X-ray is a modern way to diagnose many respiratory diseases. This is often important when diagnosing pneumonia in children.
Modern medical clinics use x-rays to determine the type and stage of inflammation in the lungs, which makes it possible to prescribe more accurate and effective treatment.
In many cases, you can do without an x-ray. For example, with harmless environmental pneumonia, it is not always advisable to confirm pneumonia with an x-ray examination. In such situations, immediate treatment with antibiotics is important.
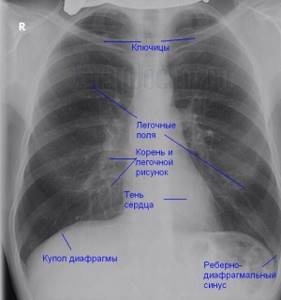
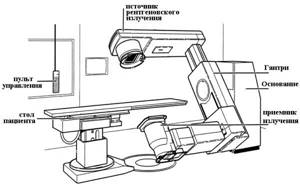
An x-ray is a negative image of an organ shown on photographic film. The image is obtained through various projections aimed at the area of the body being examined. This image is used to evaluate the condition of the organ and identify abnormalities or problem areas.
In modern medicine, the following types of x-rays are used to diagnose not only pneumonia, but also other diseases:
- Tomography is the study of an organ using layer-by-layer radiography. For this purpose, a classic or spiral computed tomograph is used.
- Fluoroscopy - examination is carried out using a special X-ray screen. This allows you to look at the anatomical features of the organ and comprehensively assess its functional state.
- Fluorography is a study of the chest organs with enlarged images. The number of rays passing through the patient's body is also reduced.
Most often in modern clinical medicine, radiography is recommended as the best option for diagnosing various diseases.
How does the device work?
The principle of operation of this device is quite simple - the device's emitter sends a beam of X-rays, which passes through the patient's body and displays the image on a special film. This process is similar to the photographic method, but because human organs transmit rays differently, the result is an image with a different negative color. The soft tissues are gray, the cavities are black, the bones are white (due to radiation absorption).
There are 2 types of radiography:
- survey (examines the lungs as a whole);
- targeted (a fragment of an organ is examined).
There are some difficulties in diagnosing pneumonia in children using x-rays. This is due to the small volume of lung tissue and a large number of structural elements in a small study area. For this reason, difficulties arise in correctly assessing the picture of the lungs and recognizing the condition of the pulmonary roots and lymph nodes.
Age-related features of pneumonia in children
There are several forms of the disease:
Intrauterine transplacental
The source is the mother, infection occurs in the womb. The infection reaches the fetus through the hematogenous route, that is, through the blood. The presence of a focus of infection in the maternal body is characteristic. Often this type of disease can be accompanied by sepsis. Infants in the first hours of birth, in the presence of intrauterine pneumonia, may experience the following symptoms:
- respiratory failure;
- dyspnea;
- blue discoloration of the skin;
- wet rales.
An x-ray can immediately after birth confirm the presence of lesions.
Intrauterine amniotic
The source of infection is the mother; the pathogens enter the fetus's body along with infected amniotic fluid, which the baby swallows. One of the signs of the presence of a lesion is the diagnosis of polyhydramnios in a woman.
Intrapartum
The source is the mother's body. Infection occurs during the movement of the fetus through the birth canal. The route of transmission of infection is contact - contamination with pathogens contained in the amniotic fluid (amniotic fluid) and mucous secretions. Signs do not appear immediately, but after 2-3 days after birth. The clinical picture is similar to intrauterine infection.
The initial stage is characterized by:
- respiratory failure;
- toxicosis;
- weakness, lethargy;
- the baby refuses the breast;
- foam is released from the oral cavity.
The following signs are common:
- diarrhea;
- otitis;
- conjunctivitis
Postnatal pneumonia (domestic)
The source of infection is the people around the baby at home. Infection occurs after discharge from the hospital. The route of transmission of the infectious agent occurs through the air - aerogenic method. Most often, the disease is associated with the presence of pneumococcal pathogens and massive contamination of the upper respiratory tract.
The disease begins acutely and the following symptoms are observed:
- cough;
- heat;
- sputum discharge;
- breathing may be weak or harsh;
- fine bubbling rales are heard.
