enter the blood, and some of them are retained in the spleen. They exist for about 7-10 days and are then destroyed by liver and spleen cells. Platelets are responsible for blood clotting and stopping bleeding. Their normal amount in the blood is 150-450×109/l.
There are two types of thrombocytosis.
1. Primary thrombocytosis. In this case, an increased number of megakaryocytes is formed in the bone marrow, which increases the number of platelets that have a normal life expectancy, but an abnormal structure and impaired functions. Platelets are large, and there is an increased tendency to form clots that block blood vessels and cause bleeding. Bleeding occurs due to disruption of platelet adhesion, and also due to the fact that most of them can be used to form blood clots. This can lead to serious complications: stroke, myocardial infarction, gastrointestinal bleeding. The causes of impaired division of megakaryocytes in the bone marrow are not fully known, however, there is information about the presence of a mutation in the V617F gene in patients. Primary thrombocytosis refers to myeloproliferative diseases in which the hematopoietic function of the bone marrow is disrupted, which stimulates the formation of blood cells.
2. Secondary (reactive) thrombocytosis. With it, platelets function normally, and the cause of the disease itself is some other abnormality, one of the following.
- Oncological diseases, most often cancer of the stomach, lungs, ovaries. Tumor cells secrete biologically active substances that activate platelet production.
- Response to irritation of the bone marrow by substances that are released by damaged tissues during: infectious diseases, most often bacterial, less often parasitic, fungal and viral,
- fractures of large bones (femur, humerus, pelvic bones),
- extensive surgical operations.
Such thrombocytosis always does not last long and disappears when the patient’s condition normalizes.
- Splenectomy – removal of the spleen. In this case, thrombocytosis is associated with the entry into the blood of those platelets that are normally found in the spleen, as well as with a decrease in the amount of substances synthesized by the spleen and inhibiting the formation of platelets in the bone marrow.
- Acute or chronic bleeding. Acute occurs suddenly and is caused by trauma, surgery, chronic lasts a long time and can accompany a stomach or duodenal ulcer, or intestinal cancer. As a result of blood loss, iron deficiency anemia occurs, that is, a decrease in the amount of hemoglobin, red blood cells and iron included in their composition. The mechanism of development of thrombocytosis in response to iron deficiency has not been fully studied. Another factor is important in this case: during blood loss, the production of red blood cells in the bone marrow is activated. The process of more active division also involves megakaryocytes, that is, the number of platelets in the blood increases. In addition, thrombocytosis is a natural response of the body, which needs additional platelets to stop bleeding.
- Chronic inflammation (colitis - inflammation of the large intestine, vasculitis - inflammation of the walls of blood vessels, rheumatoid arthritis - inflammatory disease with joint damage), in which interleukin-6 is released - an active substance that stimulates the formation of thrombopoietin, which promotes the division of megakaryocytes and the formation of platelets.
- Taking medications: glucocorticosteroids (synthetic analogs of adrenal hormones), chemotherapy drugs (vincristine).
- Recovery from thrombocytopenia caused by vitamin B12 deficiency and alcohol. Thrombocytosis in this case occurs as a response to thrombocytopenia therapy.
The likelihood of clots and bleeding with secondary thrombocytosis is lower than with primary thrombocytosis.
Who is at risk?
- People over 60 years of age (for primary thrombocytosis).
- Children (for secondary thrombocytosis).
- Patients with iron deficiency anemia.
- Having undergone surgery, severe injuries.
- Suffering from cancer.
Diagnostics
Thrombocytosis is often asymptomatic. A doctor may suspect it during a routine checkup. An important point in diagnosis is to determine the type of thrombocytosis - primary or secondary. In the case of secondary thrombocytosis, the doctor may prescribe a number of additional studies necessary to determine its cause.
