Alloimmune anti-erythrocyte antibodies (including anti-Rhesus antibodies), titer
This is the detection of antibodies to a specific protein located on the surface of red blood cells - the Rh factor. These antibodies are one of the main causes of hemolytic disease of newborns.
Synonyms Russian
Anti-Rhesus antibody titer, indirect Coombs test.
English synonyms
Anti Rh, Rh Typing.
Research method
Agglutination reaction.
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
Do not smoke for 30 minutes before the test.
General information about the study
The Rh factor (Rh) is inherited and is a protein on the surface of red blood cells. Those people who have it (and this is the majority, about 85%) are called Rh positive. However, some people who are Rh negative lack this protein. Negative Rh does not affect the health of the person himself. However, problems can arise between the mother and the baby she is carrying if they have different Rh factors or if the mother develops antibodies that react with factors in the baby's blood cells. The most common example: a woman with a negative Rh factor (Rh-) is pregnant with a child with a positive Rh factor (Rh+). This woman's immune system may develop antibodies against her baby's Rh-positive blood. Despite this, the firstborn is quite rarely sick, because the mother’s immunity does not come into contact with the child’s blood until birth. However, antibodies produced during the first pregnancy can freely cross the placenta in subsequent pregnancies and thus create problems for the Rh-positive baby.
To reduce the likelihood that an Rh- mother will develop antibodies to the blood of an Rh+ baby, she is sometimes given injections of anti-D-gamma globulin 28-34 weeks before giving birth, as well as during the first time after the birth of an Rh-positive baby. Additional injections may be required during pregnancy if there is a suspicion that the mother's blood has come into contact with the blood of the Rh+ fetus (for example, during puncture of the amniotic sac or abdominal trauma). The injection of the antibody clears the baby's blood of any antigens present and thus prevents the mother's immune system from reacting to them.
What is the research used for?
The anti-Rh antibody test is used primarily to detect antibodies to the Rh factor. An Rh-negative mother and an Rh-positive father can conceive an Rh+ child, and there is a chance that some of the baby's red blood cells will enter the mother's bloodstream during pregnancy and childbirth. In response to foreign Rh+ red blood cells, the mother's body produces anti-Rh antibodies. They pose a threat to this mother's future children. Every woman before or during pregnancy must be tested for the Rh factor. It will help determine whether her blood is Rh-negative, and also determine whether the Rh-negative woman has acquired antibodies against Rh+ red blood cells. A pregnant woman whose body has not yet formed anti-Rhesus antibodies can use immunoglobulin injections to prevent their appearance. An Rh-negative woman during pregnancy should undergo additional treatment with immunoglobulins immediately after any situation where fetal blood could enter her bloodstream. Analysis for anti-Rh antibodies helps to identify these processes and promptly prescribe and adjust treatment to prevent Rh conflict.
When is the study scheduled?
- If necessary, prescribe treatment with immunoglobulin injections to a pregnant woman with a negative Rh factor.
- In the case when the red blood cells of the fetus could enter the bloodstream of a pregnant woman with an Rh-negative factor, if she had miscarriages, ectopic pregnancy, artificial birth or abortion, puncture of the amniotic sac, abdominal trauma, artificial change in the position of the fetus.
- The test may be prescribed to a woman who is Rh negative, who has given birth to a Rh positive child and has been treated with immunoglobulin injections, to determine whether the child has antibodies against Rh+ red blood cells.
What do the results mean?
Reference values: negative.
Positive result
- Antibodies have been detected, there is a possibility of Rh conflict.
Negative result
- Antibodies were not detected, the likelihood of Rh conflict is low.
Proper treatment with anti-D-gamma globulins prevents the formation of anti-Rhesus antibodies in almost all pregnant women with a negative Rh factor. However, such prevention does not work if the woman has already formed anti-Rhesus antibodies.
Important Notes
- Anti-Rhesus antibodies are sometimes present in very low, undetectable quantities.
- The blood of young children can react with the antibody, even if the test is negative.
