Adenomyosis of the uterus is a gynecological disease of a benign nature, in which endometrial cells grow into the walls of the organ, leading to disruption of its functions and infertility. The exact causes of the pathology have not yet been established, but doctors have identified a number of predisposing factors that, under a combination of unfavorable circumstances, can become a trigger for the development of adenomyosis. At the initial stages of development, the disease does not manifest itself in any way. But as it progresses, pronounced clinical symptoms are disturbing, which should be a reason to visit a gynecologist as soon as possible and undergo a comprehensive examination. One of the methods for diagnosing adenomyosis is ultrasound examination (US). Echosigns of uterine adenomyosis are manifested by changes in the density of organ tissue, the presence of areas with hypoechogenicity, hyperechogenicity and heteroechogenicity. The treating gynecologist interprets the ultrasound results and, based on the data obtained, will select the most effective treatment plan. The medical clinic is equipped with high-precision ultrasound diagnostic equipment of the new generation, with which you can determine the diagnosis at the earliest stages.
What is adenomyosis
Adenomyosis is a benign hormone-dependent tumor formed by endometrial cells that grow uncontrollably, affecting the myometrium to varying depths. Depending on the nature of the course and the type of changes inside the walls of the uterus, the following forms of the disease are distinguished:
- Focal. In the focal form, endometriotic tissue grows into the myometrium in the form of locally located focal areas.
- Nodal. This type is characterized by damage to the walls of the reproductive organ by glandular epithelial cells in the form of multiple nodules.
- Diffuse. With diffuse adenomyosis, the growth of pathological cells occurs to different depths, sometimes forming fistulas in the pelvic area.
- Diffuse nodular. Combines diffuse and nodular types of adenomyosis.
Adenomyosis occurs in 4 stages:
- First. Pathological processes are limited to the myometrial mucosa; any suspicious symptoms indicating the disease are completely absent.
- Second. Endometriotic cells spread to the muscle tissue of the reproductive organ, the clinical picture is absent or mild.
- Third. The pathological process affects the entire thickness of the muscle wall, right down to the serous membrane. Certain symptoms are concerning.
- Fourth. The muscular layer of the uterus is completely affected by endometrial tissue, which can also grow into the tissue of organs located nearby. The clinical picture is clearly expressed.
How does adenomyosis develop?
Adenomyosis is one of the types of endometriosis. To understand the mechanism of pathology, it is important to know the structure and basic functions of the uterus. The body of the uterus consists of smooth muscle. But muscle tissue itself is not enough to bear and give birth to a child. During each menstrual cycle, the body produces a special layer to which the fertilized egg attaches and develops further. This layer is called the endometrium. The endometrium, in turn, consists of 2 membranes:
- Functional. Designed for bearing a fetus.
- Basal. The shell from which the functional layer grows.
If fertilization does not occur during the cycle, the functional membrane is rejected and leaves the uterus along with menstrual bleeding. In the next cycle, the functional layer is formed again. But under the influence of negative factors, a malfunction occurs; the endometrium damages the basal layer, as well as the membrane, and in some places begins to grow into the body of the uterus. The reproductive organ reacts to the failure by forming thickenings of muscle fibers around the pathological foci, trying to limit further spread. As a result, the body of the uterus increases in size, which leads to disruption of its functioning.
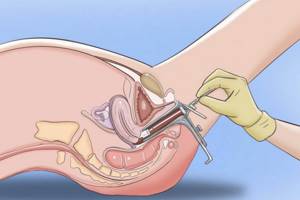
What are the features of using ultrasound?
If the development of adenomyosis is suspected, the gynecologist, after an initial examination, gives a referral for an ultrasound examination, which is performed transvaginally. This ultrasound examination method is not used in girls and young women who are not yet sexually active.

For an ultrasound to be informative and effective, you need to prepare for it. Basic rules of preparation:
- 2–3 days before the procedure, exclude from the diet foods that contribute to increased gas formation.
- The evening before the test, drink a laxative and have a bowel movement.
- Before manipulation, empty your bladder.
