When and how to donate blood for HPV
The abbreviation HPV stands for human papillomavirus.
It is he who is responsible for the appearance of papillomas, or, in simple terms, warts. These tumors can be very dangerous, and it is quite easy to become infected with the virus. Therefore, it is important to know how the human papillomavirus test is taken and where it can be done. HPV is transmitted through sexual and domestic contact, as well as during childbirth. You can become infected with it even through a kiss (albeit, if there is damage to the lips or mucous membranes). Failure to comply with hygiene rules in public places (baths, saunas, toilets), as well as using someone else's dishes, towels or toothbrushes can also cause infection. As you can see, it is not difficult to get the virus, and therefore everyone should know how to test for the human papillomavirus.
There are several ways to get tested for HPV:
- cytological method (examination of a smear under a microscope for the presence of koilocytes and dyskeratocytes);
- histological examination of a tissue sample for the presence of modified cells affected by the virus;
- detection of antibodies to the virus in the blood - this analysis method allows you to diagnose HPV in the early stages, however, it cannot be used to accurately determine the type of virus (and there are over 100 of them) and determine its concentration;
- Digene test, which allows you to accurately determine the type of virus, its concentration and oncogenicity;
- PCR, based on the detection of viral DNA, is highly accurate.
Symptoms and first signs of the disease
Even after entering the human body, human papilloma viruses may not manifest themselves at first. When immunity decreases, the virus is activated and begins to multiply. At this stage, clinical manifestations appear.
When infected with HPV of low oncogenic risk, patients are most often concerned about visual discomfort associated with the appearance of warts on any part of the skin and mucous membranes. These formations in the anogenital area have a special name - genital warts or anogenital warts. They are often accompanied by itchy skin. As a rule, these formations are of various shades of brown, have an uneven surface, and may be on a narrow base (leg).

Appearance of skin warts
A distinctive feature of warts and condylomas is rapid and multicentric growth. The presence of single warts on the skin and mucous membranes is an indirect sign of HPV infection and requires diagnosis.
Most infections caused by highly oncogenic types of HPV are asymptomatic. Only a general decrease in immunity is possible. Often the virus can only be detected after swab collection. However, the prolonged presence of an oncogenic type of virus leads to the development of precancerous pathologies, which, without appropriate therapy, degenerate into a malignant process. It is well known that in the early stages of the disease, cervical cancer is practically asymptomatic, and specific manifestations (discharge and irregular bleeding, pain in the back, pelvis, legs; unilateral swelling of the legs) occur when the process is widespread.
Viruses of high oncogenic risk - HPV 16, 18, 31, 33, 39, 50, 59, 64, 68, 70. The most studied and aggressive are types 16 and 18; these HPVs in women cause up to 70% of all cases of precancerous conditions and cervical cancer.
Clinical picture
It is believed that the incubation period before the clinical manifestation of HPV-associated diseases can be 1-8 months. Condylomas are exophytic formations, sometimes resembling cauliflower, on the skin, perineal and perianal mucosa, as well as on the mucous membranes. They can be multiple, asymmetrical and polymorphic. It is possible to change the size and number of genital warts, often resulting in the disappearance of the rash. In women, HPV most often affects the cervix, vagina, vulva and perianal area.
The classification of HPV-associated diseases is presented as follows:
- changes in the squamous epithelium of low malignancy (anogenital condylomas of the cervix, mild dysplasia);
- changes in the squamous epithelium of a high degree of malignancy (moderate and severe dysplasia and cancer);
- invasive cancer.
Subjective symptoms of HPV infection of the genitals and anal canal are usually absent. Characterized by a rapid increase in the size and number of genital warts, especially during pregnancy. Occasionally, patient problems such as bleeding, discharge and itching in the affected areas are identified.
Diagnosis of HPV in women
The polymerase chain reaction method, the so-called PCR, can reliably identify a specific type of papilloma virus. For analysis, a vaginal smear into a test tube with a special medium is sufficient. PCR is a simple but highly sensitive method.
A positive test for HPV 16 and 18 is associated with a higher risk of malignancy.

Eppendorf tube for collecting material for HPV testing
It is important to understand that changes in the cervix are often not visible to the naked eye, so it is necessary to use special additional examination methods, such as colposcopy and smears from the cervix and cervical canal.
Colposcopy is an examination of the cervical mucosa using a special device - a colposcope.
In this case, 2 tests are carried out:
- Acetic Acid Test - test with acetic acid solution
- Schiller's test - treatment of the surface of the cervix with Lugol's iodine solution.
Based on the data obtained, a satisfactory or unsatisfactory colposcopic picture is judged. This test is performed using a special Papanicolaou stain, which is why it is often referred to as a PAP test.
Detection of a pathological type of smear and an unsatisfactory colposcopic picture are indications for a biopsy of suspicious lesions.