- If the mother has had an anti-D-gamma globulin injection within the last six months, the antibody test may give positive results.
- A woman who is Rh negative does not need to be treated with anti-D-gamma globulin injections if the child's father is also Rh negative, since the child will also be Rh negative, so there is no risk of hemolytic disease.
Antibodies to erythrocyte antigens and Rh factor
Antibodies to erythrocyte antigens and Rh factor
- study of antibodies to the most important antigens of erythrocytes, primarily the Rh factor, which indicate sensitization of the body to these antigens.
Rh antibodies belong to the so-called alloimmune antibodies. Alloimmune antibodies
are antibodies to red blood cell antigens. Alloimmune anti-erythrocyte antibodies appear in the blood after transfusion of immunologically incompatible donor blood. Antibodies can appear during pregnancy when fetal red blood cells, carrying paternal antigens that are immunologically foreign to the mother, penetrate through the placenta into the woman’s blood. Non-immune Rh-negative people do not have antibodies to the Rh factor.
Rh factor (Rh)
- protein on the surface of red blood cells. Acquired by inheritance. It is present in most people (85%), which is why they are called Rh positive. There are also people who lack this protein, they are called Rh negative accordingly. The absence of Rhesus does not in any way affect the health of the person himself.
However, the difference in Rh factors can pose a significant danger during pregnancy. The difference in Rhesus of the mother and child can contribute to the formation of antibodies that react with the child’s red blood cells.
An anti-Rh antibody test is prescribed primarily to detect antibodies to the Rh factor, since they pose a threat to the mother's future children.
In accordance with medical protocols, every woman must be tested for the Rh factor before or during pregnancy. The test will help determine whether her blood is Rh negative and will also determine whether the Rh negative woman has acquired antibodies against Rh+ red blood cells. Analysis for anti-Rh antibodies will help identify specific processes and timely prescribe and adjust therapy to prevent Rh conflict.
Indications:
- pregnancy (prevention of Rh conflict);
- monitoring pregnant women with negative Rh factor;
- miscarriage;
- hemolytic disease of the newborn;
- preparation for blood transfusion.
Preparation
No special preparation is required.
It is recommended that blood be taken no earlier than 4 hours after the last meal. Interpretation of results
Units of measurement: U/ml. Reference values: negative.
Positive result:
- sensitization to Rh antigen or other erythrocyte antigens.
When alloimmune anti-erythrocyte antibodies are detected, their semi-quantitative determination is carried out. The result is given in titers (the maximum dilution of the serum at which a positive result is still detected).
SCREENING OF ANTIERYTHROCYTE ANTIBODIES AND OTHER PRACTICAL ISSUES IN IMMUNOSEROLOGY
| CwCDee | + | + | 0 | 0 | + | + | 0 | + | 0 | + | + | 0 | + | 0 | 0 | + | + | + | 0 | + | + | 0 | + | M | |
| II | ccDEE | + | 0 | + | + | 0 | 0 | 0 | + | 0 | + | 0 | + | + | 0 | + | 0 | + | 0 | + | + | 0 | 0 | + | M |
| III | ccddee | 0 | 0 | 0 | + | + | 0 | + | + | 0 | + | 0 | + | 0 | + | 0 | + | + | + | 0 | + | + | 0 | + | M |
table 2
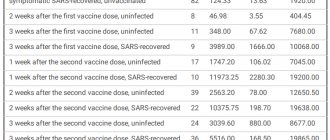
Results of antibody screening in donors using gel and gelatin methods
| № | FULL NAME. | Floor | Phenotype | Result | Possible antibody specificity | |||
| Gelatin | Gel | |||||||
| I | II | III | ||||||
| 1 | I.V.V. | m | сcddee Cotres | — | + | + | — | D,Jka |
| 2 | H.O.F. | and | сcddee Cotres | — | + | + | — | D,Jka |
| 3 | WILLOW. | m | сcddee Cotres | — | + | + | — | D,Jka |
| 4 | D.G.P. | and | сcddee Cotres | — | + | + | — | D,Jka |
| 5 | E.A.V. | m | CcDee Cotres | — | + | + | — | Jka |
| 6 | T.A.V. | m | CcDee Cotres | — | + | + | — | Jka |
| 7 | MMM. | m | CCDee Kotr | — | + | + | — | Jka |
| 8 | G.A.A. | and | D Cotr | + | ++ | ++ | — | |
Table 3
Results of antibody screening in patients using gel and gelatin methods
| № | FULL NAME. | date | Phenotype | Result | Variants of antibodies to antigens | |||