Postnatal nosocomial (in-hospital)
The source of infection is medical workers and equipment. Infection occurs after birth. There are several ways of infection - bronchogenic (the disease originates in the bronchi), contact, aerogenic (rare infection through the air). More often they begin in the first week of life with general symptoms of toxicosis.
It is characterized by signs of acute toxicosis and a change in the acid-base balance towards increasing acidity. More often, the symptoms have blurred signs and can have a rapid course with a fatal outcome. Infants on mechanical ventilation (artificial pulmonary ventilation) may develop early pneumonia - in the first 5 days, and late pneumonia - in the next 5 days.
How to read pictures?
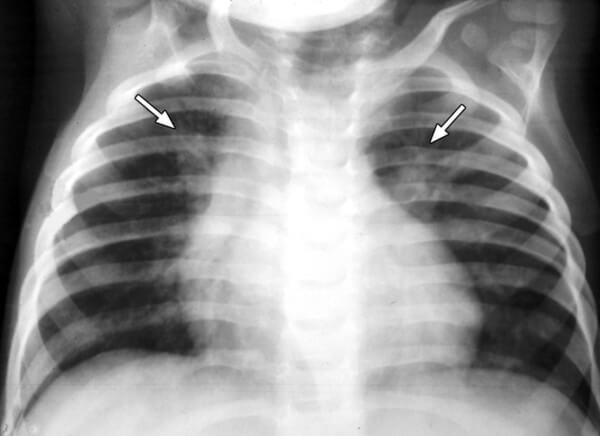
The most common symptom of pneumonia in children, which appears on photographs, is focal shadows in the lower segments of the lungs with a diameter of 1-2 mm.
Shadows on scans can be different and are divided as follows:
- 3 mm - small;
- 4-7mm - medium;
- 8-12 mm - large;
- Focal length - 12 mm or more.
Lung lesions manifest themselves in the following forms:
- oval shape;
- circular;
- circular.
Acute pneumonia: features of the course and symptoms
Acute pneumonia (pneumonia acuta) is a disease that has different etiologies and, depending on the pathogen, different symptoms. Most often, this form of the disease occurs in children under 3 years of age. It is characterized by the presence of infiltrates in the lung tissues (accumulations of cellular elements with the addition of blood and lymph particles) and filling of the alveoli with exudate containing neutrophils (leukocytes that protect against infectious pathogens).
Acute pneumonia can be caused by:
- viruses;
- bacteria;
- atypical pathogens.
Pneumonia in its acute form can be either an independent disease or a complication of previously suffered diseases. Depending on the pathogen, symptoms of acute pneumonia may include the following conditions:
- signs of intoxication - fever, lack of appetite, weakness, etc.;
- when listening, changes are detected - noises, wheezing, short breathing, etc.;
- X-ray reveals areas of infiltration in the form of darkening;
- the disease in most cases is accompanied by a cough;
- respiratory failure is observed (shortness of breath, rapid breathing, etc.)
The main predisposing factor for the development of pneumonia is hypothermia.
Different types of pathologies in the photo
Each type of pneumonia looks different on x-rays, which is how the disease can be diagnosed. Let's look at different types of pneumonia, their images in photographs and explanations.
Focal
Focal (or focally illuminated) form of pneumonia - foci of infiltration have a diameter of 0.5-1 cm and are located in one or several segments of the lung. Sometimes lesions can be localized on both sides. The lung tissue becomes catarrhal, and serous exudate forms in the lumen of the alveoli. If the focal form becomes focally pure, individual areas of infiltration merge into one large lesion, which can often cover the entire lobe.
The image may show single small formations (1-1.5 cm) in one of the lungs (or both in the case of bilateral forms). In this case, expansion of the roots of the lung is visible as a result of filling with exudative fluid.
Segmental
Segmental pneumonia - the entire segment of the lung becomes inflamed. This form of pneumonia can be complicated by atelectasis (collapse of part of the lung with complete loss of aeration. The segmental form of inflammation can be a manifestation of long-term pneumonia, progressing to pulmonary fibrosis, or complicated by local chronic bronchitis. The entire segment is visible on x-rays.

Krupoznaya
Irregular pneumonia is a hyperglycemic inflammation that goes through the following phases: erythema, redness and gray swelling, and a recovery period.