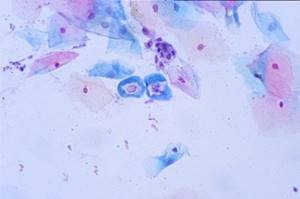
Pap smear staining
HPV: methods of infection, symptoms, oncogenic types of virus
Main methods of infection:
- vaginal, oral, anal sex with a person infected with HPV;
- during skin-to-skin contact with a person infected with papillomavirus, or contact with surfaces touched by an infected person - household infection is possible if there are cuts, abrasions, or other damage to the skin;
- during childbirth - from mother to child.
Recent studies by American and European scientists have shown that there is a high probability of HPV infection in medical institutions - through blood transfusion, use of medical equipment, inhalation of viral particles, for example, during laser ablation or electrocoagulation of condylomas.
The difficulty of combating non-sexual forms of infection is that the virus is extremely resistant to most disinfectants. HPV is the first virus to be insensitive to inactivation (treatment) with glutaraldehyde (a means for sterilizing surgical instruments that require absolute cleanliness). Doctors and technologists are faced with the problem of disinfecting devices that cannot be autoclaved and exposed to aggressive chemical compounds.
Prevention and treatment
The issue of preventing human papillomavirus is currently being actively discussed.
Patients often ask, is there a vaccine for cervical cancer?
In fact, there is no such vaccine. There is no treatment for the papilloma virus that would completely remove the virus from the human body. Only the result of the virus’s impact on the body’s cells can be treated. Regimen containing antiviral drugs and immunomodulators are used. The papillomas themselves can be removed surgically: by radio wave techniques, laser coagulation, and also by methods of chemical destruction.
All these types of therapy are actively used on the basis of the National Medical Research Center for Oncology named after N.N. Petrova after a thorough examination, examination and individual selection of treatment by highly qualified specialists. Undergoing therapy in a non-specialized institution may result in the spread of the virus to surrounding tissues damaged during the removal of the affected areas.
How is HPV treated?
Currently, there is no 100% cure for HPV. The only way to protect against the virus is vaccination, carried out at the age of 9-12 years. The Cervarix and Gardasil vaccinations protect against sexually transmitted strains 6 and 11.
The drug is administered intramuscularly three times, and during this time the body produces antibodies to the virus. Despite the high price, vaccination will significantly reduce the risk of developing the cervix in girls whose family members have had cases of cancer of the reproductive organs.
The main method of treating papillomas is complex, combining surgical removal of skin tumors and increasing immunity. The most effective and painless method for the patient is the radio wave method. It is performed under local anesthesia. The tumor is removed by a high-frequency radio wave, cutting off exclusively the area affected by papilloma.
Self-removal of papillomas at home is not recommended, despite the sale of various products such as celandine in pharmacies. This is delicate work that cannot be done independently. As a result, skin burns and rapid relapse.
HPV treatment in St. Petersburg
At the Diana clinic, the doctor will prescribe the necessary tests and identify the exact cause of the relapse. Perhaps HPV manifested itself due to hidden hormonal disorders or the development of another disease that the patient was not previously aware of.
When treating papillomavirus in our clinic, you will receive specialist advice on further strengthening your immune system. This will help prevent dangerous complications from HPV.
The specialist will give an accurate answer whether the patient is at risk of malignant neoplasms. For this reason, you should definitely undergo an examination and consult a doctor, even if papillomas do not cause any concern.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Vaccines against human papillomavirus
There are currently 2 recommended vaccines in use. It is considered optimal to vaccinate girls before they become sexually active.
Since 2006, the Gardasil vaccine has been used (Fig. 4). This is a quadrivalent vaccine, i.e. it is directed against HPV types 6, 11, 16 and 18.
The recommended course of vaccination consists of 3 doses and is carried out according to the following scheme: first dose - on the appointed day; the second - 2 months after the first; the third - 6 months after the first. Carrying out the full course leads to the formation of stable immunity in 99% of vaccinated people for a period of at least 36 months in all age groups. Children and adolescents, as well as young women aged 9 to 26 years, are subject to vaccination.
Another vaccine is Cervarix. Created in 2007 for the prevention of diseases caused by human papilloma viruses types 16 and 18. A full course of vaccination according to the 0–1–6 month schedule leads to the formation of specific immunity in 100% of vaccinated individuals 18 months after the last dose of the vaccine in age groups from 10 to 25 years. The need for revaccination has not yet been established.

Vaccines against human papillomavirus a) Gardasil b) Cervarix
In a number of regions of the Russian Federation, patients are vaccinated free of charge, while in others vaccination is carried out on a commercial basis.
Suspected risk factors for cervical cancer:
- smoking (including passive smoking);
- long-term use of oral contraceptives (more than 5 years);
- a large number of pregnancies;
- other STIs (caused by Chlamydia trachomatis, herpes simplex virus type 2, HIV);
- poor nutrition (especially those with low amounts of antioxidants in the diet);
- immunodeficiency (AIDS, organ transplantation, immunosuppressive therapy);
- a large number of sexual partners, early onset of sexual activity, sexual contacts with persons infected with HPV;
- genetic predisposition: polymorphism of some genes that encode proteins that regulate the cell cycle.