| Gelatin | Gel | |||||||
| I | II | III | ||||||
| 1. | K.L.A. | 06.07.03 | CCDee Kotr | — | + | — | — | Fya, Leb |
| 2. | S.N.V. | 30.12.03 | сcddee Kotr | — | + | + | — | D,Jka |
Table 4
Issues of ensuring compatibility of donor and recipient with respect to Kell system antigens in the current documents of the Russian Ministry of Health
| Index | Source (according to the list of references) | ||
| 2 | 3 | 6 | |
| Determination of K antigen (K1) in a donor | Every time | Not regulated | Once |
| Determination of antigen K (K1) in the recipient | Not regulated | Not regulated | If necessary |
| Use of K+ red blood cells is prohibited | K-negative patients | Kell can be transfused into positive recipients. | Possible (K-) for male patients, provided they do not have alloantibodies to the K antigen. Not possible for women of childbearing age and children with K negative affiliation |
Immunological incompatibility of maternal and fetal blood
the Rh factor may occur.
, less often according to
the AB0 system
and even less often according to some other (
Kell, Duffy, Lutheran, Lewis system, PP system
) blood factors. As a result of this incompatibility, hemolytic disease of the fetus and newborn occurs.
Rh factor and hemolytic disease
Rh factor (Rh) is a protein found primarily in human red blood cells and in much smaller quantities in white blood cells and platelets. There are several types of Rh factor. So antigen-D is present in the blood of 85% of people. Antigen C (Rh') is found in the blood of 70% of people, and antigen E (Rh") is present in 30% of people. Blood that lacks the listed antigens, which are types of the Rh factor, is Rh negative.
Most common hemolytic disease of the fetus
and the newborn arises due to an immunological conflict due to the incompatibility of the blood of mother and fetus for factor D. In this case, the maternal blood must be Rh-negative. And the fetal blood contains the Rh factor. Hemolytic disease of the fetus and newborn can also occur when the blood of the mother and fetus is incompatible according to the blood group (according to the ABO system). The grouping of human blood is determined by the presence of certain antigens in it. Thus, the presence of antigen “A” in the blood determines blood group II (A). The presence of antigen “B” - III (B) blood group. The combined presence of antigens “A” and “B” determines blood group IV (AB). In the absence of both antigens, a person’s blood group is determined to be I (0). Immunological incompatibility most often manifests itself if the mother has blood group I (0), and the fetus has blood group II (A) or III (B). Fetal blood cells containing the Rh factor or group antigens and having the corresponding antigenic activity penetrate into the maternal bloodstream. As a result, the woman is immunized, which is accompanied by the production in her body of either anti-Rh antibodies or antibodies against group antigens.
Hemolytic disease of the fetus and newborn develops as a result of immunization of the maternal body
, which occurs either already during the first pregnancy with a fetus with Rh-positive blood or with the presence of corresponding group antigens in its blood, or after a transfusion of Rh-positive blood. Most often, elements of the fetal blood containing the corresponding antigens enter the maternal bloodstream during childbirth, especially during surgical interventions, when a cesarean section or manual separation of the placenta and discharge of the placenta are performed. The entry of fetal blood elements into the maternal bloodstream and subsequent immunization of the woman is also possible during pregnancy if the integrity of the placental villi is disrupted, which happens with toxicosis of pregnant women, threatened miscarriage, placenta previa, placental abruption, intrauterine fetal death.
Taking into account that the Rh factor is formed from the very first days of pregnancy, and red blood cells are formed in the first weeks of pregnancy, their entry into the maternal body and immunization are possible during abortion or ectopic pregnancy. After the first pregnancy, about 10% of women are immunized.
