Research method
- PCR
HIV infection is an infectious disease caused by the human immunodeficiency virus (HIV).
It is characterized by a specific lesion of the immune system, leading to the formation of acquired immunodeficiency syndrome (AIDS). The human immunodeficiency virus is an RNA virus that belongs to the retrovirus family. There are two types of virus: HIV-1 and HIV-2. HIV-2 is much less common. The examination to detect HIV infection is carried out in accordance with the sanitary and epidemiological rules SP 3.1.5.2826-10 “Prevention of HIV infection”.
Determination of provirus DNA by PCR is indicated for examining children born to HIV-infected mothers (under the age of 18 months); other categories of patients in cases of questionable results of antibody determination by immunoblot and positive results of antibody determination by ELISA. HIV provirus DNA is present in the blood even in the case of an undetectable viral load (undetectable amount of HIV RNA).
Diagnosis of HIV infection Treatment of HIV infection (go)
The diagnosis of HIV infection is established by an infectious disease specialist at the AIDS Center through a comprehensive assessment of epidemiological data, clinical examination results and laboratory tests. The
first step and standard method for laboratory diagnosis of HIV infection is the simultaneous determination of antibodies to HIV 1, 2 and the HIV p25/24 antigen. The p24 antigen can be detected on the 15th month, the first antibodies - on the 30th, late - by 3-6 months.
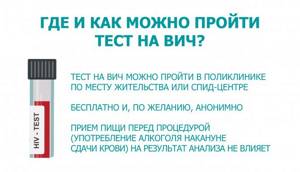
In the laboratory of the AIDS center you can take an HIV test to detect antibodies and antigens. The service is completely free for citizens of the Russian Federation, confidential and, at the request of the applicant, anonymous. The procedure is quite simple and consists of three stages: pre-test counseling (carried out at the request of the patient), collection of material for research, issuance of results and post-test counseling.
In addition to the standard HIV test, which involves drawing blood from a vein, there are rapid tests for HIV.
They can be performed using a drop of blood from a finger or saliva. Such tests are often focused on detecting antibodies. Rapid tests are used in test mobiles and at outreach campaigns for information, counseling and voluntary HIV testing.
This is the law: every HIV test using simple/rapid tests must be accompanied by a blood test using standard testing methods for HIV antibodies 1,2 and p24 antigen or by referring the patient for testing using standard methods.
Issuing a conclusion about the presence or absence of HIV infection only based on the results of a simple (quick) test is not allowed.
Laboratory diagnosis of HIV infection can be done both at an AIDS center and at a local clinic, antenatal clinic or dispensary, if you are registered there and undergo regular treatment.
An HIV test is the only way to find out whether you have the disease or not. HIV infection has no external specific signs or symptoms; if in the acute period (this is about a year from the moment of infection) some ailments appear, then they all proceed like diseases known to us, for example, a cold or sore throat.
It is important to remember that HIV infection has an incubation period. Those. The first antibodies can be detected after about a month from the moment of infection, and the later ones - after three. All this time, a person can transmit the virus to another, for example, through unprotected sex, and the HIV test may be negative (antibodies will not be detected).
This is why it is so important to get tested for HIV regularly. This will not only help stop the development of the disease, but will also protect other people from becoming infected.
Pre-test counseling - a conversation between the patient and a specialist - is carried out before taking an analysis (HIV test) and serves to:
— clarify and assess the risks of contracting HIV infection;
— update information about HIV, inform or correct misconceptions about the disease;
— talk about the analysis procedure
— discuss possible test results and prepare the patient for the test result.
The result of the consultation is informed voluntary consent to undergo the procedure - testing for HIV. It is completed in writing and confirms the patient's decision to undergo testing.

In what cases and how often should you take an HIV test?
If there is no risk of infection in your life, then you can take an HIV test once every 1-3 years, for example, during a medical examination. If you have had a risk, you must take an HIV test as soon as possible after the risk situation, and again after 3 months, i.e. after the end of the incubation window.
An HIV test can be either positive—antibodies to HIV and/or HIV antigen are detected—or negative—antibodies/antigen are not detected.
Negative
The result of an HIV antibody test is not absolute confirmation of the absence of the disease.
For several months after HIV infection (up to 3 months), the test result may be negative. This period is called the “seronegative window” or “incubation period”, we wrote about it above - the period between infection and the appearance of antibodies to HIV. It is important to remember: the results of the study are not communicated by phone, email, or SMS.
The result is issued upon personal application from the subject or his legal representative. After receiving a positive result using ELISA or CLIA, the next stage of diagnosis
diseases. To confirm the results regarding HIV, confirmatory tests are used (immune, linear blot and determination of HIV RNA/DNA by molecular biological methods).
