September 24, 2021
High blood viscosity is the medical term equivalent to the colloquial expression “thick blood.” It is traditionally believed that blood thickening is associated with an increase in the level of prothrombin, a component of the blood coagulation system.
According to medical research, cardiovascular diseases can have different causes. And if some (heredity, age) remain unchanged, then others can be corrected by giving up bad habits and changing lifestyle.
High blood viscosity is the medical term equivalent to the colloquial expression “thick blood.” It is traditionally believed that blood thickening is associated with an increase in the level of prothrombin, a component of the blood coagulation system. This opinion exists due to the fact that serious complications of cardiovascular diseases such as heart attack and stroke occur more often with elevated levels of prothrombin. In fact, viscosity is determined by many factors.
The main function of blood is to transport respiratory gases, hormones, nutrients and many other substances to organs and systems. Almost all active processes that occur in our body directly depend on this. Deviation from the norm provokes its thickening and liquefaction. In both the first and second cases, this leads to undesirable results.
You won't be able to tell by the appearance of your blood whether your blood is thick or thin. This can only be determined with the help of a general blood test and a coagulogram, which are prescribed by a doctor during periodic medical examinations or if a disease is suspected. In critical situations, namely: injuries, operations, hypothermia, lack of sleep, etc., thick blood poses a danger. In the older age group, the experience of these disorders is more extensive, and they manifest themselves differently - with heart attacks and strokes. Thick blood moves much worse through the vessels, creating additional stress on the heart, which increases the risk of blood clots in the vessels. Often, when your blood is thicker, your body produces more hemoglobin. Excessively thick blood penetrates much worse into small vessels and capillaries, because of this the body feels a lack of oxygen. Therefore, blood thickening should be noticed as early as possible and consult a doctor.
Why is blood thinned?
Bleeding disorders can occur at any age. First of all, this problem concerns everyone over 50 years of age. Thick blood puts additional stress on the heart. This is due to the fact that it is more difficult to pump thick liquid through a huge circulatory system; more power is required, which the heart must produce. At the same time, the pulse becomes faster and the tremors become stronger. During such work, the heart muscle wears out faster, the valves fail, and the tightness of the atria is compromised.
Another danger of thick blood is the formation of blood clots. Thrombi are individual clots that form as a result of platelets sticking to each other. The resulting blood clots attach to the walls of blood vessels and interfere with blood flow. But the worst thing for a person’s life is a detached blood clot. As it rushes through the circulatory system, the current carries it to the lungs and then to the heart. By blocking the lumen of an artery in one of the organs, a blood clot causes an ischemic stroke, which often leads to death.
In addition, thick blood cannot supply organs and tissues with nutrients in a timely manner, which is why the body suffers from mild forms of hypoxia. The thicker the biological fluid, the more difficult it is for it to rise from the lower extremities to the heart. As a result, blood stagnation in the veins, thrombosis and varicose veins appears.
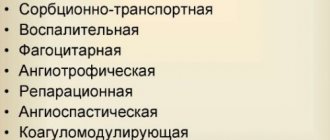
Platelets in men
Platelets are a special blood enzyme that is responsible for blood clotting. They play a huge role in many physiological processes. The size of these cells is small: only 2 - 4 micrometers. Their lifespan is only ten days, after which they are destroyed in the spleen. Every day, the human body produces about 70,000 new platelets. They are formed in the bone marrow, and a special hormone, thrombopoietin, is responsible for their production. It is synthesized in the kidneys and liver and, along with the bloodstream, enters the bone marrow.
With a limited number of platelets, the blood clotting process slows down, but if there are a lot of them, this can cause the formation of blood clots. Due to their special structure, platelets move throughout the body towards damaged walls, attach to them, form a blood clot and stop bleeding. You can determine your platelet count by taking a blood test. The normal platelet count in the blood of men differs from that of women. If there is a deviation from normal values, you should consult a doctor.