Immune antibodies
, which are produced in the woman’s body, penetrate back into the bloodstream of the fetus and affect its red blood cells. In this case, red blood cells are destroyed, which entails the formation of indirect toxic bilirubin, anemia and oxygen starvation (hypoxia). The fetus develops hemolytic disease. The structure and function of the fetal liver is disrupted, protein production in the fetal body is reduced, and blood circulation in the fetal body is disrupted with symptoms of heart failure. In the fetus, excess fluid accumulates in the body, which manifests itself in the form of edema and ascites. Brain tissue is often affected. The development of hemolytic disease of the fetus is possible as early as 22-23 weeks of pregnancy.
Diagnosis of hemolytic disease
Diagnosis of hemolytic disease must be comprehensive, using a number of diagnostic techniques, and is based on identifying signs indicating maternal immunization, determining antibodies and their titer, assessing the condition of the fetus and amniotic fluid indicators. The results of just one test cannot serve as an objective and reliable indicator of a possible complication and require supplementation with the results of other research methods.
If in a conversation with a woman with Rh-negative blood
or with I (0) blood group, it turns out that she was given donor blood without taking into account the Rh or group affiliation, and also if she had spontaneous abortions in the late stages or there was fetal death in previous pregnancies, or the birth of a child with icteric anemic or edematous form, then these factors are prognostically unfavorable from the point of view of a high risk of fetal damage during this pregnancy.
One of the simple ways to determine the nature of the course of pregnancy, the rate of growth and development of the fetus and the increase in the volume of amniotic fluid is to measure the height of the uterine fundus (UF) above the pubic symphysis and measure the length of the abdominal circumference. It is advisable to carry out these measurements over time every two weeks from the second trimester of pregnancy. An excessive increase in these indicators in comparison with the normative ones for a given stage of pregnancy, together with the results of other studies, allows us to suspect the presence of an existing pathology.
Determination of antibodies in the blood of a pregnant woman
has a relative diagnostic value and should be used to identify this pathology only in combination with other diagnostic tests. An important sign is the magnitude of the antibody titer and its change as pregnancy progresses. The antibody titer corresponds to the highest serum dilution at which it is still able to act (agglutinate) Rh-positive red blood cells (antibody titer can be 1:2, 1:4, 1:8, 1:16, etc.). Accordingly, the higher the titer, the more antibodies and the less favorable the prognosis.
During pregnancy, the antibody titer may increase, remain unchanged, decrease, and there may also be an alternating rise and fall in the antibody titer. In the latter case, the likelihood of fetal disease is greatest.
Assessment of the condition of the fetus and feto-placental complex
To assess the condition of the fetus and feto-placental complex, instrumental diagnostic methods such as cardiotocography (CTG) and ultrasound can be used. According to CTG data, in case of fetal suffering, there are clear signs of fetal heart rhythm disturbances, slowing of heartbeats, monotonous rhythm, etc. An ultrasound examination evaluates the size of the fetus, the condition of its internal organs, the structure and thickness of the placenta, and the volume of amniotic fluid. The functional activity of the fetus is also determined and, using Doppler sonography, the intensity of blood flow in the mother-placenta-fetus system is studied.
Ultrasonography
in women with expected hemolytic disease of the fetus should be carried out at 20-22 weeks, 24-26 weeks, 30-32 weeks, 34-36 weeks. and shortly before delivery. Until 20 weeks of pregnancy, signs of hemolytic disease are not detected echographically. Repeated studies are necessary to exclude dynamic hemolytic disease of the fetus. For each pregnant woman, the timing of repeated scans is determined individually; if necessary, the interval between studies is reduced to 1-2 weeks.
Whereas in hemolytic disease of the fetus, swelling of the placenta occurs
, then its thickening by 0.5 cm or more may indicate a possible disease of the fetus. However, other complications should be excluded, in which thickening of the placenta can also occur (for example, intrauterine infection or diabetes mellitus).