Immune or line blot
are focused on identifying antibodies to HIV, but to specific glycoproteins of the virus. The molecular biological research method (PCR) allows you to identify the genetic material of HIV - RNA or DNA of the virus. At the diagnostic stage, qualitative analysis is used. Unlike quantitative, it shows only the presence or absence of HIV genetic material in a biological sample (blood), and not the number of viral particles.
Detection of HIV gene material is used in cases where the patient urgently needs to start taking medications, for example, if a newborn child is infected from the mother during pregnancy and/or childbirth, if a woman is pregnant and it is necessary to make a decision about starting the prevention of mother-to-child transmission of HIV. For example, if there is a high risk of HIV infection, the test is carried out in the first 48 hours of the child’s life and again at the age of 14 - 21 days. The HIV DNA detection method is predominantly used. Obtaining positive test results for HIV DNA or HIV RNA in two separate blood samples from a child at any age is laboratory confirmation of the diagnosis of HIV infection.
Testing for HIV antibodies in children born to HIV-positive mothers will give a positive result until approximately 18 months. This is due to the presence of maternal antibodies in the child’s blood.
If you have been diagnosed with HIV infection
, then the specialist is obliged to inform you about this during a personal visit. This is why it is so important to come back for your test results. Most often, the diagnosis is made by a specialist at the AIDS center. That is why in the medical organization where you took the test, the doctor can only tell you the result of the study and recommend that you contact the AIDS center for a diagnosis and registration for dispensary observation and treatment.
During the consultation, the specialist must inform you: - the result of the study - explain precautions to prevent the spread of HIV infection - explain the guarantees of receiving medical care and respect for rights and freedoms - warn about criminal liability for creating a threat of infection or for infecting another person with HIV -infection.
Epidemiologist
The AIDS center is obliged to conduct an investigation and clarify the source of infection. As well as the possible further spread of the virus. Therefore, a person with HIV will face questions regarding any situations related to the possibility of transmitting the virus: - contact with blood in medical and non-medical organizations - use of psychoactive substances - sexual contacts, etc.
Infectious disease physician
At your appointment, he will examine you and question you about the manifestations of acute HIV infection. In 30-50% of cases, people develop symptoms that resemble other diseases in the first year of infection.
After the diagnosis is established, the stage of the disease is clarified and treatment for HIV infection is prescribed.
When registering at a dispensary, all patients undergo a set of laboratory diagnostic tests to identify the following diseases:
syphilis (further every 12 months)
viral hepatitis C (further every 12 months)
viral hepatitis B (further every 12 months)
toxoplasmosis (Toxoplasma gondii)
cytomegalovirus (Cytomegalovirus)
tuberculosis (further every 6 months).
Origin of PCR analysis
The date of birth can be given as 1983. The method is based on isolating a fragment of a foreign nucleotide chain, it can be either ribonucleic acid or deoxyribonucleic acid, artificially propagating it and studying it. A PCR specialist takes HIV DNA and multiplies it according to the principle of complementarity, building a fairly long chain that is convenient to examine and test. HIV RNA PCR is carried out in the same way, only plasma or serum is taken.
The emergence of this approach in widespread practice was a real breakthrough and made it possible to take a big step in helping patients. Thus, it became possible to help people at the earliest stages, to detect the disease even before the appearance of specific antibodies. From this day in the history of medicine, HIV is no longer a death sentence.
HIV treatment
Video “Stages of HIV development.
Treatment of HIV" There are no drugs that can completely cure HIV. The virus remains in the human body throughout life. However, special antiretroviral drugs (ARVs) have now been developed that prevent reproduction and reduce the amount of virus in the body, preserve or restore immune functions and prevent or cure opportunistic infections that occur against the background of immunodeficiency. Timely and correctly prescribed treatment can preserve health and prolong the life of patients with HIV infection for many years.
Treatment with these drugs is called combination therapy, or antiretroviral therapy (ART). This involves taking three or four drugs at the same time. Today, treatment for HIV infection is recommended to begin immediately after the disease is detected. This allows you to preserve the immune system and quickly suppress the activity of the virus, maintain quality of life and prevent the development of concomitant diseases.
The main goal of ART is the maximum suppression of HIV replication, which is accompanied by a decrease in the content of HIV RNA in the blood (BL) to an undetectable (by PCR) level.
However, not all people are ready to start taking drugs right away; some people will need a year or two, or even more, to decide to start taking ARV drugs.