Laboratory diagnostics
- Complete blood count with leukocyte formula. With thrombocytosis, the platelet level is elevated. In primary thrombocytosis, it can even exceed one million per microliter (1000×109/l), which is not typical for secondary thrombocytosis. In addition, with primary thrombocytosis, the number of other blood elements is sometimes increased: leukocytes, lymphocytes, erythrocytes. In secondary thrombocytosis, blood characteristics depend on the underlying disease, for example, during infection, the level of leukocytes may be increased. In primary thrombocytosis, large, irregularly shaped platelets are detected in the blood smear; fragments of megakaryocytes, as well as single immature leukocytes, can occasionally be found; in secondary thrombocytosis, platelets are usually not changed.
- ESR – erythrocyte sedimentation rate. May be elevated due to inflammation that causes reactive thrombocytosis.
- Ferritin is an iron-binding protein. Its level indicates the amount of iron in the body. With secondary thrombocytosis caused by iron deficiency anemia, it is reduced.
- Molecular genetic studies - identification of possible genetic disorders. With primary thrombocytosis, the structure of the gene (DNA section) JAK2V617F may be disrupted.
Additional Research
- Bone marrow biopsy is the removal of a sample of bone marrow from the breastbone or pelvis using a fine needle. It is carried out after preliminary anesthesia. In primary thrombocytosis, an increased number of megakaryocytes may be found in the bone marrow. A bone marrow biopsy is also necessary to exclude malignant blood diseases, the first sign of which may be thrombocytosis.
- Ultrasound of the abdominal organs to identify possible internal bleeding.
Treatment
Treatment of primary thrombocytosis depends on the risk of complications - thrombosis and bleeding. This is determined by age, the presence of concomitant diseases (for example, diabetes, cardiovascular diseases), and platelet levels. If the likelihood of complications is high, then use:
- drugs that suppress the production of cells in the bone marrow,
- aspirin - it thins the blood, which reduces the likelihood of blood clots,
- therapeutic thrombopheresis - in this case, using a special device, the patient’s blood is filtered to remove excess platelets.
Treatment of secondary thrombocytosis is determined by its immediate cause. As a rule, when the patient recovers from the underlying disease, the platelet level returns to normal. In addition, long-term secondary thrombocytosis can develop after splenectomy, then the patient is prescribed small doses of aspirin or drugs containing it to prevent complications.
Prevention
There is no prevention for primary thrombocytosis.
Prevention of secondary thrombocytosis consists of preventive examinations and timely identification of diseases that can lead to a secondary increase in the number of platelets.
Recommended tests
- General blood analysis
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- Coagulogram No. 1 (prothrombin (according to Quick), INR)
- Ferritin
- Cytological examination of punctates, scrapings of other organs and tissues
Platelets in babies
The norm of platelets in children (their content in the blood) is directly dependent on age:
- in newborns up to the 10th day from birth – 100-420×109/l of blood;
- in babies under 1 year of age – 150-350×109/l;
- in children after 1 year, as in adults – 180-320×109/l.
If the platelet count doubles, doctors consider it a critical condition.
Elevated platelet levels in children may indicate the presence of serious diseases such as leukemia.
About the normal platelet count in a child’s blood
The number of platelets in the body is constantly changing - these blood cells live only 7-10 days, then they are destroyed in the internal organs (mainly in the spleen and liver), and new ones are produced to replace them. The production of platelets is a constant and continuous process. Some cells are destroyed, new ones appear. Even within one day, the amount of these elements may change, but the difference will be no more than 10%.
The following indicators are the norm:
| Child's age | Blood platelet volume |
| 1-9 days | 100-420x10 to the 9th degree l |
| 10 days | 150-400x10 to the 9th degree l |
| 1 month | 160-400x10 to 9 degrees l |
| 6 months | 180-400x10 to 9 degrees l |
| 1 year | 180-400x10 to 9 degrees l |
| 2-4 years | 180-400x10 to 9 degrees l |
Minor deviations from the norm are possible, but since the permissible range is quite wide, if you go beyond its limits, you should still pay increased attention to the child’s health.
If the baby is in good health and rarely communicates with doctors, for control it is enough to take a CBC test to check the number of platelets in the blood once every six months.