Secondary prevention of HPV infection includes screening the population in order to detect the disease at the precancer stage and its timely treatment.
Previous post When do the first signs of pregnancy appear?
Next entry How to calculate the calorie range
Dynamic observation
Today, cervical cancer screening in the Russian Federation is regulated by Order No. 572n of the Ministry of Health: preventive examinations with cytological screening are carried out at least once a year. PCR testing of vaginal discharge for the presence of human papillomavirus is not prescribed as part of a preventive medical examination. However, according to international standards, HPV detection is an important and integral factor in the prognosis of cervical diseases. Initial HPV testing is recommended, as is cytological screening of the cervical epithelium. The screening interval for patients with a normal cytology test result and a negative HPV test ranges from 1 to 3 years.
Cost of testing for the presence of human papillomavirus infection at JSC "SZDCM"
The cost of testing for HPV infection depends on the type of study, coverage of virus strains, type determination/non-determination, and calculation of viral load.
Prices for types of research in the medical departments of JSC "SZDCM" represent various combinations in terms of coverage, detail, and prognostic value.
Your doctor - gynecologist, dermatologist, venereologist - will tell you which research method to choose. If you are getting tested on your own initiative, choose to test for oncogenic strains of HPV.
Types of HPV tests

In modern medicine there are several effective examinations for human papillomavirus. With their help, you can determine the presence of infection and find out the type of HPV. The patient is referred for testing for papillomavirus by the attending physician, a dermatologist, gynecologist or urologist.
The most common HPV tests are:
- colposcopy;
- histological diagnosis;
- cytological examination;
- amplification and non-amplification test;
- detection of antibodies to HPV.
Colposcopy is prescribed to women to detect papillomas localized in the cervix. Diagnosis is considered simple and is carried out using special equipment - a microscope. The doctor examines the mucous membrane of the vagina and cervix. Colposcopy allows you to examine organs at multiple magnification. The duration of the procedure varies from 10 to 30 minutes. The doctor hands over the results 10-15 minutes after the examination.
Histological diagnosis is almost always prescribed in conjunction with cytological tests. This test examines a small biopsy sample - a small piece of tissue. The biomaterial is placed under a microscope and the affected cells are assessed. Histological techniques allow one to determine whether a tumor is malignant or benign. The duration of the manipulation takes no more than 15 minutes. The patient can receive the results 2-3 days after the examination. Most often, after histology, the patient is sent for a non-amplification test or PCR study.
To conduct a cytological examination, the doctor collects biomaterial. A smear of skin cells is taken as a sample. The resulting material is examined under a microscope. With this analysis, you can see modified cells and tissues that indicate HPV. The technique is simple and not expensive, but at the same time it quite often shows a false negative result. The result form is given to the patient after 4-6 days.
The amplification test in modern traditional medicine is considered accurate because it shows the type of infection and its oncogenicity. The sample is taken from the urinary canal or vaginal mucosa. This analysis is often prescribed by a gynecologist in conjunction with cytological diagnostics.
PCR analysis is used to determine the oncogenicity of a growth or papilloma. The biomaterial is urine, blood plasma, a smear from the mucous surface or amniotic fluid. The accuracy of the survey is close to one hundred percent. Human papillomavirus can be detected even with a small concentration of infection in the blood. With the correct collection of biomaterial and accurate interpretation of the results, it is possible to know for sure whether there is HPV or not just 1-2 days after the manipulation.
Some patients are surprised when the test result is “positive”, but there are no condylomas on the body. This indicates that there is an infection in the body, but the immune system is restraining it in every possible way. Doctors recommend that if the result is “positive,” you undergo a course of treatment, and if there are papillomas, remove them using a laser or other methods.
Indications for prescribing HPV testing
The appearance of warts, condylomas, papillomas and growths on the skin are primary indications that may indicate HPV in the body and require prompt examination. After examining and finding neoplasms of unknown etiology on the body, a dermatologist refers the patient for diagnosis and blood donation for human papillomavirus. It is very important to determine the type of infection, since some of them are considered completely harmless, while others are considered deadly.
An important indication for taking the test is planning a pregnancy. You also need to undergo an examination to identify female and male infertility, pathological processes in the body, and miscarriages. Both partners should be examined, since the infection is transmitted through sexual intercourse.
Preparation for the procedure
It is advisable to conduct examinations of women in the first half of the menstrual cycle, but not earlier than the 5th day.
Examination in the second half of the cycle is acceptable, but no later than 5 days before the expected start of menstruation. If there are pathological changes, material is taken on the day of treatment.
The day before and on the day of the examination, the patient is not recommended to douche the vagina. Biomaterial collection should not be carried out earlier than 24-48 hours after sexual intercourse, intravaginal ultrasound and colposcopy.
A scraping from the urethra is carried out before or 2-3 hours after urination.
Men need to avoid sexual intercourse 1–2 days before taking a smear (scraping). You cannot urinate for 1.5-2 hours before the procedure.