The principles of ART are:
voluntariness
– conscious decision-making about the initiation of treatment and its implementation,
documented "informed consent"
»;
timeliness
– start ART as early as possible;
continuity
– long-term (lifelong) adherence to the ARVP regimen.
Having started such therapy, an HIV-positive person must take it regularly and without interruption throughout his life. Otherwise, a person who skips medications or stops treatment altogether will develop resistance.
Resistance is the adaptability of the virus to a given drug. This means the virus has changed in such a way that this drug no longer works on it. The range of medications used in ART is limited, so the next time the choice of drug combination is reduced. The worst thing is that changes in the virus will be transmitted further during infection. Therefore, when deciding to start treatment, the so-called adherence or readiness for ART is very important.
By law, in our country, treatment for HIV infection is provided free of charge to all citizens who need it.
Myths and with
The patient’s consent to start treatment is confirmed by filling out and signing the Informed Consent for ART
The treatment regimen is selected for each patient taking into account the identified characteristics - chronic diseases, mutations and resistance, tolerability of drugs and the effectiveness of their action.
Monitoring the effectiveness of treatment
In order to assess how treatment is going, whether ART is working and how intact the immune system is, doctors prescribe a set of tests. Among them there are two that are worth paying special attention to.
Immune status and viral load.
There are two very important tests that all people with HIV need - immune status and viral load. It is thanks to them that the degree of damage to the immune system and the effectiveness of drugs can be determined.
What is immune status?
Immune status determines the number of different cells of the immune system. For people with HIV, what matters is the number of CD4 cells or T-lymphocytes - white blood cells that are responsible for “recognizing” various pathogenic bacteria, viruses and fungi that must be destroyed by the immune system.
The CD4 cell count in an adult is usually between 600 and 1200 cells/mL.
In accordance with the WHO classification of immune disorders, the following degrees of immune disorders are distinguished:
— no or slight immunodeficiency: CD4 >500 μl;
- moderate immunodeficiency: CD4 350 - 499 µl;
- severe immunodeficiency: CD4 200 - 349 µl;
- severe immunodeficiency: CD4 <200 μl or <15%.
If the CD4 cell count is below 350 cells/ml, it is recommended to initiate antiretroviral therapy (ART) “for life-saving reasons”, since this immune status poses a risk of developing AIDS-related diseases.
A CD4 count below 350 cells/mL indicates severe immunodeficiency. In this case, it is necessary to take medications not only to treat HIV infection, but also to prevent opportunistic diseases: tuberculosis, fungal, bacterial and viral infections.
The main thing that the CD4 count tells us is about the health of the immune system: is it worsening or improving.
Changes in CD4 count
Your CD4 cell count can rise and fall as a result of infections, stress, smoking, exercise, your menstrual cycle, birth control pills, time of day, and even time of year, and different test kits may give different CD4 count results. .
That is why it is very important to regularly get tested for your immune status and look at changes in the results. It is impossible to assess the health status of an HIV-positive person using one single test. If you have an infection, such as a cold or herpes, it is best to delay getting tested until your symptoms have passed.
If you have a relatively high CD4 cell count (over 500), getting your immune status tested every 6 months is sufficient. If the cell count is less than 500 cells/ml, the examination must be carried out once every 3 months.
Without regular examination of the immune status, it is difficult to determine how the disease develops and whether adjustment of the prescribed ARV therapy is necessary.
What is viral load?
Viral load shows the number of viral particles in 1 ml of blood. A viral load of up to 10,000 copies/ml is considered not high. From 10,000 to 50,000 copies/ml – medium. From 50,000 to 100,000 copies/ml and above – high.
If we compare the development of HIV infection with a train that goes to the AIDS station, then the immune status is the distance that remains, and the viral load is the speed at which the train is moving.
Changes in the viral load are used to judge the effectiveness of therapy and the correct selection of drugs when taking ART.
In a person regularly taking ART drugs, after 3 months from the start of treatment, the viral load should reach an undetectable level and remain at this level throughout the entire treatment period.
An undetectable viral load indicates that there is very little virus in the human body, which means there is very little chance of transmitting HIV to other people, even with unprotected sexual contact. This is what the U=U movement is based on - undetectable burden = impossibility of HIV transmission. Any risk of sexual transmission of HIV is related to viral load, and undetectability reduces this risk to zero.
ART is not only good for your health, but it also protects your partners.
Treatment of concomitant diseases - hepatitis B and C, tuberculosis, herpes viral infection, toxoplasmosis, etc. - is carried out in accordance with recommended regimens and depends on the severity of the disease and the degree of damage to the immune system.
