Eosinophils consist of a bilobed nucleus and three types of eosinophil granules (lipid bodies, eosinophils, small and primary). They contain protein structures with the help of which foreign cells are neutralized. Eosinophils are quite large cells: their diameter reaches 20 microns.
Eosinophils got their name due to the fact that when stained according to Romanovsky, they are easily stained with eosin (an acidic dye), while other types of dyes have no effect on them. Eosin itself was invented in 1873 by the German scientist G. Caro and, due to its bright pink color, was named after the ancient Greek goddess of the dawn Eos (in the German version the name sounds like “eosin”).
Blood test for eosinophils
To determine the level of eosinophils, a general blood test is used, which is familiar to all of us since childhood. Eosinophils by themselves do not give an accurate idea of the nature of pathological changes in the body, however, in combination with other values of the leukocyte formula, they allow a specialist to judge the nature of the pathology. In the analysis form, eosinophils are designated as EO. Their content is indicated as a percentage of the total number of leukocytes. A formula is also used to calculate the absolute number of eosinophils in peripheral blood and it looks like this: number of leukocytes * 10 to the 9th power. For a general analysis, blood is most often taken from a finger prick, but venous blood is also suitable.
Figure 1. Causes of eosinophilia (increased number of eosinophils in the blood). Image: kavusta/Depositphotos
Indications for analysis
A complete blood test with a count of eosinophils is prescribed for most people who visit the clinic. The range of indications is very wide, but in modern clinical practice, the initial eosinophil count is most often used as a biomarker to assess the effectiveness of drugs prescribed to patients with bronchial asthma. In this regard, the absolute number of eosinophils is of greatest value to the physician.
Eosinophils belong to microphages. This means that they can only absorb small foreign particles.
The study is relevant when confirming a preliminary diagnosis, checking the effectiveness of the prescribed therapeutic course, assessing the state of a person’s health during medical examinations or medical examinations. The doctor also prescribes a general blood test in the postoperative period. In addition, counting eosinophils is important when the development of infectious, oncological and autoimmune diseases is suspected.
Diagnostics
Eosinopenia has a fairly wide range of etiological factors, so if it is detected, you should consult a general practitioner. When collecting anamnesis, it is necessary to clarify whether the patient is taking medications and whether he is registered at a dispensary for a chronic disease. It is also necessary to find out whether the patient has traveled abroad over the past few months, or eaten insufficiently processed meat or fish, unwashed vegetables or fruits.
Much attention is paid to examining the patient. Thus, skin rashes in the form of urticaria indicate the presence of allergies, centripital obesity, stretch marks on the lateral surfaces of the abdomen are characteristic of hypercortisolism. If COVID-19 is suspected, body temperature and saturation are measured, and lung auscultation is performed. It is clarified whether there is a dry cough, difficulty breathing, loss of smell and taste. Additional research methods are prescribed, including:
- General blood analysis.
Patients with coronavirus infection often experience lymphopenia; with purulent infections, general leukocytosis and an increase in ESR are detected; helminthic infestations are characterized by a decrease in hemoglobin levels. - Blood chemistry.
With helminthiasis, a deficiency of iron and ferritin is detected; for patients with hypercortisolism, a high concentration of glucose is typical. - Parasitological studies.
Using various processing methods (sedimentation, enrichment), microscopic examination of feces for helminth eggs is carried out. - Allergological research.
The allergic nature of the disease is confirmed by the high content of immunoglobulin E. The presence of hypersensitivity to certain types of allergens is determined by skin tests, prick tests, and the detection of specific immunoglobulins in the blood. - Hormonal studies.
There are 3 tests for diagnosing hypercortisolism - determination of cortisol in saliva, in daily urine, and also in blood serum after taking tableted dexamethasone (small dexamethasone test). To differentiate the syndrome from Cushing's disease, a large dexamethasone test is performed. - Pathogen identification.
If COVID-19 is suspected, immunoglobulin M is determined in the blood using ELISA or the express method (immunochromatography). An accurate diagnosis can be determined by the presence of viral RNA by PCR of materials from the pharynx and nasopharynx. - CT, MRI.
In patients with Cushing's syndrome, an abdominal CT scan reveals an adrenal tumor. In Itsenko-Cushing's disease, a pituitary adenoma is found on MRI of the brain.

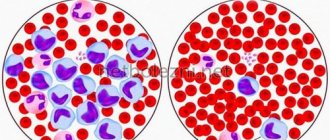
Eosinophil count
Norms of eosinophils in the blood
When deciphering the analysis, the patient’s age is taken into account, since these factors affect the content of eosinophils in the blood.
