The baby’s health directly depends on the results of his tests. One of the important indicators of the general condition of the baby is a stool analysis. Feces are the result of a complex process of biochemical reactions, with the help of which an appropriate diagnosis can be made, and only then the necessary treatment can be prescribed.
Malabsorption syndrome
is a syndrome of malabsorption of food components in the small intestine. The absorption or absorption of monomers (fatty acids, amino acids, monosaccharides, etc.) is preceded by hydrolysis - the breakdown of food polymers (proteins, fats and carbohydrates) under the influence of digestive enzymes. Violation of polymer hydrolysis due to insufficiency of digestive enzymes (digestive enzymes) is called maldigestion syndrome or digestive insufficiency syndrome. The combination of both types of disorders, malabsorption and maldigestion, which is often encountered in clinical practice, was proposed to be designated as malassimilation syndrome. However, in the medical literature, all disorders of intestinal absorption caused by both the pathology of the absorption process itself and the insufficiency of digestive enzymes are traditionally called malabsorption. Malabsorption syndrome is accompanied by a whole group of diseases, the development of which is based on hereditary or secondary (in pathology of the pancreas or other organs of the digestive system) enzyme deficiency.
In the first year of life, malabsorption syndrome is most often a genetic hereditary pathology; the most well-known hereditary enzymopathies are disaccharidase deficiency, celiac disease and cystic fibrosis.
How to lower the level of leukocytes in a coprogram
Treatment for excess white blood cells involves eliminating the cause and lowering the white blood cell level. The child must be shown to a doctor if the following symptoms occur:
- frequent fatigue and drowsiness;
- general malaise;
- increased body temperature;
- urination less often than usual with an uncharacteristic odor and color;
- quiet crying, with almost no visible tears;
- dry mouth;
- frequent diarrhea with a strong odor;
- vomit.
If a child experiences such signs, immediate consultation with a doctor is required. This is associated with an increased risk of dehydration and even death!
By contacting a doctor in a timely manner, taking tests and immediately starting to treat the child, parents increase the chances of a good prognosis for the disease and rapid recovery of the baby’s body. The doctor prescribes treatment with Lactazar, Acipol, Bifidumbacterin, Linex or other drugs. It is only allowed for children over 3 years of age and adults - infants have hearing problems.
It is also impossible to treat with prescribed medications for too long - dysbacteriosis may occur. But you cannot prescribe or cancel medications on your own - such actions are performed only under the close supervision of a doctor. Incorrect treatment can only make the situation worse.
0 0 votes
Article rating
Disaccharidase deficiency.
Disaccharides are components of most carbohydrates. Their digestion processes are ensured by special intestinal enzymes - disaccharidases. After the breakdown of disaccharides, monosaccharides are formed, which can then be absorbed through the intestinal transport systems. Disaccharide intolerance in children is caused by a hereditary absence or decreased activity of one or more intestinal disaccharidases, resulting in incomplete breakdown of disaccharides in the small intestine. By peristaltic movements of the intestine, incompletely broken down disaccharides move to the lower parts of the digestive tract, where, under the influence of natural microflora, they transform into organic acids, sugars and hydrogen. These substances reduce the absorption of water and salts from the intestinal cavity, i.e., food gruel (chyme) becomes liquefied, and this leads to the development of diarrhea in the child. Symptoms of primary disaccharidase deficiency usually appear in a child immediately after birth. This group of diseases is characterized by the fact that with age, some compensation of impaired enzymatic functions occurs, and the symptoms of the disease soften or disappear altogether. Among the hereditary defects of disaccharidases, the most well-known are lactose, sucrose, isomaltase, and trehalase deficiency. Lactase deficiency is explained by a mutation in the gene that is responsible for the synthesis of lactose, as a result of which this enzyme is either not synthesized at all (alactasia) or its low-active form is synthesized (hypolactasia). Therefore, when lactose enters the intestine, it is not completely broken down by inferior lactose, and a characteristic symptom of malabsorption develops - diarrhea.
