Red blood cells produced in the bone marrow are called erythrocytes. Their transport function allows you to deliver oxygen to tissues at the cellular level and take carbon dioxide to the lungs. In addition to the main functionality, they take part in water-salt metabolism and regulation of blood acidity levels. For the normal functioning of the body, their quantity must correspond to age standards.
Normal indicators
The level of red blood cells contained in the bloodstream depends on the gender and age group of the patient. For a healthy person, the following level is acceptable:
- women – 3.7-4.7*1012 per liter;
- men – 4-5.1*1012 per 1 liter.
In childhood, the concentration of corpuscles constantly changes; for each month or day of a newborn’s life, there is a certain standard. Small fluctuations are observed after the first year of life, but the values are not particularly different from the same data for adults. At 12-13 years of age, the indicator is equal to adult values.
Tests for red blood cells
A red blood cell count and cell count is usually done as part of a complete blood count (CBC).
A general blood test is the most common analysis, informative for almost any pathological process. This test can also be used to diagnose and/or monitor a number of diseases that affect the production or lifespan of red blood cells. You can take a general blood test with determination of 5 fractions of leukocytes at any CityLab medical center.
For an accurate diagnosis, the doctor may prescribe additional tests:
- Reticulocyte count - determines the number of immature red blood cells.
- Iron test - this trace element plays an important role in the production of red blood cells.
- Vitamin B12 and folic acid levels – these vitamins are also important for red blood cell production.
- A blood test for ferritin reflects iron reserves in the body.
- Serum iron, total iron-binding capacity of blood serum are additional parameters reflecting the process of iron metabolism in the body.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
Classification Features
There are two types of erythrocytosis:
- Primary hereditary – refers to genetic pathologies, is rare. The source of the development of the disease is the low susceptibility of oxygen receptors in the kidneys and increased levels of erythropoietin. A sign of the disease is a pronounced loss of strength, attacks of dizziness, a change in the standard shade of the skin and mucous membranes into purple shades, and reduced blood clotting.
- Secondary or acquired - provoked by oxygen starvation of cells, occurs against the background of neoplasms in the liver, kidneys, and respiratory organs.
If the primary form of pathology is ignored, there is a risk of vascular complications, including thrombus formation. The problem is related to changes in the rate of blood clotting.
Primary sources of increasing values
Changes of physiological nature are provoked by:
- severe emotional stress;
- severe dehydration;
- long-term sports activities;
- living in high mountain areas.
The pathological form of erythrocytosis is associated with:
- with erythremia - tumor damage to the hematopoietic organs;
- heart defects - when arterial and venous blood is mixed, there is an insufficient supply of oxygen to the tissues; to compensate for the deviation, the bone marrow begins to produce a larger number of red blood cells;
- neoplasms in the kidneys, pituitary gland, adrenal glands or liver - the organs are responsible for the disposal of old elements in the blood, the formation of the disease leads to the cessation of this function, the tests indicate a predominance of mature forms;
- diseases of the respiratory tract and heart, infectious pathologies - a large number of young or reticular types of elements are observed;
- primary pulmonary hypertension;
- Pickwick's syndrome caused by obesity, pulmonary insufficiency, high blood pressure.
Less dangerous sources of development of an increased number of red blood cells include:
- lack of digestive enzymes;
- dehydration due to heat or prolonged physical activity;
- low-quality water: with chlorine, contaminated, highly carbonated;
- vitamin deficiency or deficiency due to liver dysfunction;
- smoking.
Against the backdrop of a large number of reasons causing changes in tests, only a doctor can correctly determine the original source of the deviation.
ERYTHROCYTOSIS
Erythrocytosis
(Greek erythros red + kytos receptacle, here - cell + -osis; obsolete
polyglobulia
) - an increase in the hemoglobin content and the number of red blood cells in the blood.
There are absolute erythrocytosis, in which the mass of circulating red blood cells is increased, and relative, caused by a decrease in blood plasma volume.
Under physiological conditions, erythrocyte balance in the body is maintained by the interaction of factors such as blood oxygen saturation, the content of erythropoietin (see) in the blood, the functional capacity of the bone marrow and the mass of circulating erythrocytes.
For the first time, the possibility of the existence of compensatory erythrocytosis developing during high-altitude hypoxia was pointed out by P. Bert in 1878. Subsequently, the presence of erythrocytosis was noted in a number of diseases.
Based on their origin, absolute erythrocytosis is divided into primary (hereditary), caused by gene mutations, and secondary, or symptomatic (acquired). Secondary erythrocytosis occurs in various somatic diseases as a result of the indirect effect of erythropoietin on erythrocytopoiesis.
Absolute erythrocytosis (both primary and secondary) is also divided into hypoxemic and non-hypoxemic. Absolute hypoxemic erythrocytosis, caused by hypoxemia and in response to it by physiologically adequate increased production of erythropoietin, can be observed as a result of a decrease in oxygen transport in chronic lung diseases, congenital “blue” heart defects (see Congenital heart defects), stay in high mountains (see. Mountain sickness), methemoglobinemia (see), carboxyhemoglobinemia (see Carbon monoxide), Pickwickian syndrome (see). They can be observed in the case of a decrease in the release of oxygen in hemoglobinopathies (see) with increased affinity for oxygen and a hereditary decrease in the content of 2,3-diphosphoglyceric acid in erythrocytes.
Absolute non-hypoxemic erythrocytoses, not associated with hypoxemia and caused by physiologically inadequate increased production of erythropoietin, occur with kidney lesions such as cancer, polycystic disease, renal artery stenosis (see Kidneys), hydronephrosis (see), after kidney transplantation, as well as with tumors accompanied by the presence of ectopic foci of erythropoietin production, for example, with adrenal adenoma (see Adrenal glands, tumors), chromaffinoma (see), fibromyoma (see). Excessive production of erythropoietin is observed in so-called hereditary familial erythrocytosis (see Hereditary familial erythrocytosis).