PCR in the diagnosis of infectious diseases
Today, PCR diagnostics of infections is one of the most accurate, sensitive and effective clinical laboratory methods. The range of detected pathogens is practically unlimited - a test system would be developed to analyze the desired pathogen.
Due to its high sensitivity, PCR allows you to detect the pathogen even with its minimal content (that is, when only a few molecules of its DNA are present in the biomaterial being studied).
PCR detects pathogens of infectious diseases when this cannot be done by other methods (immunological, cultural, microscopic). Therefore, for a number of infectious agents, the polymerase chain reaction method has become the “gold standard”; it is time-tested and clinically approved. This method allows not only to establish the etiology of the disease, but also to monitor the course of the infectious process and evaluate the effectiveness of the treatment.
Analysis by PCR method is especially relevant in the asymptomatic course of the infectious process caused by unconditionally pathogenic microorganisms - causative agents of sexually transmitted infections (Chlamydia, qualitative determination of DNA; Mycoplasma, qualitative determination of DNA; Causative agent of gonorrhea, qualitative determination of DNA; Causative agent of trichomoniasis, qualitative determination of DNA) . For example, with chronic gonorrhea in women, even using the bacteriological method, it is often not possible to identify gonococcus, despite the existing symptoms of a chronic inflammatory process in the cervix or urethra.
Modern PCR diagnostics allows not only to identify the presence of genetic material of the infectious agent, but also to determine its quantity. Determining the number of pathogens is important for deciding on treatment, its methods and duration, especially if opportunistic microorganisms are identified (Mycoplasma, quantitative determination of DNA; Ureaplasma typing, quantitative determination of DNA).
The CMD laboratory has developed the “Multiprime” PCR research format, which makes it possible to detect several pathogens in one test tube (and one reaction).
- Comprehensive STI research
- Urogenital infections in men
- Urogenital infections in women
- Causative agents of intestinal infections
- Causative agents of intestinal infections
- Pathogens of whooping cough/parawhooping cough
- Diagnosis of ARVI
- Pathogens of infections transmitted by ixodid ticks
- Herpesviruses
Primary prevention (preventive treatment) of secondary (opportunistic) infections
When the immune system is deeply damaged, it is important to prevent the development of diseases, the pathogens of which have the opportunity to parasitize in the body that finds itself without protection. Such diseases are called opportunistic, and pathogens are called opportunists from the Latin opportunus - opportunity. It is for this purpose that schemes for the prevention of opportunistic diseases were created for those patients whose immunodeficiency does not allow effective defense. These regimens involve taking medications used for treatment, but in doses that are lower than needed to fight an existing infection.
It is very important to take medications as prescribed by your doctor in accordance with the prescribed regimen. This can save lives, because against the background of a weakened immune system, such diseases can become fatal.
To prevent secondary infections, it is necessary to exclude their presence.
Prevention of Pneumocystis pneumonia and toxoplasmosis with CD4 count < 200 μl-1 (less than 15%) - it is recommended to take Co-trimoxazole according to the regimen until the CD4 + lymphocyte count increases during ART > 200 cells/μl for 3 months.
Prevention of fungal diseases, incl. candidiasis - antifungal drugs as prescribed by a doctor.
Prevention of non-tuberculous mycobacteriosis - azithromycin or clarithromycin according to the regimen.
Prevention of tuberculosis - isoniazid according to the regimen (or another drug combined in ART).
The dosage of drugs and the course of treatment depend on the degree of immunodeficiency and the severity of the patient’s condition.
Memo for HIV-positive people: what is important to remember about your health
Studying all the information about the treatment of HIV infection is not an easy task. To help people with HIV better navigate health issues, you need to know some quick information that can help you stay healthy.
1. Avoid eating raw or undercooked meat, raw fish or raw eggs. They may contain germs that are dangerous to you.
2. If you have never had hepatitis A or B, talk to your doctor about getting vaccinated against them.
3. Undergo medical examination prescribed by the attending physician of the AIDS center:
Fluorography or radiography of the OGK - diagnosis of tuberculosis (once every 6 months)
electrocardiogram
Ultrasound examination of the abdominal organs (comprehensive)
ultrasound examination of the kidneys and adrenal glands
Examinations of doctors depending on the clinical manifestations of secondary diseases (dermatovenerologist, general practitioner, neurologist, otolaryngologist, ophthalmologist, obstetrician-gynecologist, oncologist and others).
4. Going to the dentist regularly is very important. It is advisable to have a dental examination twice a year. The first HIV-related diseases usually appear in the oral cavity.