Imaging shows that the inflammatory process is localized large or subscapularis (i.e., the affected lobe of the lung) with the involvement of the pleura. The pulmonary pattern is changed and the pulmonary roots are expanded. Fluid stagnation is observed in the pleural cavity. As the disease progresses, the shadows in photographs become darker.
Abscess
With purulent pneumonia, the image clearly shows complete darkening of the infiltrate area and thickening of the pleura; cavities up to 2 cm are observed in which purulent fluid accumulates.

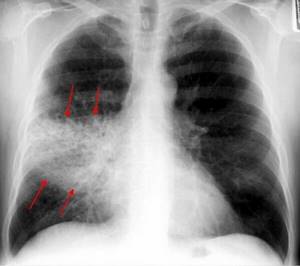
Interstitial
Interstitial pneumonia - lesions of a focal or disseminated nature occur with infiltration of interstitial tissue. In children, this form of pneumonia is caused by viruses or pneumocystis.
The image shows protrusion of the vascular bundle and enlargement of the pulmonary roots. The intense silhouette of a “tree branch” becomes noticeable, which is a specific symptom of the disease.

Aspiration
With aspiration pneumonia, bronchial obstruction in the form of triangular shadows is visible on x-rays. The diaphragm is raised.

Viral pneumonia: pathogens and signs
Pneumonia can be caused by various viruses, most often it is provoked by parainfluenza virus, chickenpox, measles, cytomegalovirus, viruses of categories A and B. In this case, the child’s pulmonary alveoli are filled with purulent exudate (liquid).
This form of pneumonia affects both children under one year old and older ones. Among the main signs of the disease are the following:
- in the initial stage, the cough is dry, “barking”, and with the development of inflammation it turns into a wet one;
- rapid breathing, whistling often appears;
- when coughing, the patient feels pain in the area of the shoulder blades or chest;
- the temperature is elevated;
- cyanosis of the skin of the fingertips and nasolabial triangle;
- decreased appetite;
- chills;
- dyspnea;
- headaches, muscle, joint pain.
Often, pneumonia is “masked” as a common cold and it becomes difficult to recognize. But with pneumonia, unlike a common cold, a decrease in temperature is not observed even 2-3 days after the onset of the disease.
Initially, a viral infection develops in the first 2-3 days, and then, from 3-5 days, an infection of bacterial etiology occurs. Pneumonia becomes viral-bacterial.
Indications for research
An X-ray examination is prescribed to a patient if pneumonia is suspected. Reasons for referral for an x-ray may include the following symptoms:
- Cough (“wet”, with copious moisture and phlegm);
- wheezing on auscultation in the lungs;
- Increased levels of leukocytes and lymphocytes in the blood.
An external examination of the patient and laboratory tests are carried out simultaneously with an x-ray examination or before the procedure. Using X-rays, foci of inflammation, the location of foci, changes in the image of the lungs and roots, as well as the pathology of the location of the diaphragm are determined.
Sluggish pneumonia: symptoms and features
This type of pneumonia, which is classified as a separate category, is in most cases focal and occurs in a mild form without pronounced clinical signs. Pneumonia of this type is a complication of acute respiratory viral infection or influenza virus and has a favorable outcome. It is treated at home; difficulties can only be caused by primary diagnosis, which only includes examining the patient and collecting information.
In case of prolonged colds, the following symptoms should alert you:
- an increase in temperature two to three days after a decline;
- During the recovery period, a sudden deterioration in condition.
If there is a second “wave” of the disease, then this is a signal to seek advice from a doctor. Even without visible signs characteristic of pneumonia, such a phenomenon can be alarming and cause an x-ray to be prescribed.
Do not confuse the two concepts - sluggish and prolonged inflammation; in the second case, the disease begins acutely, and then the symptoms subside significantly.
Contraindications
In modern medicine there are no absolute or cardinal contraindications to x-ray diagnostics. However, there are some recommendations when this procedure is undesirable.

Pregnant women and children under 16 years of age undergo X-ray examination only in special cases when other diagnostic methods do not provide a complete picture and do not allow an accurate diagnosis and subsequent treatment.