Increased platelet count - thrombocytosis
This phenomenon requires treatment, adjustment of the body’s functioning in order to reduce platelets. Otherwise, the colorless bodies will aggregate into large clots, which slows down the blood flow and also leads to the formation of blood clots. And although blood clots in newborns break off extremely rarely, it is better to try to eliminate the likelihood of this process.
Children are most susceptible to thrombocytosis during periods of active growth and stressful situations.
Obvious symptoms of the disease are:
- A bluish tint to the body.
- Pain in the limbs.
- Bleeding gums.
- Enlarged spleen.
Of course, these symptoms may not be related to thrombocytosis, but if at least one of them is present, it is a priori necessary to take a blood test. There are two types of the disease.
Primary thrombocytosis
Increased platelet counts in infants can be caused by dysfunction of the bone marrow, namely, increased division of the primary (parent) platelet cell. This can be caused by heredity or the degeneration of the parent cell from a platelet into a tumor substance. This phenomenon occurs in the following diseases:
- lymphoma;
- lymphogranulomatosis;
- myeloid leukemia;
- erythermia.
Secondary thrombocytosis
Appears when the production of thrombopoietin, an activator of cell division, increases. Or when there has been significant blood loss - in this way the body tries to make up for the platelet deficiency. Secondary thrombocytosis occurs in the following cases:
- infection of the body;
- autoimmune disease;
- injury;
- prolonged bleeding;
- undergone surgery;
- splenectomy;
- chronic kidney disease;
- osteomyelitis;
- tuberculosis;
- anemia (lack of iron in the body);
- hemolysis (excessive breakdown of red blood cells).
Elevated platelets in an infant without an obvious reason require additional research to understand why their number has increased and what this can lead to. It is necessary to treat not only the consequence (which is thrombocytosis), but also the root cause - otherwise the effect on the body will not be effective.
Treatment of thrombocytosis is complex. It consists of taking medications that stabilize hematopoiesis, as well as a balanced diet dominated by dairy products, red meat, red fruits and vegetables, and sea fish. Nuts and seafood are also recommended for adults, but such components are not recommended on the menu for children in their first year of life due to increased allergenicity. It is also necessary to take multivitamin complexes, in which B vitamins predominate.
Mechanism of action
It may seem strange that such tiny blood cells play such a significant role in the functioning of the body. How does this happen?
The bottom line is this: platelets accumulate in large numbers where there is tissue damage, accompanied by blood loss. Here they connect and collapse, forming a protective sphere in the form of a blood clot, which stops the bleeding.
- Platelets are elevated in an adult - what does this mean, and how to reduce them?
In addition to performing this function, blood platelets provide nutrition to the protective layer of blood vessels - the endothelium.
Hemolytic-uremic syndrome (HUS) in children
HEMOLYTIC-UREMIC SYNDROME (HUS) is one of the common causes of acute renal failure (ARF) in children.
TRIAD OF SYMPTOMS:
- Hemolytic anemia (decrease in the level of hemoglobin and red blood cells in the blood, with the presence of fragmented red blood cells - schizocytes)
- Thrombocytopenia – decreased level of platelets in the blood
- Acute renal failure
The majority (90-95%) of children have so-called typical or postdiarrheal HUS (D+HUS).
Another form of HUS, called atypical (aHUS), is much less common (5-10% of all cases) and is the result of an abnormality (usually genetic) of proteins that regulate the process of complement activation.
D+HUS OR POSTDIARHEAL HUS
D+HUS develops as a result of an intestinal infection caused by E coli (Escherichia coli) which produces the toxin Shiga toxin (STEC).
It is observed mainly before the age of 3 years and rarely before 6 months.
Symptoms
- diarrhea (liquefied stool, diarrhea) for several days (in 90-95%). Sometimes there is blood in the stool. IF YOU NOTICE BLOOD IN YOUR STOOL, CONSULT A DOCTOR IMMEDIATELY.