For hemolytic disease of the fetus, along with thickening of the placenta, an increase in the size of its abdomen is possible in comparison with the chest and head of the fetus. This increase is due to the excessive size of the fetal liver, as well as excessive accumulation of fluid in its abdominal cavity (ascites). Swelling of the fetal tissues manifests itself in the form of a double contour of its head. With severe fetal hydrops, there is also an accumulation of fluid in other cavities (hydrothorax, hydropericardium), and signs of swelling of the intestinal walls.
Ultrasound scanning also evaluates the behavioral reactions of the fetus (motor activity, respiratory movements, fetal tone). If its condition is disturbed, corresponding pathological reactions from these indicators are noted. According to Doppler ultrasound, there is a decrease in the intensity of blood flow in the feto-placental complex.
Determination of the optical density of bilirubin in amniotic fluid is of great diagnostic importance.
, fetal blood type, antibody titer. On the eve of delivery, it is advisable to examine amniotic fluid to assess the degree of maturity of the fetal lungs.
To study amniotic fluid, starting from 34-36 weeks of pregnancy, amniocentesis is performed, which is a puncture of the uterine cavity to take a sample of amniotic fluid. The procedure is carried out under ultrasound control with anesthesia and in compliance with all rules of asepsis and antisepsis.
Amniocentesis
can be performed either through the anterior abdominal wall or through the cervical canal. The puncture site is chosen depending on the location of the placenta and the position of the fetus. Possible complications in this case may be: increased uterine tone, placental abruption, bleeding, rupture of amniotic fluid and the onset of labor, development of inflammation.
Based on the optical density of bilirubin in amniotic fluid, if it is more than 0.1, the possible severity of fetal hemolytic disease is assessed. If this indicator is more than 0.2, one can expect the birth of a child with a moderate to severe form of hemolytic disease.
Detection of fetal blood type
amniotic fluid test is one of the tests that determines the prognosis for the fetus. More often, one can expect the development of hemolytic disease due to incompatibility of the Rh factor, with the same blood group of the mother and fetus.
It is important to determine the blood group if the development of an AB0-conflict pregnancy
. A significant diagnostic test is the determination of antibody titer in amniotic fluid.
To study fetal blood, puncture of the umbilical cord vessels is used ( cordocentesis
) under ultrasound control. A study of the fetal blood obtained in this way makes it possible to determine its blood type and Rh status, assess the level of hemoglobin, serum protein and a number of other indicators that reflect the presence and severity of the complication.
As part of pregnancy management, all patients and their husbands should be determined to have their Rh and blood type determined when they first see a doctor, regardless of whether childbirth is imminent or termination of pregnancy is planned. In pregnant women with the first blood group, if their husbands have a different blood group, it is necessary to conduct a test to determine group antibodies. Pregnant women with Rh-negative blood must be examined for the presence of antibodies and their titer once a month until 20 weeks, and then once every 2 weeks. If a pregnant woman with Rh-positive blood has an indication of the birth of a child with a hemolytic disease, the blood should be examined for the presence of group immune antibodies, as well as for “anti-c” antibodies if the husband’s blood contains the “c” antigen. The presence of Rh sensitization in pregnant women is not an indication for termination of pregnancy.
Prevention and treatment of hemolytic disease of the fetus
All pregnant women with Rh-negative blood, even in the absence of antibodies in their blood, as well as in the presence of AB0 sensitization, should undergo 3 courses of nonspecific desensitizing therapy
lasting 10-12 days, in periods of 10-22, 22-24, 32-34 weeks.
As part of nonspecific desensitizing therapy, the following is prescribed: intravenous administration of 20 ml of 40% glucose solution with 2 ml of 5% ascorbic acid solution, 100 mg of cocarboxylase; orally rutin 0.02 g 3 times a day, theonicol 0.15 g 3 times a day or methionine 0.25 g and calcium gluconate 0.5 - 3 times, iron supplements, vitamin E 1 capsule. Antihistamines are used at night: diphenhydramine 0.05 or suprastin 0.025.