Table 1. Norm of eosinophils by age
| Children under 5 years old | Children 5 – 14 years old | Adults |
| 0,5 – 7% | 1 – 5% | 0,5 – 5% |
It should also be taken into account that in women in the first days of menstruation there is a slight excess of the norm in the content of eosinophils, while after ovulation their number may be slightly below the norm.
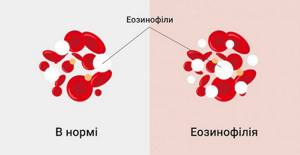
In absolute terms, the norm for adults is 0.15-0.450X10.0⁹ per liter of blood plasma. Exceeding the normal percentage of leukocytes is called eosinophilia. There are three stages of eosinophilia:
1. Light (no more than 10% of the total number of leukocytes).
2. Average (up to 15%).
3. Heavy (over 15%).
Causes of an increased number of eosinophils in the blood
An increase in the level of eosinophils indicates that the body is resisting the inflammatory process, and tissues and cells are experiencing oxygen deficiency. Possible reasons for the increase in the number of eosinophils:
- Allergy. This is one of the most common reasons. Hypersensitivity reactions always increase the production of eosinophils in the bone marrow. In turn, eosinophils reduce the production of allergy mediators.
Allergies are a common cause of elevated eosinophil levels. Photo: Dmyrto_Z / Depositphotos
- Asthma. In bronchial asthma, there is a moderate increase in the number of eosinophils in the blood, and in the allergic form they can also be found in sputum and bronchoalveolar fluid.
- Helminthic infestations. When infected with helminths, the number of eosinophils in the blood increases for two reasons: first, they release eosinophil cationic protein and reactive oxygen species to kill parasites. Secondly, the metabolic products of parasites provoke hypersensitivity reactions, and here the mechanism for increasing the production of eosinophils is the same as in allergies.
- Lung diseases. Despite the fact that the mechanism of increased eosinophil production in lung diseases has not yet been fully studied, experts note the relationship between these phenomena. Eosinophilia is observed in Churg-Strauss syndrome (in this case it reaches a frightening figure of 50%), allergic bronchopulmonary aspergillosis (an increase in the level of eosinophils is observed only in the acute phase and rarely exceeds 15%), as well as in eosinophilic pneumonia (up to 20%).
- Blood diseases. First of all, we are talking about hematological pathologies of a malignant nature (eosinophilic leukemia, myeloid leukemia). Eosinophilia is also characteristic of mastocytosis, but in leukemia its severity is much higher (up to 70%).
- Gastrointestinal diseases. An increased number of eosinophils in a general blood test is observed in gastritis, esophagitis and enterocolitis. All these diseases are accompanied by inflammatory processes, which causes accelerated formation of eosinophils.
- Oncological diseases. When confirming the diagnosis, the leukocyte count is not a priority indicator, but an increase in the number of eosinophils in malignant diseases is indeed observed. After therapeutic interventions such as radiotherapy, the increase in the number of eosinophils also increases significantly.
- Weakened immunity. In immunodeficiency conditions (Wiskott-Aldrich syndrome and Jobe syndrome), the level of eosinophils can reach 60%, which is associated with increased production of immunoglobulin E.
- Endocrine diseases. In diseases such as primary adrenal insufficiency (Addison's disease), congenital adrenal dysfunction, Schmidt's syndrome and panhypopituitarism, eosinophil levels increase to moderate levels and normalize after treatment with glucocorticoids.
- The recovery period after surgery. This is especially true when transplanting donor organs to a patient and removing the spleen.
Correction
Conservative therapy
Patient management tactics depend on the etiology of eosinopenia and the severity of the patient’s condition. Eosinopenia in itself does not have a negative effect on the body. Therefore, if it develops during the use of GCS, their withdrawal is not required. For neurotic disorders, it is necessary to consult a psychotherapist who conducts psychotherapy sessions and prescribes pharmacological drugs (antidepressants, tranquilizers).
People with allergies are advised to avoid contact with the allergen. If COVID-19 is confirmed, in order to prevent the spread of coronavirus infection, patients are moved to an infectious disease isolation ward. In severe bilateral pneumonia with respiratory failure (saturation below 90%), connection to a ventilator is indicated.
The following medications are used to treat conditions that can cause eosinopenia:
- Antihistamines.
To relieve allergy symptoms, drugs are used that block histamine receptors, the main mediator of allergic reactions. - Bronchodilators.