- vomiting (in 30-60%) and abdominal pain
Manifestation of HUS begins on average after 6 (average 2-14) days. Paleness, general malaise, weakness, changes in behavior, slight icterus, and decreased urine output after (bloody) diarrhea should alert the physician to HUS.
IF YOUR CHILD HAS AN INTESTINAL INFECTION AND AFTER A SEVERAL DAYS YOU NOTICE DARK URINE (RED) WITH A DECREASING QUANTITY, OR NOTICE PASTY EYELIDS OR SWELLING OF THE FACIAL, PALENITY WITH YELLOWING, DO NOT CONSULT YOUR DOCTOR IMMEDIATELY!
EXPANDED PICTURE OF GUS
- hemolytic anemia (decreased hemoglobin, schizocytes)
- thrombocytopenia
- leukocytosis
AKI with increased levels of serum creatinine and urea nitrogen. Approximately half of patients have severe oliguria (decreased urine output) or anuria (complete absence of urine), and 50-60% require acute dialysis. In the presence of at least some amount of urine, micro- or macrohematuria (blood in the urine) and proteinuria (protein in the urine) are constantly determined.
EXTRA-RENAL COMPLICATIONS
- damage to the central nervous system
- damage to the gastrointestinal tract (inflammation of the large intestine - colitis, etc.)
- pancreatic swelling
- liver damage
- cardiac complications
To clarify the diagnosis, appropriate laboratory tests must be urgently carried out and treatment must be started immediately.
FORECAST
In most cases, hemolytic anemia and thrombocytopenia disappear within less than 1-2 weeks, and diuresis normalizes. On average, 10% of children reach terminal chronic renal failure within 4 months. Mortality is mainly due to damage to the central nervous system (CNS).
ADVICE FOR PARENTS
PREVENTING STEC (shiga toxin-containing Escherichia coli) INFECTION and HUS development
- chopped beef should be well cooked until it turns gray when cut
- children under 3 years of age should not consume unpasteurized products (milk, cheese, fruit juices)
- Before preparing food, especially after handling minced beef, you must wash your hands
- Children who have touched cattle and other animals should wash themselves afterwards and before eating.
- To prevent contamination of meat with intestinal contents, control of slaughter is necessary. Proper supervision and care of water supply is important
- antibiotics? Numerous studies have shown that antibiotic therapy during diarrhea increases the risk of developing HUS, possibly due to the release of Shiga toxin as a result of bacterial lysis. However, this risk has not yet been proven.
For more information, call the doctors of the department: +
Types and causes of thrombocytosis
Thrombocytosis is of two types:
- Primary thrombocytosis, in which the number of megakaryocytes in the bone marrow increases. This, in turn, leads to an increase in the number of platelets with a normal life expectancy, but impaired functions and abnormal structure. These platelets tend to be large, increasing the tendency for them to bleed and form clots that can block blood vessels. Bleeding occurs because platelet aggregation is disrupted and because most of them can be used to form blood clots. This condition can provoke serious complications: myocardial infarction, stroke, gastrointestinal bleeding. At the moment, the reasons why the division of megakaryocytes in the bone marrow is disrupted are unknown, but scientists have information that patients have a mutation in the V617F gene. Primary thrombocytosis is a myeloproliferative disorder. In such diseases, the hematopoietic function of the bone marrow is disrupted, which stimulates the formation of blood cells.
- Secondary (or reactive) thrombocytosis, in which platelets function normally, but the disease itself is formed due to one of the following abnormalities:
With secondary thrombocytosis, the likelihood of bleeding and clots is usually lower than with primary thrombocytosis.- Oncological diseases (most often ovarian, lung, stomach cancer);
Response to irritation of the bone marrow by certain substances that damaged tissues release during: fractures of large bones; infectious diseases (usually bacterial, less often viral, fungal and parasitic); serious and large-scale surgical operations: Removal of the spleen (splenectomy);
- Chronic or acute bleeding;
- Chronic inflammation;
- Taking certain medications: chemotherapy drugs and glucocorticosteroids;
- Recovery from thrombocytopenia (which was caused by alcohol or vitamin B12 deficiency).