If there are contraindications for transvaginal ultrasound, transabdomial ultrasound is prescribed. To confirm the diagnosis, the following diagnostic procedures may be additionally prescribed:
- hysteroscopy;
- Ultrasound of the uterus with Dopplerography, elasography;
- hysterosalpinography;
- Ultrasound of the ovaries.
Methods for performing ultrasound of the pelvic organs
There are two diagnostic methods - transabdominal and transvaginal. Transabdominal is used more often because of its simplicity - the examination is carried out with a sensor through the abdominal wall, the person being examined is conveniently located on the couch and does not experience any unpleasant sensations. The key to a successful transabdominal examination is a full bladder, thanks to which the pelvic organs are positioned most successfully for proper visualization on the monitor.
At the same time, the transvaginal method (the study is carried out using a shallowly inserted vaginal sensor, and is not accompanied by any negative sensations) still has an undeniable advantage - it shows a more complete and accurate picture due to the closer location of the sensor to the area being examined. If the doctor wants to get the clearest possible picture or requires clarification of some diagnostic points, both methods of examination are carried out in one session.
Manifestations of adenomyosis on an ultrasound echogram

Signs of uterine adenomyosis on ultrasound are characterized by noticeable deviations from generally accepted physiological norms. Pathology is best visualized at the beginning of the second cycle of the luteal phase, when endometrial functions are most active.
Characteristic echo signs of adenomyosis on ultrasound:
- heterogeneity of myometrial tissue;
- blurred boundaries between the germ and muscle layers;
- rounded shape of the organ;
- asymmetry in wall thickness;
- the presence of endometrial spiral vessels in the myometrium;
- deviation from the norms in length, width, weight by more than 10%;
- pockets of compaction, voids more than 2 mm inside the muscle layer.
Adenomyosis on ultrasound is manifested by changes in the density of uterine tissue, as well as the presence of areas with hypoechogenicity, hyperechogenicity, and heteroechogenicity. Also, during an ultrasound examination, pathological spots with impaired density ranging in size from 1 to 50 mm are detected.
How is the research conducted?
Transperineal ultrasound examination is carried out with a convex or sector probe of 5-7.5 MHz with a rubber cap on, with the patient on the left side with legs brought to the abdomen or on the back with legs apart and bent. Thus, with the help of echography, it seems possible to quite accurately and objectively determine the size of the prostate gland using a combination of transperineal and transabdominal approaches).
Using this technique, it is possible to obtain images in both longitudinal and transverse sections. The volume of the pancreas is calculated as during a transabdominal examination. The anteroposterior dimension is measured in a transverse section of the pancreas, and the superior-inferior and transverse dimensions are measured in a longitudinal section. Its echostructure, features of the internal and external blood supply, and the prostatic uterus are also assessed. In addition, this scan allows in a number of patients to identify the processus vaginalis of the urogenital sinus (POUS), assess its internal structure, size, and also detect echographic signs of inflammatory changes.
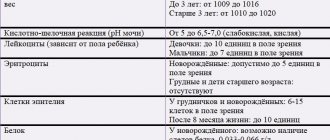
Decoding the ultrasound protocol
The results of the ultrasound are recorded in a protocol, which will be deciphered by the gynecologist. When studying the data obtained, the specialist first of all pays attention to the parameters of the organ and their compliance with the standards.
Sonographic signs of the absence of adenomyosis:
- Size – corresponds to physiological standards.
- The shape is pear-shaped.
- The wall thickness is uniform and symmetrical.
- The contours of the boundaries between the muscle and growth layers are clear, even, without bulges.
- The structure of the myometrium is unchanged, homogeneous.
- The thickness of the functional layer of the myometrium corresponds to the phase of the cycle, there is no deformation of reflection according to M-echo.
If echo signs of uterine adenomyosis are visualized, the doctor evaluates the form, localization and stage of the disease, after which he draws up an individual treatment plan or prescribes surgery.
Signs of adenomyosis development on ultrasound
Ultrasound signs of adenomyosis in the initial stages of development are clearly visualized on the monitor:
- The presence of tubes from the endometrium to the myometrium.
- Formation of circles or ovals, as well as notches in the basal layer.