To relieve an attack of bronchial asthma, inhalers containing beta-2-adrenergic receptor agonists and cholinergic receptor blockers are prescribed. - Inhaled glucocorticoids.
As a basic therapy that suppresses the inflammatory process in the bronchi, GCS in the form of inhalations are very effective. - Anthelmintic drugs.
These drugs disrupt the function of the neuromuscular system of helminths, thereby causing their paralysis and death. - Antibiotics.
For purulent processes, broad-spectrum antibacterial drugs are prescribed - cephalosporins, penicillins. - Steroidogenesis blockers.
Inhibitors of cortisol synthesis or glucocorticoid receptor blockers are used in preparation for surgical treatment of Cushing's disease or syndrome to reduce the concentration of cortisol in the blood. - Immunobiological drugs.
To reduce the severity of the cytokine storm in patients with COVID-19, monoclonal antibodies, Janus kinase inhibitors, and intravenous administration of human immunoglobulin are used.
It is worth paying attention to the fact that none of the many antiviral drugs recommended by many experts has demonstrated a positive effect in the treatment of a new coronavirus infection. Also ineffective were drugs prescribed to suppress the inflammatory process in the lungs - synthetic antimalarials and macrolide antibiotics.
Surgery
Patients with Itsenko-Cushing's disease are indicated for neurosurgical surgery - transsphenoidal adenomectomy. For Itsenko-Cushing syndrome, laparoscopic bilateral adrenalectomy is performed, followed by hormonal replacement therapy with glucocorticoids and mineralocorticoids. An hydatid cyst, which is most often localized in the liver, also needs to be surgically removed.
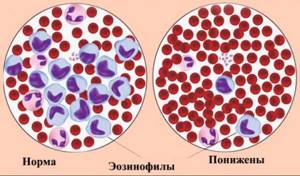
Causes of a low number of eosinophils in the blood
A decrease in the number of eosinophils below 0.02*109/l is called eosinopenia. There are several possible reasons:
- Taking glucocorticoids and steroids. These are hormonal drugs that help reduce the number of leukocytes (including eosinophils) in the blood due to their destruction. At the same time, eosinopenia is not a strong enough reason to discontinue a course of glucocorticoids, since in itself it does not pose a threat to health, while the therapeutic effect of these drugs for allergic reactions or autoimmune diseases fully justifies their use.
- Nervous tension and stress. During times of severe mental stress, depression and emotional turmoil, the level of cortisol, which is called the stress hormone, increases in the blood. It is cortisol that destroys eosinophils.
- Allergic reactions. The level of eosinophils in allergies is a rather paradoxical issue. With moderate hypersensitivity reactions, eosinophilia is observed, but with severe allergies, the level of eosinophils, on the contrary, decreases.
- Infectious diseases. Eosinopenia is characteristic of diseases of a viral and bacterial nature, which include coronavirus infection. A decrease in the number of eosinophils is also observed in purulent-septic processes (abscesses and phlegmon).
- Endocrine diseases. As we already know, an increase in the level of cortisol in the blood entails a decrease in the number of eosinophils. Cortisol is produced in the adrenal glands, so adrenal diseases (for example, Cushing's syndrome) cause eosinopenia.
- Bone marrow diseases. Since eosinophils are formed in the bone marrow, any associated pathologies and injuries cause eosinopenia.
- A decrease in the level of eosinophils in the blood can also be observed in the first days after a heart attack, with appendicitis, sepsis, acromegaly, lupus erythematosus, burns and injuries.
Figure 2. Eosinopenia (low eosinophil count). Dr Graham Beards / Wikipedia (CC BY-SA 3.0)
Causes of eosinopenia
Taking hormonal medications
One of the most common causes of eosinopenia is long-term use of adrenal hormones - glucocorticosteroids.
Glucocorticoids have the ability to reduce the number of leukocytes, including eosinophils, in peripheral blood by directly destroying them. Therefore, people taking corticosteroids may experience eosinopenia, often due to a decrease in the total number of white blood cells (leukopenia). The presence of eosinopenia in itself is not considered a reason to discontinue hormonal therapy, since it does not have a pathological effect on human health. Glucocorticoids are widely used in clinical practice to treat a wide variety of pathologies, such as:
- Allergic reactions
: bronchial asthma, Quincke's edema. - Rheumatological pathologies
: ankylosing spondylitis, diffuse connective tissue diseases (systemic scleroderma, systemic lupus erythematosus), inflammatory bowel diseases (ulcerative colitis, Crohn's disease). - Autoimmune disorders
: glomerulonephritis, autoimmune hemolytic anemia, psoriasis.