Lactose is the main component of milk, including human milk, so treating severe forms of lactose deficiency in infants is quite a difficult task. Lactase deficiency manifests itself from the first days of a child’s life, as soon as he begins to eat. There are two forms of lactose deficiency. The first form (congenital lactose intolerance of the Holzel type) has a more benign course. Newborns with this form of the disease develop foamy, watery stools with a sour smell of vinegar or fermented wine, and there may be streaks of mucus in the stool. You can hear rumbling in the stomach, flatulence is pronounced, and gases escape profusely. The general condition of the child is usually satisfactory, appetite is not impaired, children suck well, body weight increases normally. Some children tolerate small amounts of lactose quite well; they develop diarrhea only when they receive it in quantities that lactose with reduced activity cannot cope with. If the course is favorable, the symptoms of the disease completely disappear after milk is excluded from the newborn's diet. By 1-2 years of life, lactose deficiency is compensated to one degree or another. In severe cases, the addition of a secondary infection may lead to the formation of metabolic disorders and chronic nutritional disorders that do not go away with age. The second form (congenital lactose intolerance of the Durand type) is characterized by a more severe course. After the first feeding, the child develops watery stools and vomiting. Growth and weight gain are slow. Over time, severe metabolic disorders develop, affecting the kidneys and nervous system. There may be hemorrhagic disorders. Vomiting in some cases is persistent (reminiscent of vomiting due to pyloric stenosis), leading to dehydration of the child. Treatment with a lactose-free diet is ineffective. The main component of the treatment of lactose deficiency for breastfed children is the use of enzymes (containing lactose), and for bottle-fed children, the use of special formulas (lactose-free).
Parents need to know that lactose is found not only in whole breast milk, cow's and goat's milk, but also in all types of powdered milk, many fermented milk products (sour cream), condensed milk, and also in some medications as a filler. Therefore, when prescribing a medicine, you should inform your doctor about the existing lactose deficiency and carefully read the drug label. In mild cases of lactose intolerance, dairy products and milk treated with B-galactosidase preparations are given instead of milk. Children with lactose intolerance are advised to eat products containing fructose (vegetable and fruit purees), which is well absorbed and does not undergo bacterial fermentation. In addition to therapeutic nutrition, enzymatic preparations are prescribed in a short course (5-7 days) in the first days of illness. Probiotics are used for 30-45 days to normalize the intestines. Sucrose and isomaltase deficiency often occur together. In children who are bottle-fed, there are no signs of deficiency of these enzymes. Symptoms of the disease appear after the child eats food containing sucrose and starch (sugar, potatoes, semolina, flour products) when transferring him to artificial feeding or after introducing complementary foods. After eating such food, the child experiences foamy, watery stools and vomiting. In severe cases and the child is bottle-fed with formulas containing sucrose, vomiting becomes persistent and the child loses weight. The diagnosis of sucrose intolerance is confirmed by performing a sucrose load test. Treatment consists of following a diet excluding foods containing sucrose and starch. You can eat fruits and vegetables in which the amount of sucrose is small (carrots, apples). The prognosis is favorable. With age, enzyme deficiency is compensated, and the diet can be expanded.
Diet before taking the test
Regardless of which method the study will be carried out, you should prepare for it by following a diet. Doctors recommend 2 types of diets:
- According to Pevzner. This Soviet doctor developed a number of diets for the treatment of gastrointestinal diseases and the rehabilitation of those who had cholecystitis and hepatitis. During the diet, the child is fed potatoes, butter, vegetables, vegetable soups, buckwheat and rice porridge, sauerkraut and apples. To improve intestinal motility, crumbs exclude meat, fish and confectionery products from the menu.
- According to Schmidt. The menu includes milk oatmeal, potatoes, eggs, milk and butter. This diet is also prescribed before coprology to check for bleeding. Then the child’s menu should not contain green vegetables, tomatoes, fish and meat.
Parents should also take into account that some medications can distort the results of coprograms. This issue should be discussed with the treating pediatrician or pediatric gastroenterologist before the analysis.
Celiac disease (celiac disease)
is a chronic hereditary disease that develops due to a deficiency of enzymes involved in the digestion of gluten. In recent years, due to improved diagnostic quality, celiac disease is being detected more and more often. Gluten is a component of the gluten of a number of cereal crops - wheat, rye, barley, oats. When gluten breaks down, a toxic product is formed - gliadin, which has a damaging effect on the mucous membrane of the small intestine. However, normally in healthy children gliadin does not damage the mucous membrane, since specific enzymes break it down into non-toxic substances. With celiac disease, there is a deficiency of these enzymes to varying degrees (up to their complete absence). As a result, gluten is not hydrolyzed in the intestine, but accumulates along with the products of its incomplete breakdown, causing a toxic effect on the mucous membrane of the small intestine, cells of the small intestinal mucosa die, and digestive and absorption functions are disrupted. In typical cases of celiac disease, the disease has a chronic course with periods of exacerbation and remission.
The first signs of celiac disease appear in a child in the second half of life after the introduction of complementary foods that contain gluten from cereals (semolina, wheat, oatmeal).