This is due to the fact that radiation negatively affects the genome of a growing cell. If you still need to take X-rays, it is recommended to carry out diagnostics using the target image - the irradiation area will be much smaller.
Contraindications also include:
- presence of open wounds;
- bleeding;
- serious condition of the patient.

Latent pneumonia in children: features and symptoms
This form of pneumonia is the most dangerous, as it often occurs without the symptoms characteristic of pneumonia. However, children's lungs are affected and the condition can lead to significant complications. The main reasons for the absence of obvious signs are a significant decrease in immune functions and the body’s addiction to certain drugs.
This type of pneumonia can affect children of any age, but increased danger threatens children under three years of age who cannot talk about their feelings. Parents need to be more attentive to the baby’s condition, since unexpressed signs of the disease are still present:
- drowsiness, weakness, lethargy;
- mood swings, tearfulness;
- pale skin;
- shortness of breath during physical activity;
- lack of appetite;
- pain in various parts of the body;
- increased sweating;
- increased thirst.
Statistics show that about 1,500 children die annually due to undetected latent (silent) pneumonia.
Other methods
In addition to X-rays, the picture of the disease is studied by other clinical methods. The etiological diagnosis is made based on the study of discharge from the nose and pharynx (virological and bacteriological). Bacteriological examination of sputum is also possible. Intracellular inflammatory factors are detected using ELISA and PRC.
The need for additional methods for diagnosing pneumonia in children is explained by the specificity of the symptoms. Often the symptoms of pneumonia are confused with other childhood diseases (acute respiratory infections, bronchitis, tuberculosis, bronchiolitis).
For typical pneumonia, diagnosis and treatment are carried out by a local pediatrician. If the disease has already become complicated or is accompanied by unusual symptoms, consultation with a pulmonologist is necessary.
For a more accurate diagnosis, computer X-ray diagnostics of the lungs is performed.
Focal pneumonia in children: signs of the disease
Focal pneumonia, or bronchopneumonia, is most often a complication of ARVI. It develops within 5-7 days after infection. The disease is characterized by localization of the lesion in a limited area of the lung. This can be a single lesion, the minimum size of which is 10 mm. When infected with chlamydia, the lesions can be multiple. The primary symptoms of bronchopneumonia are very similar to those of a cold - cough and runny nose.
The development of infection leads to damage to the epithelial cover of the bronchi, and then damage to the lung tissue. After 5-7 days, a sharp deterioration in the condition occurs, the symptoms become more pronounced:
- severe cough, it can be both dry and wet;
- shortness of breath (in infants it can be observed even during sucking, in older children - with any, even minor, load;
- the skin becomes pale;
- breathing becomes noisy, with obvious participation of the chest muscles;
- body temperature rises to 38-39? C and can last for several days;
- feverish condition;
- increased heart rate;
- vomiting and nausea;
- enlarged liver;
- pain in the abdomen.
Reference materials (download)
| # | file | file size |
| 1 | Differential radiological diagnosis of respiratory and mediastinal diseases t1 1991 | 7 MB |
| 2 | Pulmonary studies and major syndromes | 199 KB |
| 3 | Diagnosis of diseases of the respiratory system. Hams | 9 MB |
| 4 | Diagnosis and treatment of environmental pneumonia. Infectious Diseases Society of America guidelines. | 833 KB |
Community-acquired (out-of-hospital) pneumonia: signs of the disease
This form of the disease occurs in the first two days after the child’s hospitalization or outside the hospital and can affect one or both pulmonary lobes. Children under 5 years of age are at risk for this lesion.
The high incidence of community-acquired or home-acquired pneumonia in children is influenced by the anatomical features of the respiratory system and the body’s weak immune defense. Children's trachea and bronchi are narrow, and this causes retention and stagnation of mucus, in which pathogenic microorganisms actively multiply. Infants spend more time lying down, which can lead to blood stagnation.
Symptoms and course of the disease depend on the type of pathogen and the location of the infection. Common signs include the following:
- cough;
- increased body temperature;
- sputum production;
- chest pain when coughing and breathing;
- general weakness;
- increased sweating at night.
The prevalence of community-acquired pneumonia is quite high. But there are no exact statistics, since many cases of the disease are not recorded due to the low population seeking medical help.