Thinning agents
The most affordable ones today are drugs based on acetylsalicylic acid, better known as Aspirin. Such medications are common in pharmacies and cost little. Due to the fact that acetylsalicylic acid carries certain risks for the hematopoietic system and can cause gastric bleeding or ulcers, medicine has actively begun to work on the creation of drugs free from aspirin. Such dosage forms are available in pharmacies today. This group of drugs is divided into two subgroups
- antiplatelet agents that prevent blood cells from sticking together.
- anticoagulants, which prevent the formation of fibrin clots during coagulation.
Such drugs can be prescribed not only to older people to thin the blood, but also to pregnant women, in order to ensure the best blood flow between mother and fetus. A course of taking medications from this group saturates the blood with oxygen, which is very important for the developing fetus.
Blood tests to determine your platelet count
The level of platelets in the body is calculated as part of a coagulogram.
Laboratory testing evaluates a set of blood properties. The result of the analysis helps not only to identify the level of clotting, but also to determine where the failure occurred. The study includes the following indicators:
- thrombin time - a value indicating the period of conversion of fibrinogen to fibrin;
- activated partial thrombin time is an indicator that allows you to evaluate the work of plasma blood factors;
- prothrombin index - a value indicating the time period of blood clot formation;
- Plasma fibrinogen is an indicator of a protein that turns into fibrin and promotes the formation of blood clots.
Antiplatelet agents
The main indications for prescribing antiplatelet agents are:
- Cardiac lesions that have led to a lack of blood circulation in the myocardium or completely deprived it of blood flow.
- Ischemic heart lesions, especially those accompanied by tissue necrosis.
- Arrhythmia.
- Tachycardia.
- Prevention of thrombosis in patients who have had a stroke.
- Heart surgery or interventions to restore the circulatory system (stenting).
- Arterial damage.
The cost of such medicines is slightly higher than those containing acetylsalicylic acid. As a rule, such medications are taken in a course, which ensures high rheological properties of the blood constantly.
Norm
The level of platelets in men changes at each age stage. The number of these cells is measured in billions per liter of blood. Normal platelet count in men:
- in adolescents under 16 years of age - from 160 to 390 billion/l
- in young people from 16 to 25 years old - from 180 to 380 billion/l
- men from 26 to 35 years old should have from 180 to 400 billion/l
- in men under 60 years of age, platelets per liter of blood are up to 340 billion with a lower threshold of 180
- in elderly men over 60 years of age, the platelet count ranges from 180 to 320
In young people, as can be seen from the indicators, the platelet count in the blood is high. By the age of 18, the process of formation of the hematopoietic system ends in a young man, therefore, the composition of the blood approaches the norm characteristic of an adult man. While the lower indicators remain unchanged, the upper ones are constantly changing. The older a man gets, the lower the upper limit becomes.
Preparations without acetylsalicylic acid
Patients over 18 years of age who do not have problems with the gastrointestinal tract are safely prescribed medications containing aspirin. Especially if the duration of use does not exceed 5-7 days. In other cases, it is recommended to avoid consuming large doses of acetylsalicylic acid, especially in older patients.
The list of antiplatelet agents that do not contain aspirin includes:
- Curantil with the active ingredient dipyridamole.
- Ticlid, whose action is based on ticlodipine.
- Plavix, blood thinners thanks to cropidogrel.
- Brilint, which is based on the active ingredient ticagrelor.
- Efficient, working thanks to prasugrel included in the composition
- Pletax with the active ingredient cilostazol.
- Trental, whose action is due to pentoxifylline.
A wide selection of drugs allows a competent doctor to select an individual course of therapy for each patient, based on possible side effects and the presence of chronic diseases in the patient.
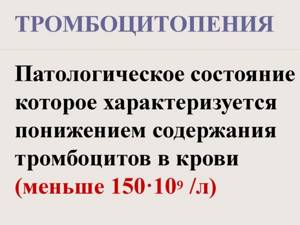
Causes of low platelets
A condition in which platelet levels decrease is called thrombocytopenia. If the pathology occurs during menstruation, it does not require treatment. During pregnancy, changes in the number of blood cells are caused by the formation of the uteroplacental blood flow . In some cases, thrombocytopenia can threaten miscarriage due to the development of uterine bleeding. The reasons for a critical decrease in cells during pregnancy include:
- taking diuretics or antibacterial drugs;
- placental abruption;
- intoxication of the body;
- features of the immune system;
- hyperfunction of the thyroid gland;
- viral and infectious diseases.