If a child is bottle-fed with formulas containing wheat flour, then the symptoms of the disease appear earlier. From the moment gluten-containing products are introduced into a child’s diet until symptoms appear, it usually takes 4-8 weeks. The main signs of celiac disease are dystrophy, weight loss and stunting, diarrhea, steatorrhea (the presence of undigested fats in the stool) and damage to the central nervous system. The celiac disease clinic is developing gradually. First, the child’s appetite decreases, lethargy, weakness, and frequent regurgitation appear. Subsequently, regurgitation turns into vomiting, and diarrhea develops. Feces in celiac disease are sharply foul-smelling, copious, foamy, pale with a grayish tint, and shiny. The child stops gaining weight, and then his body weight decreases. Children are severely stunted. The abdomen is enlarged, which, in combination with thin limbs, gives the child a characteristic appearance - a “backpack with legs.” The child’s facial expression is sad, facial expressions are poor (“unhappy look”). Over time, other organs of the digestive system are affected - the liver, pancreas, duodenum. Liver cirrhosis may develop. There is a moderate increase in the size of the liver and spleen. Violation of the enzyme-forming function of the pancreas leads to even greater inhibition of the digestive process. It is possible to develop secondary insulin deficiency, which explains the symptoms of diabetes mellitus (increased urine output and thirst) during an exacerbation of the disease. All types of metabolism suffer, especially protein metabolism. A deficiency of amino acids develops, the concentration of total lipids and cholesterol decreases, and the amount of ketone bodies in the blood serum increases. Metabolic disorders are manifested by rickets, polyhypovitaminosis, and anemia. Children may experience baldness of the scalp (alopecia), and fractures of long bones are common. A secondary immunodeficiency state develops; children are susceptible to frequent colds, which are more severe and last longer. All children have disorders of the central nervous system (metabolic-toxic encephalopathy), children are irritable, capricious, and lagging behind in psychomotor development. To confirm the diagnosis of celiac disease, a gluten provocation test and examination of a biopsy of the mucous membrane of the duodenum or jejunum are used.
The main method of treating celiac disease is diet therapy - excluding from the diet of a sick child all products containing gluten (bread, bakery, confectionery and pasta, semolina, oatmeal, pearl barley, wheat and barley cereals and industrially produced porridges from these cereals). Since flour and other processed products of gluten-containing cereals are often added to sausages, frankfurters, canned meat and fish (including those intended for baby food), they are also excluded from the child’s diet. During the acute period of the disease, enzymes, vitamins, and probiotics are also used.
In extremely severe forms of celiac disease and low effectiveness of diet therapy, glucocorticoids (hormones) are used for a short course with gradual withdrawal thereafter. Parents should remember that a gluten-free diet should be followed for life, even if signs of the disease completely disappear. Failure to follow the diet can lead to a more severe relapse of the disease, and the resulting violations will be difficult to compensate for.
Why do children's stool contain leukocytes?
To protect against infections, the body produces white blood cells. Moreover, with increasing age, the norm of indicators decreases. So, in a child aged 14 - 16 years, the normal level of neutrophils is 7.5 * 109 / l, and in an infant - 15 * 109 / l. The newborn’s body more actively fights infectious diseases.
The leukocyte level does not increase without a reason. A newborn's stool is sterile and olive-colored. Then parents notice a change in the color of the stool. There is no cause for concern as the bowel movements will continue to be greenish-brown until the baby is 2 weeks old. During this period, the baby's stool is formed. For children aged 1 year and older, it is formalized.
But if there is a serious excess of leukocytes in the stool, or the appearance of an uncharacteristic smell or color of the stool, you should contact your pediatrician. Perhaps this condition was caused by infectious diseases. To identify and eliminate the causes that provoked this condition, a high-quality diagnosis is required, on the basis of which the doctor will refer you to the right specialist. Most often, a consultation with a pediatric gastroenterologist is needed, who will then determine the appropriate treatment.
Intestinal form of cystic fibrosis.
A genetic defect in this hereditary disease disrupts the reabsorption of sodium chloride by all exocrine glands, as a result of which their secretion becomes viscous, thick, and its outflow is difficult. The secretion stagnates in the excretory ducts of the glands, they expand, and cysts form. Glandular cells die. The most common forms of cystic fibrosis are intestinal and pulmonary, in which the glands of the intestine or bronchi are predominantly affected, respectively. Combined forms may occur. Damage to the intestinal glands in cystic fibrosis leads to significantly impaired processes of digestion and absorption of food components (maldigestion and malabsorption syndromes). Fat digestion suffers to a greater extent, which is associated with inhibition of the enzymatic activity of the pancreas, which also suffers in cystic fibrosis.
In newborns, the intestinal form of cystic fibrosis can manifest as meconium ileus - intestinal obstruction as a result of blockage of the intestinal lumen by thick and viscous meconium. Normally, newborns should pass meconium on the first day of life. If this does not happen, suspicion should arise regarding cystic fibrosis, especially if the parents or close relatives of the child have signs of this disease. Complications of meconium ileus are perforation (formation of a hole) in the intestinal wall and the development of a serious condition - meconium peritonitis (inflammation of the peritoneum).