Relative erythrocytosis is often observed in arterial hypertension, in smokers, in people who abuse alcohol or are in a state of chronic stress.
Manifestations of erythrocytosis are varied and, as a rule, are determined by the characteristics of the underlying pathological process, and therefore their symptoms may vary. Usually there is red cyanosis of the skin and visible mucous membranes, moderate hepato- and splenomegaly, varicose veins, and sometimes thrombosis and bleeding. The hemogram reveals an increase in red blood (See Hemogram) and hematocrit (see Hematocrit number). White blood cell and platelet counts are usually within normal limits.
Erythrocytosis is established on the basis of anamnesis, signs of diseases that may be accompanied by erythrocytosis, blood counts, and trephine biopsy data of the ilium (see Trephine biopsy).
Erythrocytosis should be distinguished from polycythemia, which is characterized by an increase in the number of red blood cells, leukocytes and platelets, panmyelosis in the bone marrow, splenomegaly (see Polycythemia); in difficult cases, the content of erythropoietin is determined, which is increased in most cases with erythrocytosis and low with polycythemia.
There are no pathogenetically based methods for treating absolute primary erythrocytosis. In case of absolute secondary erythrocytosis, it is necessary to first clarify the diagnosis of the underlying disease. Elimination of the cause of secondary erythrocytosis ensures its complete elimination.
Symptomatic treatment to remove excess red blood cells includes bloodletting 2-3 times a week with the immediate removal of 400-500 ml of blood (a total of 3-4 bloodlettings per course). In case of hypoxemic erythrocytosis caused by congenital heart defects and hemoglobinopathies, special care must be taken with bloodletting, since these erythrocytosis have a compensatory value (the hematocrit number is reduced to 52-55%, guided by the patient’s condition; in this case, oxygen therapy is advisable). In case of erythrocytosis caused by kidney damage or kidney transplantation, bloodletting is carried out until the hematocrit normalizes. It is advisable to combine bloodletting with disaggregants (chimes, rheopolyglucin), which are prescribed during the period of bloodletting therapy and for two weeks after the end of treatment.
Patients with erythrocytosis require constant medical observation:
Bibliography:
Demidova A.V. Analysis of the causes of diagnostic errors in red blood. Modern approaches to the differential diagnosis of erythremia and secondary erythrocytosis, Ter. arch. vol. 56, no. 6, p. 147, 1984; Hereditary anemias and hemoglobinopathies, ed. Yu. N. Tokareva et al., p. 312, M., 1983; Guide to Hematology, ed., A. I. Vorobyova and Yu. I. Lorie, p. 222, M., 1979; Bert P. La pression barom^t-rique, P., 1878; Donati R. M. a. o., Erythrocythemia and neoplastic tumors, Ann. intern. Med., v. 58, p. 47, 1963; Hematology, ed. by W. J. Williams ao, p. 673, NY 1983; Smith JR a., Landaws A. Smoker's polycythemia, New Engl. J. Med., v. 298, p. 6, 1978; Weatherall DJ Polycythemia resulting from abnormal hemoglobins, ibid., v. 280, p. 604, 1969.
Yu. N. Tokarev.
Changes in childhood
A pathological increase in the number of red blood cells in children is associated with various factors:
- with a low level of oxygen in maternal blood - the anomaly manifests itself in newborns;
- regular exposure of the baby to tobacco smoke (passive smoking);
- living in high mountain areas;
- regular sports activities.
A list of probable sources of deviation in children is presented:
- congenital heart defects;
- bone marrow dysfunction;
- hypertension in the pulmonary circulation;
- blood pathologies;
- obstructive pulmonary lesions with a chronic course;
- acute bronchitis, rhinitis or allergies;
- obesity of the last two degrees;
- dehydration caused by vomiting or diarrhea;
- disruption of the adrenal cortex.
Serious diagnoses associated with changes in the number of red blood cells include cancer of the kidneys and liver. Erythrocytosis is not an independent disease; it indicates latent pathologies or the presence of external influence factors.
What is secondary erythrocytosis and why is it dangerous?
In addition to hemoglobin, doctors always look at the content of red blood cells in the blood, because hemoglobin does not circulate through the bloodstream on its own, it is transported by red blood cells. If the hemoglobin level is high, then the number of red blood cells in the blood is also increased.
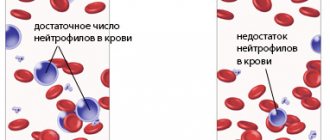
There is primary or true erythrocytosis, which is caused by congenital disorders in the regulation of red blood cell production. A similar situation occurs when the bone marrow malfunctions, which grows and begins to produce an excessive amount of red blood cells (the so-called erythremia or Vaquez disease). However, such diseases are quite rare.
Much more often you can find the so-called secondary erythrocytosis, which, most often, is a symptom of diseases that lead to disruptions in the normal functioning of the respiratory system. In this case, increased production of red blood cells by the bone marrow is a compensatory mechanism that improves the delivery of oxygen to tissues in conditions of insufficient oxygen supply to the blood through the lungs. In this way, the body tries to protect itself from hypoxia.
But in fact, if the problem of hypoxia is solved to some extent by increasing hemoglobin and the number of red blood cells, then a new problem appears: an increase in their number leads to an increase in blood viscosity. And when the blood thickens, the likelihood of blood clots increases significantly. This is not only ordinary thrombophlebitis, but in the future – deadly pulmonary thromboembolism, stroke or myocardial infarction, the risk of which is significantly increased.