- Various defects in the endometrial layer.
As adenomyosis progresses, signs of adenomyosis on ultrasound become more pronounced:
- asymmetry of the walls;
- increase in size;
- uneven increase in the posterior and anterior walls.
Adenomyosis as a pathology of the endometrium
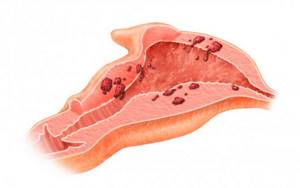
Uterine adenomyosis is a common disease of benign etiology, diagnosed in women of childbearing age. Pathology is considered as one of the stages of endometriosis. According to the location of endometriosis, it can be:
- genital;
- extragenital.
Genital, in turn, is internal and external. When internal, the body of the uterus and the supravaginal cervical part are affected. Externally, pathological processes occur in the following areas:
- body of the uterus and part of the cervix;
- retrocervical zone;
- the fallopian tubes;
- vagina;
- ovaries;
- Douglas space.
Indications for uterine ultrasound
Gynecologists recommend that women who exhibit symptoms of reproductive system diseases undergo ultrasound diagnostics. These include nagging abdominal pain, cycle failure, painful and prolonged menstruation, uterine bleeding, vaginal discharge, etc.
Diseases that require monitoring by ultrasound:
- Infertility.
- Uterine fibroids.
- Endometriosis.
- Polyps.
- Ectopic pregnancy.
- Ovarian cysts and others.
If there is a predisposition to the development of gynecological diseases (frequent inflammation, thrush), then doctors advise patients to periodically undergo ultrasound diagnostics for preventive purposes. In addition, ultrasound is indicated for pregnant women as a screening observation. After a caesarean section, it is mandatory to diagnose a scar on the uterus.
Reasons for development
The root causes of the development of the pathology have not been fully established. But doctors put forward various theories with the help of which they try to explain the etiology and pathogenesis of adenomyosis. A popular theory is the implantation of separated endometrial cells during retrograde reflux of menstrual blood through the fallopian tubes.
There are theories that speak of the spread of pathological cells by hematogenous and lymphatic routes. The genetic factor may also play a significant role, given the concordance of the manifestation of adenomyosis in twins. Many medical studies have been conducted in search of the exact root cause of the pathology, but doctors have not received a clear answer to this question.
Contraindications
The medical equipment used makes it possible to minimize discomfort from transrectal examination. However, it should still be abandoned during an exacerbation of hemorrhoids and anal fissures. The examination is also replaced by a transabdominal one if the patient cannot overcome the psychological barrier before the transrectal procedure. This is a common phenomenon in boys, in whom, fortunately, serious prostate pathologies requiring detailed study are rare.
Risk factors
- Risk factors for the occurrence of pathology include:
- higher than normal estrogen levels;
- early onset of menstruation, their abundance, duration more than 8 days;
- surgical intervention on the uterus, appendages;
- abuse of bad habits;
- obesity;
- immune dysfunction;
- chronic stress, nervous overload;
- unfavorable environmental conditions;
- genetic predisposition;
- history of abortions.
Indications
Ultrasound of the reproductive organs should be part of the annual preventive medical examination for all men over 40 years of age, since at this age the risk of typical male diseases increases, in particular such as prostate adenoma and prostatitis.
Ultrasound examination of the scrotum is prescribed for boys with:
- failure of one or both testicles to descend from the abdominal cavity;
- dropsy;
- very early (before 11 years) or late (after 15 years) puberty;
- deviations in tests for male sex hormones.
Adult men require a similar ultrasound for:
- enlargement of one testicle relative to the other;
- changes in the shape of the scrotum;
- the presence of seals in it;
- pain and discomfort.
An ultrasound examination of the prostate is necessary if the following symptoms appear:
- frequent urination;
- difficulty urinating, pain during it;
- bloody impurities in the urine, bleeding from the urethra;
- pain in the lower abdomen, radiating to the groin and lower back;
- decreased potency.
Diagnostics

If you have characteristic symptoms, you should contact a gynecologist who will diagnose and treat the pathology. To confirm the diagnosis, a referral is given for a comprehensive examination, the results of which will help determine further tactics for managing the patient.