5. Do not refuse visits to the doctor at the AIDS center. It is necessary to undergo regular testing for viral load and immune status.
6. It is better to avoid unnecessary “activation” of the immune system; due to HIV, it already has enough work to do. All diseases, especially infections, even those not related to HIV, must be treated as soon as possible. When the immune system is “activated,” the virus can multiply faster.
7. HIV-positive women need to monitor the condition of the cervix. Every 6 months you need to undergo a full gynecological examination, and it is advisable to do a cytological analysis of the cervical mucosa. This will help prevent cervical cancer.
8. If you feel constantly tired, talk to your doctor about possible anemia (low hemoglobin levels in the blood) or low hormone levels. Prompt diagnosis and treatment of these problems can help.
9. If you suddenly and rapidly lose weight, you will need treatment for weight loss syndrome.
10. If your immune status is above 200 cells/ml, get vaccinated according to the national vaccination calendar, this will help you avoid severe infectious diseases - influenza, coronavirus infection.
11. If you have HIV, this does not mean that your child will have it. Currently, the risk of mother-to-child transmission of HIV is less than 2%.
12. ARV drugs can cause undesirable (side) effects in the first month of use. If after a month they continue to bother you, consult your doctor; perhaps the proposed treatment regimen is not suitable for you.
13. Immune status determines the state of the immune system, and is an even more important test than viral load. HIV infection affects the number of CD4 cells that are destroyed by the virus. The CD4 count can be a percentage (of the total number of lymphocytes) or an absolute count (the number of CD4 per milliliter of blood). The percentage is more stable, so it can more accurately indicate the development of HIV infection.
14. Usually, although not always, viral load allows you to “predict” how quickly HIV infection will develop. The higher your viral load, the more likely it is that your CD4 count will begin to decline rapidly in the near future. If the viral load is less than 50 copies/ml, the likelihood of disease progression is extremely low.
15. Find out what signs may be present in HIV-associated cancers: Kaposi's sarcoma and non-Hodgkin's lymphoma. The sooner these diseases are diagnosed, the easier it will be to treat them.
The main treatment for HIV infection is a combination of three or more antiretroviral drugs. They make it possible to reduce the viral load below a detectable level, improve immune status and prevent HIV-associated diseases. Your doctor will choose a combination depending on your medical history and your attitude toward the dosage regimen, dietary restrictions (for example, take the drug on an empty stomach or with food) and possible side effects. You need to work with your doctor to choose a combination that's truly right for you.
Medicines must be taken every day, on time. If you are unable to do this, it is best to talk to your doctor about stopping therapy and possibly changing the combination. Regularly skipping medications can cause the virus to become resistant to their effects.
Half-time rule: if you forget to take the drug at the appointed time and there is less than half the time left before the next dose that should pass between doses, then you should not take the pill. If it is less, then the drug can be taken. For example, if you take the drug every 12 hours (in the morning, at 7.00 and in the evening at 19.00), then in the first 6 hours after missing it (i.e. until 13.00) you can take the missed pill. If you remember about the omission when there are less than 6 hours left before the next dose, the tablet must be taken only at the appointed time, i.e. at 19.00
Do not take any medications, vitamins, or dietary supplements, including over-the-counter ones, until you are sure they are compatible with the medications you are taking.
It's important to take care of your eyes. If your vision has deteriorated or you experience a “blurry picture,” be sure to consult a doctor.
Learn to communicate and collaborate with your doctor. Many people have problems in their relationship with their doctor, while others simply avoid visiting the doctor. However, as a result, you will only suffer yourself. Be proactive about your health and it will save you from many problems in the future.
Why is it worth getting tested?
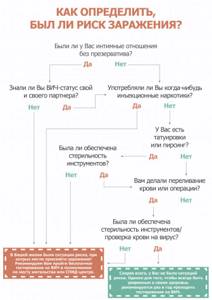
Regular HIV testing is recommended for adolescent and adult patients aged 13 to 64 years. The sooner a person finds out that he has HIV, the sooner he can receive a referral for treatment and live a normal life. Refusing this knowledge often only shortens life and puts others at risk in the long run. Particular attention should be paid if:
- unprotected sexual contact with new partners is practiced;
- taking drugs;
- intravenous medications are used, including steroids, hormones, and silicone;
- previously diagnosed with tuberculosis or sexually transmitted infections (STIs), such as hepatitis B or syphilis;
- pregnancy is planned or has already occurred;
- forced sexual contact occurred.
Even if you are monogamous (both partners have no sexual contact except with each other), there is a risk of becoming infected, so do not neglect taking an HIV test.