A decrease in platelet volume is indicated by the body's tendency to bleed. A woman may notice the appearance of bleeding gums and prolonged healing of even minor wounds and scratches . Unreasonable nosebleeds and bruises on the body also occur . A small rash forms on the skin surface.
How to raise platelet levels
Before treatment, blood is donated for a detailed study. It is important to normalize the number of blood platelets before labor. There is a risk of internal bleeding or cerebral hemorrhage. In the autoimmune form of thrombocytopenia, the child may receive antibodies from the mother. This leads to transmission of the disease to the newborn.
Corticosteroids are prescribed to increase the number of blood cells . These include Dexamethasone and Prednisolone . At the same time, glucocorticoids are prescribed . Injections of immunoglobulin are sometimes practiced .
In advanced cases, donor blood transfusion . If treatment fails, a decision is made to remove the spleen . It is an organ that has a destructive effect on blood plates. Most often, the operation is performed laparoscopically. The question also arises about the method of delivery of a woman with thrombocytopenia.
Chimes with depyridamole
This drug can be called mandatory for use by pregnant women after the 20th week of gestation. In the annotation you can read a phrase warning about possible risks. If a local obstetrician-gynecologist has prescribed a course of Curantil, this indicates that the woman is not at risk and can safely take a blood thinner.
The medicine accelerates the blood, allowing the expectant mother to share nutrients with the child. Taking Curantil will ensure the full development of the unborn baby.
And if the indicators are reduced
Thrombocytopenia is manifested by increased bleeding, frequent hematomas and spontaneous bleeding. Most often, various autoimmune diseases cause excessive destruction of red blood cells, which causes a decrease in their levels. Also, some viral diseases can provoke such conditions. Thrombocytopenia is observed with hepatitis, HIV, herpes, ARVI, etc.
A decrease in the number of red blood cells below 20*109/l is critical for the health of any woman; in such situations, treatment should be carried out in a hospital.
An independent disease with a decrease in the level of these formed elements is thrombocytopenic purpura, the trigger for which is various infectious pathologies.
HELLP syndrome
At the end of pregnancy, pathology is sometimes observed, one of the manifestations of which is a decrease in the number of platelets and an increased risk of developing DIC - a disorder of blood clotting. With HELLP syndrome, a decrease in the level of red blood cells, yellowing of the skin, impaired liver function, etc. are also observed. All this leads to fetal suffering and threatens the woman’s life, so establishing this diagnosis is an indication for emergency delivery.
We recommend reading the article about getting tested during your period. From it you will learn about in what cases it is possible and in what cases it is not possible for a woman to take a blood test on the days of menstruation, as well as about the possibility of donating urine and conducting an ultrasound examination.
Description of the drug Tiklpid
Taking Triclid can reduce the aggregation of blood platelets and significantly reduce the viscosity of biological fluid. Violation of the prescribed treatment regimen and overdose can lead to the following adverse reactions:
- bleeding;
- lack of platelets necessary for natural blockage of damaged areas of arteries, vessels and tissues;
- decreased levels of white blood cells;
- abdominal pain;
- diarrhea.
In case of severe blood thickening, the drug is prescribed for a long course, and the patient’s condition is regularly monitored. When the rheology of the main biological fluid is restored, the drug can be discontinued. However, stopping the medication does not replace regular blood quality testing.
Normal values
The gold standard is considered to be the content in the blood of an adult woman from 160 * 109 to 400 * 109 in one liter of blood. However, there are a number of conditions when physiological indicators shift in one direction or another as normal. These include:
- Pregnancy. At the same time, in the first and second trimesters there is a slight decrease in the number of red blood cells. The lower limit of normal in this case is 90-140*109/l. This condition develops to ensure proper formation of placental vessels and blood supply to the fetus. This is also due to the relative dilution of the blood liquid component of plasma. On the eve of childbirth, there may be a slight increase in the number of platelets and coagulogram parameters (shows the clotting properties of blood). This is provided by nature so that during childbirth a woman loses as little blood as possible. Readings above 450*109 in one liter of blood are already considered a pathology.