Emotional stress
Severe emotional stress tends to stimulate the adrenal glands to produce large amounts of cortisol, which can destroy eosinophils. Eosinopenia can be observed both in healthy people under the influence of significant stress, and in various neuroses - social anxiety disorders, depression, neurasthenia. After eliminating the traumatic factor, conducting psychotherapy, prescribing anti-anxiety medications, antidepressants, the level of eosinophils returns to normal.
Allergic reactions
As a rule, allergic reactions are accompanied by eosinophilia, i.e. an increase in the number of eosinophils. However, with severe allergic inflammation, on the contrary, the level of eosinophils in the blood decreases. The pathogenesis of this phenomenon is as follows: an allergen that has entered the body causes degranulation of basophils and the release of allergy mediators (histamine, leukotrienes, etc.), as well as the eosinophil chemotactic factor (ECF) of anaphylaxis. This factor stimulates the migration of eosinophils from the peripheral blood to the site of inflammation.
With massive degranulation of basophils, a large amount of ECP is released, as a result of which almost all eosinophils in the peripheral blood migrate to the site of inflammation to suppress it, and new eosinophils do not yet have time to be synthesized in the bone marrow. Therefore, in the first hours after an attack of a severe allergic reaction (status asthmaticus, angioedema, anaphylactic shock), patients may experience eosinopenia, and sometimes aneosinophilia (complete absence of eosinophils).
Eosinopenia
Worm infestations
As is known, helminths are capable of inducing hypersensitivity reactions that occur within a few weeks after infection. Eosinopenia can develop according to the mechanism described above (massive migration of eosinophils to the site of allergy). It is worth noting that eosinopenia in patients with helminth infections is extremely rare, and the overwhelming majority of patients have very high eosinophilia (can reach 60-70% of the total number of leukocytes).
- Nematodes
(caused by roundworms): ascariasis, toxocariasis, trichinosis. - Cestodoses
(caused by tapeworms): diphyllobothriasis, teniarinchiasis, cysticercosis. - Trematodes
(caused by flatworms)
:
opisthorchiasis, clonorchiasis.
Viral and bacterial infections
Eosinopenia may accompany some infectious diseases. Of these, the most relevant today is COVID-19. The mechanism of eosinopenia caused by coronavirus infection caused by SARS-CoV-2 is unknown. However, according to clinical observations, eosinopenia that develops in patients with COVID-19 is associated with severe pneumonia.
In such patients, there is an increased need for respiratory support (connection to mechanical ventilation) and a high incidence of deaths. Also, a low content of eosinophils is considered a marker of an unfavorable outcome in purulent-septic processes - phlegmon, abscesses.
Hypercortisolism
Since glucocorticoids can have a destructive effect on eosinophils, a constant elevated level of adrenal hormones (cortisol) in the blood is often accompanied by eosinopenia. Such endocrine pathologies include Cushing's disease (a pituitary adenoma that secretes excess adrenocorticotropic hormone) and Cushing's syndrome (adrenal corticosteroma that secretes large amounts of cortisol). Eosinopenia is detected already in the early stages of the disease and is leveled after eliminating hypercortisolism.
Consequences of deviation from the norm
A change in the normal level of eosinophils in the blood is not a criterion by which one can get an idea of possible pathological changes in the body. Simply put, the level of eosinophils in the blood itself means little - you need to pay attention to the disease that caused its change. Therefore, the consequences can be very diverse - from completely insignificant (as in the case of physical activity) to deadly (for example, in the case of oncology).
Eosinophilia itself, in rare cases, can lead to damage to tissues in which the greatest accumulation of eosinophils is observed. The mechanism of such damage has not been fully studied to date, but it has been established that eosinophils exhibit the most severe damaging effect in conditions such as eosinophilic fibroplastic endocarditis and idiopathic hypereosinophilic syndrome. The nature of the damage directly depends on the duration of eosinophilia and the severity of eosinophilic tissue infiltration.
How to reduce the number of eosinophils in the blood
Eosinophilia is not an independent nosological entity, but only a consequence of a particular disease. Therefore, it cannot be treated in isolation - first of all, it is important to eliminate the cause of its occurrence, that is, the disease that caused the change in the leukocyte formula.
Possible treatment options:
- Desensitizing therapy. For allergies, antihistamines are used to reduce hypersensitivity reactions. Some of them may cause mild drowsiness (for example, chloropyramine), but newer generation drugs such as cetirizine, levocetirizine, desloratadine and rupatadine do not have this side effect and have a mild anti-inflammatory effect.