In the first year of life, a child with cystic fibrosis, despite good care, rational feeding and good appetite, does not gain weight well. Signs of cystic fibrosis appear especially clearly during the transition from breastfeeding to mixed or artificial feeding. The appearance of children with cystic fibrosis is characteristic: a “doll” face, a deformed chest, a large swollen abdomen, and often an umbilical hernia. The limbs are thin, there is deformation (thickening) of the terminal phalanges of the fingers in the form of drumsticks. The skin is dry, its color is grayish-earthy. The child's stool is copious, liquid, grayish in color, with a fetid specific smell of rancid fat (“mouse smell”), greasy and shiny, and is poorly washed off from the potty and diapers. A common symptom of “slipping” is when the child has stool immediately after feeding. In some cases, there may be constipation, putty-like stool consistency, or the release of liquefied stool preceded by the release of fecal impaction. Constipation often causes prolapse of the rectal mucosa (as a rule, surgical correction is not required in this case). Sometimes undigested fat flows out of the baby's anus in the form of an oily liquid, leaving a greasy residue on the diaper. If defecation and urination occur simultaneously, fat floats on the surface of the urine in the form of oily films. Due to constant long-term disruption of the digestive processes, the child, against the background of a usually good or increased appetite, loses weight (up to the development of severe forms of exhaustion), signs of deficiency of various vitamins appear (polyhypovitaminosis), and metabolic processes suffer. Children are lagging behind in physical development. Diagnosis of cystic fibrosis is carried out using stool examination (determination of undigested food debris), determination of trypsin in stool, sweat tests (sodium and chlorine content in sweat fluid is determined) and using a specific genetic study with identification of the mutant gene. Treatment for the intestinal form of cystic fibrosis is aimed at improving digestion processes. In severe and moderately severe condition of the child, when malabsorption syndrome is combined with dehydration and severe toxicosis, the diet begins with a water-tea break. The child is fed at the rate of 100-150 ml/kg of body weight per day with a 5% glucose solution, rehydron, green tea, etc. In severe cases, glucose-saline solutions are also administered intravenously. In the hospital during the acute period, a short course of hormonal therapy and vitamins are prescribed. After the exacerbation is relieved, the child is transferred to a diet with a feeding frequency of 8-10 times a day. Children in the first year of life continue to receive breast milk, which is the optimal type of food for them. When artificial feeding, preference should be given to mixtures that contain fats in the form of medium chain triglycerides. These fat components do not require the participation of pancreatic enzymes for their digestion and are therefore easily absorbed. After the introduction of complementary foods and in later life, the child's diet should include minimal amounts of fat and large amounts of protein. Patients with cystic fibrosis need an increased amount of protein, as it is lost in a significant amount due to malabsorption syndrome. Therefore, from the age of 7 months, it is necessary to include high-protein foods such as meat, fish, eggs and cottage cheese in a child’s diet. In addition to the diet, individually selected dosages of enzyme preparations are prescribed. To normalize the intestinal biocenosis, preparations of normal intestinal flora are used in courses of 2-3 months or more. Vitamin therapy courses are provided. Parents should closely monitor the child’s condition, and if there are indications in the family that relatives may have the disease (the parents themselves may be healthy), inform the pediatrician about this.
General information about white blood cells in infants
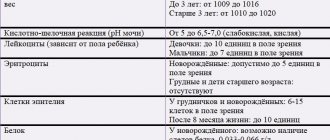
We have already found out that the appearance of white immune cells in large numbers in the stool sometimes indicates a hidden inflammatory process or infection. Such cells are detected during laboratory tests (coprogram). Doctors believe that a slight excess of the norm does not matter in the diagnosis, given that the child’s condition is satisfactory. Let's consider what is considered normal leukocyte content.
Table 1. Norms of leukocytes in the coprogram of children of different ages
| Child's age | Number of leukocytes in the field of view |
| Newborn (up to 28 days) | 101005 |
| Month | 81002 |
| Six months | 81001 |
| Year | 81000 |
| Up to five years | 81000 |
If leukocytes are found in the stool above normal, the laboratory technician can enter the following by hand in the analysis results: “thickly,” “throughout the entire grid,” “entirely,” and the like. It is important to understand that an increase in white blood cells can be diagnosed in a completely healthy baby. If a child is developing according to his age, eats well, is often in a good mood, is not capricious, and is active, then there is no need to sound the alarm ahead of time.
An unpleasant burning sensation in the esophagus and throat, as well as fatty belching are signs of heartburn. They are accompanied by a feeling of bitter-sour taste and sore throat. Read more in the article: “constant heartburn: causes and treatment.”