- Women experience significant fluctuations in platelet levels during their cycle. The highest values are observed during the period of ovulation, and the moment coincides with the maximum basal temperature. When approaching critical days and during them, the number of red blood cells decreases significantly, sometimes becoming less than the normal limit. During menstruation, platelets even reach 120 - 140 * 109 in one liter of blood.
“Reading” blood: what factors influence the test result?
Useful articles / July 25, 2017
- A person begins taking a general blood test (CBC) from birth. Based on its results, it is possible to obtain information for the diagnosis of many diseases, assess their severity and monitor the dynamics of the treatment.
To evaluate the results of the OAC, special standards are used, but there are factors that influence the indicators. Can a person independently decipher the numbers of a general blood test? And what influences the deviation from the norm?
Manually or automatically?
In modern laboratories, not everything is yet subordinated to artificial intelligence. Yes, the vast majority of laboratories use automatic hematology analyzers to conduct a general blood test. In just a few minutes, the analyzer performs complex calculations of erythrocyte, leukocyte and platelet parameters. However, some defective cells may be identified incorrectly - destroyed, immature and deformed cells. In this case, a microscope is needed - on it the doctor examines the blood smear after examination with a hematoanalyzer.
“It cannot be said that a manual or automatic method of studying a general blood test is better; they complement each other,” comments Yulia KOCHKALDA, leading specialist in medical diagnostics . – Doctors working in the laboratory compare the indicators from the hemoanalyzer and microscopy, and if there is the slightest doubt, they will ask the patient to repeat the study.
What influences the result of the analysis?
Sometimes it happens that the result of a blood test differs from the norms that the patient can independently find on the Internet. The numbers vary for various reasons and do not always mean deviations in the body’s functioning. Therefore, we recommend that you do not engage in “blood reading” on your own and guess what this or that indicator means. Entrust the interpretation of the analysis to doctors and do not jeopardize your own health. But be sure to remember four factors that can distort a general blood test:
Physical exercise . It doesn’t matter whether a person has been involved in sports or for how long. The main thing is to be at rest 30-40 minutes before the test. It is advisable to limit exercise the day before blood sampling. Eating. It is not recommended to eat food earlier than 8 hours before the test. The day before donating blood, we advise you to exclude fatty and spicy foods from your diet. Menstruation. During critical days, a woman’s platelet count decreases. To avoid getting a false test, reschedule your blood donation to another day of your cycle. Taking medications . Many drugs affect the test result. Therefore, on the day of donating blood, do not take any medications; it is recommended to give up even vitamins. Before taking blood, consult your doctor; some medications should not be taken several days before the test.
Alarm bell: what does blood “say”?
What do changes in the general blood test signal?