In case of complicated pregnancy: threat of miscarriage, early toxicosis of pregnant women, gestosis, etc., patients should be hospitalized in the department of pathology of pregnant women, where, along with treatment of the underlying disease, a course of desensitizing therapy is carried out.
Pregnant women who have a high titer of Rh antibodies
, and they have a history of spontaneous miscarriages or delivery of a fetus with an edematous or severe form of hemolytic disease, it is recommended to use
plasmapheresis
. This procedure removes antibodies from the blood plasma. Plasmapheresis is carried out once a week under the control of antibody titer, starting from 23-24 weeks. pregnancy, before delivery.
Hemosorption is also used to treat hemolytic disease of the fetus.
using activated carbon to remove antibodies from the blood and reduce the degree of Rh sensitization. Hemosorption is used in pregnant women with an extremely complicated obstetric history (repeated miscarriages, stillbirth). Hemosorption begins at 20-24 weeks in the hospital, with an interval of 2 weeks.
Treatment of hemolytic disease of the fetus during pregnancy is also possible by blood transfusion to the fetus under ultrasound guidance
.
Pregnant women with Rh sensitization
hospitalized in the maternity hospital at 34-36 weeks. pregnancy. With AB0 - sensitization, hospitalization is carried out at 36-37 weeks. If there are appropriate indications indicating a pronounced nature of the complication, hospitalization is possible at an earlier date.
In the presence of hemolytic disease of the fetus, early delivery is advisable due to the fact that towards the end of pregnancy the flow of antibodies to the fetus increases. In case of severe hemolytic disease of the fetus, pregnancy is terminated at any time during pregnancy. However, in most cases, pregnancy can be prolonged until an acceptable delivery date. As a rule, delivery is carried out through the natural birth canal. Caesarean section is performed in the presence of additional obstetric complications.
During childbirth, careful monitoring of the condition of the fetus is carried out, hypoxia is prevented
. Immediately after birth, the baby is quickly separated from the mother. Blood is taken from the umbilical cord to determine the content of bilirubin, hemoglobin, the child’s blood type, and his Rh status. A special test is performed to identify the newborn's red blood cells associated with antibodies.
Treatment of hemolytic disease of the newborn
In hemolytic disease of the newborn, there are three forms: anemic, icteric and edematous.
.
When treating the anemic form of hemolytic disease of newborns with hemoglobin levels less than 100 g/l, transfusions of Rh-positive erythromass corresponding to the blood type of the newborn are performed. To treat the icteric-anemic form of hemolytic disease of newborns, exchange transfusions, phototherapy, and infusion therapy
. In severe cases of hemolytic disease of the newborn, exchange transfusions are performed repeatedly in combination with therapy aimed at reducing intoxication caused by indirect bilirubin.
The action of phototherapy or light therapy is aimed at destroying indirect bilirubin in the superficial layers of the newborn's skin under the influence of a fluorescent or blue lamp (wavelength 460A). When performing infusion therapy, solutions of hemodez, glucose, albumin, and plasma are injected intravenously in various combinations.
Treatment of the edematous form of hemolytic disease of the newborn consists of immediate replacement transfusion of single-group Rh-negative red blood cell mass. At the same time, dehydration therapy is carried out aimed at eliminating edema.
To prevent hemolytic disease of the fetus and newborn, it is necessary that with any blood transfusion it is of the same group and similar in Rhesus status.
First pregnancy and Rhesus conflict
It is important to maintain the first pregnancy in women with Rh-negative blood
.
It is necessary to prevent and treat complicated pregnancy, as well as carry out desensitizing therapy. For primigravid women with Rh-negative blood who are not yet sensitized to the Rh factor, anti-Rh immunoglobulin is administered
. After childbirth, the administration of immunoglobulin is repeated in the first 48-72 hours.
Make an appointment with specialists by calling a single call center:
+7(495)636-29-46 (metro stations “Schukinskaya” and “Street 1905 Goda”). You can also make an appointment with a doctor on our website, we will call you back!