Bimanual examination
During a bimanual examination, one hand of the doctor is placed on the stomach, the other is inserted into the vagina. The procedure allows you to determine the increase in the size of the uterus, poor mobility, which is the result of the process of formation of adhesions.
Inspection in the mirrors
A gynecological examination in the speculum will provide the specialist with information about the presence of endometriotic lesions in the vagina and on the surface of the vaginal cervix.
Ultrasound diagnostics
Ultrasound examination of the pelvic organs is an accessible, effective, safe, painless diagnostic method, which, if adenomyosis is suspected, is recommended to be performed over time on days 8–10 and 20–24 of the cycle. The procedure will help determine the degree of pathological changes in the structure of the reproductive organ. At stage 1 of adenomyosis, the uterus on ultrasound is slightly enlarged in size, and in the projection of the walls, small cystic formations with a diameter of up to 2 - 3 mm are determined. The presence of cystic inclusions makes the structure of the myometrium heterogeneous, its echogenicity is slightly increased.
At stages 2–3, endometrial cells spread to the muscle tissue towards the serous layer, which indicates a diffuse form of pathology, which is characterized by the following signs:
- heterogeneous structure of the organ;
- uneven wall thickness;
- linear striation of the median M-echo, blurring of its contours;
- increase in organ size.
Ultrasound picture in Doppler mode
To assess the condition and functionality of the uterine vessels during ultrasound, color Doppler mode is used. This type of scan allows the doctor to see blood flow and detect signs of adenomyosis.
If the walls of the uterus are damaged by pathological endometrial cells, Doppler ultrasound can detect a slight increase in vascular resistance and increased blood flow in areas affected by the disease.
Possible diagnostic errors

Errors in ultrasound diagnosis of uterine adenomyosis occur quite rarely, but still they are not excluded, because the signs of the disease often coincide with the clinical picture of other diseases. For example, myomatous nodes can be confused with overgrown endometrial tissues, which are located in unusual places. Specific bending of the feeding vessels around the formation in color or power Doppler mapping mode will help to distinguish myomatous nodes.
The nodular form of adenomyosis can be confused with uterine sarcoma, but the malignant neoplasm is characterized by characteristic hypervascularization in the CD mode with a low-resistant type of blood flow. An ultrasound doctor conducting an examination of a patient with suspected adenomyosis must be able to recognize the clinical signs of all existing gynecological pathologies and have comprehensive information about the echographic picture of each. This will help to avoid mistakes and inaccuracies in making a diagnosis, and also to prevent the development of serious complications associated with the lack of timely treatment.
To whom is it assigned?
When comparing the results of transperineal ultrasound access with transabdominal access and data from other diagnostic methods, its reliability and high sensitivity have been proven. This study must be carried out as prescribed by specialized specialists: urologist, gastroenterologist, surgeon, endocrinologist, neurologist.
Indications for the study are:
- violation of the act of defecation of any kind (constipation, constipation-associated fecal incontinence in the presence of constipation, constipation unassociated fecal incontinence, i.e. without stool retention);
- the knot can help in assessing the condition of the intestinal tube, complications of colitis, the ultrasound method is especially intensively used as a control at the stages of complex and long-term treatment;
- violation of the act of urination of any kind (stress, urgency, daytime, nighttime incontinence, constant incontinence, mixed incontinence, when laughing and crying, dripping, dripping after urination);
- various diseases of the prostate gland;
- various endocrine-genetic diseases (sex formation disorders);
- mixed testicular dysgenesis;
- syndrome of incomplete form of testicular feminization;
- vestigial testicular syndrome;
- gonadal dysgenesis, etc.
The developed method of transperineal ultrasound examination makes it possible to identify malformations of the organs of the reproductive system in patients, starting from the neonatal period and dysfunctional pelvic disorders in the older age group. Its use before, during and after urination contributes to the study of the features of the anatomical structure and functional state of abnormally formed genital organs and reduces the indications for the use of such invasive methods as voiding cystourethrography, endoscopy of the genital ducts and diagnostic laparotomy.