What diseases may this indicate? We do not recommend making a diagnosis yourself based on a blood test. However, after consulting with a doctor, you can give yourself a “tour” of your own body and pay attention to the processes occurring in it. erythrocytes
| COMPONENTS | INCREASE | DEMOTE |
| erythrocytes | polycythemia; stay in the mountains; heart diseases; tumors that produce erythropoietin; stress; smoking; blood concentration during dehydration. | anemia; hemolytic crisis; renal failure; blood loss; bone marrow aplasia; influence of toxic substances and medications. |
| HEMOGLOBIN | polycythemia; staying at high altitude; conditions associated with hypoxia; tumors producing erythropoietin; stressful conditions; dehydration. | for all types of anemia; hemolysis of red blood cells; renal failure; bleeding; red bone marrow aplasia; taking certain medications; pregnancy. |
| HEMATOCRIT | prolonged hypoxia, dehydration, leukemia, tumor processes in the kidneys. | anemia, hyperhydration, hyperproteinemia, pregnancy. |
| MCV (mean erythrocyte volume) | B12 and folate deficiency anemia, kidney disease, alcohol abuse, myxidema, bone marrow aplasia, reticulocytosis, use of anticonvulsants. | with iron deficiency; hemoglobinopathies (thalasemia); anemia in chronic diseases; sideroblastic anemia; lead poisoning. |
| MCH (hemoglobin content in red blood cells) | hyperchromic and megaloblastic anemia, hypothyroidism, liver diseases, cancer. | long-term lead intoxication, thalassemia, hypovitaminosis B12, chronic inflammatory processes, iron metabolism disorders. |
| RETICULOCYTES | anemia; acute blood loss; anemia treatment. | aplastic anemia; anemia due to impaired maturation of red germ elements; liver diseases; condition after blood transfusion; chemotherapy. |
| NEUTROPHILS | for all bacterial infections; acute and chronic myeloid leukemia; generalized tumors; stressful conditions; with tissue necrosis; vasculitis; decompensation of diabetes mellitus; acidosis; taking lithium, glucocorticoids; adrenaline; for leukemoid reactions, sepsis, endocarditis, miliary tuberculosis and tumor metastasis. | with viral infection, aplastic anemia, radiation, agranulocytosis, immunosuppression, taking certain antibiotics, chemotherapy drugs, thyreostatics, analgesics, psychotropics. With lymphocytic leukemia and monocytic leukemia, there is a relative decrease in neutrophils. |
LYMPHOCYTES
| COMPONENTS | INCREASE | REDUCTION |
| LYMPHOCYTES | for chronic infections, tuberculosis, chronic limadenopathy, infectious mononucleosis, Hodgkin's disease, Addison's disease, idiopathic thrombocytopenic purpura. | for AIDS and related diseases, bone marrow damage after chemotherapy and radiation therapy, steroid treatment, Cushing's disease, aplastic anemia, neurological diseases. |
| MONOCYTES | for viral, parasitic and protozoal diseases, sarcoidosis, Crohn's disease, tumors. | for aplastic anemia, chronic lymphadenopathy, treatment with glucorticoids. |
| EOSINOPHILES | allergic diseases, bronchial asthma, parasitic infections, collagenosis, angioedema, Hodgkin's disease, skin diseases. | general decrease in immunity, extensive burns, infectious diseases, dysentery, acute appendicitis, stress, prolonged pain, intoxication of the body. Source: https://womanadvice.ru/eozinofily-ponizheny |
| BASOPHILES | chronic myeloid leukemia, hypothyroidism, mastocytomas and systemic mastotosis. | Infectious diseases, stress, pregnancy, Cushing's disease, hyperthyroidism, regular stress conditions, allergies with severe manifestations, active thyroid function, pneumonia, adrenal diseases. |
PLATELETS
| COMPONENTS | INCREASE | REDUCTION |
| PLATELETS | acute inflammatory processes in the intestines, conditions after removal of the spleen, myeloproliferative diseases, infections, blood loss, sideropenia, pancreatitis. | with enlarged spleen, liver cirrhosis, bone marrow damage, alcoholism, Helicobacter pylori infection, collagenosis, DIC syndrome, coagulopathies, septic conditions. |
| MPV (mean platelet volume) | idiopathic thrombocytopenic purpura, thyrotoxicosis, diabetes mellitus, myeloproliferative diseases, atherosclerosis, smoking, alcoholism. | splenectomy, Wiskott-Aldrich syndrome. |
| PCT (thrombocrit) | myeloproliferative diseases, splenectomy, iron deficiency in the body, viral diseases and inflammatory diseases of other etiologies, atherosclerotic process, diabetes mellitus, smoking. | apastic anemia, myelodysplastic syndrome, megaloblastic anemia, collagenosis, hemoblastosis, ionizing radiation, the use of certain medications, hematopoietic tissue tumors, intoxication, chronic renal failure, liver cirrhosis. |
| PDW (platelet distribution width by volume) | inflammatory process, anemia, postoperative period, blood loss. | myelodysplastic syndrome, leukemia, bone marrow metastases, thrombocytopenia, radiation sickness, chronic hepatitis. |