- Antibacterial therapy - for infectious diseases, antibiotics are prescribed (amoxicillin, ceftriaxone, azithromycin, erythromycin, etc.). The choice of antibacterial drug depends on the pathogen and its sensitivity to a specific group of antibiotics.
- Anti-inflammatory therapy. An increase in the level of leukocytes (including eosinophils) is observed during inflammatory processes. When they are severe, glucocorticosteroids (prednisolone) are used.
- Chemotherapy. This treatment method is aimed at eliminating malignant tumors. For this purpose, cytostatics and antimetabolites are used.
- Hormonal therapy. For multisystem diseases accompanied by immunodeficiency (for example, Jobe's syndrome), the use of steroid drugs and interferon gamma is indicated. Treatment is supplemented with antibiotics, calcineurin inhibitors, H1-histamine blockers, and antifungal drugs.
- Antihelminthic therapy. To combat helminthic infestations, drugs such as albendazole, levamisole, bephenia hydroxynaphthoate, piperazine, tetrachlorethylene, and mebendazole are prescribed. The choice of medication depends on the type of parasite and the stage of infestation. Additionally, antibiotics, enterosorbents, enzymes, probiotics, and glucocorticoids are prescribed.
Additionally, the following measures can be taken:
- Normalize your lifestyle. It is important to avoid frequent drinking of alcohol and give up cigarettes (or at least significantly limit the number of them).
- Avoid chronic intoxication. In people working in hazardous industries or living in environmentally unfavorable regions, the number of eosinophils in the blood increases as a result of constant chemical intoxication.
- Maintain a healthy diet. You should not overuse spicy, smoked, canned and fatty foods. To increase the level of eosinophils, you should limit the amount of meat, poultry and fish in your diet (consume mainly low-fat varieties). The menu should include yogurt, cheeses, vegetables, fruits, beans, bran and whole grain bread.
Giving up bad habits will help normalize the level of eosinophils. Photo: vgstockstudio / freepik.com
Etiology of eosinophilia
The reasons for the increase in eosinophil concentration are varied:
- allergic reactions;
- infection with worms and parasites;
- pulmonary pathologies - Loeffler's syndrome, eosinophilic pneumonia, allergic reaction to pulmonary forms of aspergillosis, pulmonary infiltrates with eosinophilia, Churg-Strauss syndrome (one of the systemic vasculitis), sarcoidosis;
- blood pathologies - pernicious anemia, polycythemia vera, non-Hodgkin's lymphoma, acute or chronic myeloid leukemia, as well as eosinophilic leukemia, Sezary syndrome;
- endocrinopathies;
- malignant tumors - carcinomatosis, adenocarcinoma of the gastrointestinal tract, urinary and reproductive systems, lungs and some other cancers;
- some benign tumors;
- primary immunodeficiencies - hyper-IgE syndrome (or Jobe syndrome), T-lymphopathies, Wiskott-Aldrich syndrome, neutrophil chemotaxis defect;
- tuberculosis;
- some dermatological pathologies;
- gastrointestinal pathologies;
- mixed conditions - magnesium deficiency, idiopathic eosinophilia, recovery period after infectious diseases, AIDS, chorea, congenital heart disease, scarlet fever, hypoxia, radiation, reaction to transplantation, condition after peritoneal dialysis, etc.;
- drug-induced eosinophilia caused by taking certain medications.
How to increase the number of eosinophils in the blood
A decrease in the level of eosinophils in the blood is a sign of weakened immunity. As in the case of eosinophilia, the primary pathology should be identified and eliminated, as well as lifestyle adjustments: minimize bad habits, ensure an adequate level of physical activity, and also take care of a normal daily routine (it is important to sleep at least 8 hours a day) .
The normalization of the leukocyte formula is facilitated by the consumption of vitamins B12, C, D. They can be obtained from food (meat, fish, cottage cheese, rose hips, currants, garlic), or from pharmacy multivitamins. It is advisable to exclude foods with a high allergenic potential: milk, soy, wheat, eggs, seafood, peanuts.
When treating diseases that result in eosinopenia, the same groups of drugs are often used as in the case of eosinophilia. For example, antibiotics are prescribed for infectious diseases, as well as diffuse and localized purulent-inflammatory processes (cellulitis and abscess). As mentioned earlier, allergies can provoke not only an increase, but also a decrease in the number of eosinophils in the blood, so antihistamines can also be used in the treatment of eosinopenia.