Testosterone analysis: how to prepare
• Since physical activity stimulates the production of testosterone, you should avoid it the day before the test. This applies to intense sports and regular weight lifting. Smoking should also be avoided.
• For children and men, the test can be taken in the morning, on any day, for women - on the 6-7th day of the menstrual cycle (unless the attending physician has prescribed other dates for diagnostic purposes).
• The most favorable time to take blood for testing is from 8 to 11 am. A prerequisite is that blood is donated on an empty stomach, that is, after 8 and no more than 14 hours without food. You can only drink water.
General information
Physiological processes are regulated by hormones, one of which is testosterone. In the male body, it ensures the development and formation of the reproductive system, determines sexual behavior, affects libido and the process of spermatogenesis. In women, the hormone is responsible for the level of accumulation of fat and muscle mass, the growth and development of the body, and the functionality of the reproductive system.
Even minor deviations in testosterone production lead to serious consequences, in particular, infertility and cancer. A testosterone level test allows you to diagnose these and other pathologies, as well as timely prescribe hormone replacement therapy.
In men, testosterone is secreted in the testes. Its levels rise sharply during puberty and can persist for up to 60 years. When the secretory function of the testes in men fades, the so-called “male menopause” occurs. If the concentration of testosterone decreases not for physiological, natural reasons, then first of all it is assumed:
- abnormal development of the reproductive system;
- decreased fertility, i.e. fertilization ability;
- violation of potency.
Often, testosterone deficiency (hypogonadism) is a consequence of endocrine disorders and congenital syndromes (Kallmann, Prader-Willi, Kleifelter, etc.).
An increase in hormone levels also indicates the presence of pathologies:
- oncology of the testicles or adrenal glands;
- negative consequences of taking steroids during the formation of muscle mass;
- premature puberty;
- hyperfunction of the thyroid gland, etc.
In women, testosterone is produced by the ovarian follicles as well as the adrenal cortex. Peak concentrations occur during ovulation and the 3rd trimester of pregnancy. Increased hormone levels in other cases may indicate
- about polycystic ovary syndrome,
- about neoplasms in the ovaries or adrenal glands.
With the onset of menopause in women, testosterone production decreases, which leads to gradual decline of the body, in particular, to the decline of reproductive function.
In the blood, testosterone is found in free and bound states. Only 2% of the hormone circulates in a free form, and the rest is bound (44% binds to the globulin protein, and 54% to albumin or other proteins). To make a diagnosis, the doctor prescribes a test for total testosterone, and, if necessary, supplements it with a test for SHBG (sex hormone binding globulin).
Testosterone analysis explanation
Analysis for testosterone in men: the norm for men from 16 to 50 years old is 5.13 – 30.43 nmol/l. Testosterone levels in older men decrease and remain within the range of 5.4 – 19.5 nmol/l.
Testosterone analysis in women: the norm in women and girls from 13 years of age and throughout their reproductive years is between 0.36 and 1.97 nmol/l. During pregnancy, testosterone levels can be 3-4 times higher than normal. After menopause, the hormone level may decrease slightly and range from 0.28 to 1.22 nmol/l.
Testosterone analysis in children: the norm for boys in the first six months of life can vary from a minimum amount of 0.3 to a high concentration of 10.36 nmol/l. From 6 months to 9 years, testosterone levels usually remain stable below 1.24 nmol/L. For teenage boys, total testosterone is considered normal if it is below 15.41 nmol/L.
In girls under 13 years of age, testosterone levels usually do not exceed 0.98 nmol/l.
We must also remember that all people usually have hormone levels that fluctuate throughout the day: from the maximum value in the morning to the minimum in the evening.
All tests for testosterone should be interpreted by a doctor who takes into account not only the generally accepted average values of indicators, but also other factors that can affect the concentration of total testosterone in the blood.
Testosterone: total or free? How not to make a mistake in making a diagnosis
In everyday medical practice, a blood test for testosterone is performed in cases of suspected hypogonadism in men, hirsutism and virilism in women, premature sexual development (or its delay) in children, and suspected testicular tumors in men or ovarian tumors in women [1].
Typical symptoms and manifestations of testosterone deficiency syndrome (TDS) in men have been known for almost 70 years, these include erectile dysfunction, decreased libido, weakness, depression, anxiety, irritability, impaired concentration, joint pain, night sweats, thinning and dry skin, premature aging. However, it is still unknown why there is no good correlation between the degree of manifestations of TSD and the level of testosterone and other androgens in the blood [2].
In cases where the clinical manifestations of SDT and the level of total testosterone (TT) in the blood do not agree with each other, to confirm the diagnosis of hypogonadism, it is advisable to conduct a test for free testosterone not associated with carrier proteins, primarily with sex hormone binding globulin (SHBG) [3]. Direct methods for determining free testosterone in the blood are associated with technical difficulties and are not suitable for routine use; instead, computational methods for estimating the level of free testosterone (cFT) have been proposed [1, 4-7]. It has been shown that low cFT values, even with normal TT values, are consistent with symptoms of TSD and are characteristic of older men, while normal cFT values with low TT are not associated with these symptoms, and are rather characteristic of young obese people [8].
In clinical practice, extraction-free methods for determining TT using automatic immunochemical analyzers (Roche, Siemens, Abbott) are widely used. In a number of cases, the reliability of the results obtained is called into question [9]. However, the chromatography-mass spectrometry method proposed as an alternative is not yet widespread enough in clinical laboratories, and many doctors do not have a clear understanding of the differences between this method and immunochemical analysis [10].
A comparative blood test for testosterone (Table 1, Fig. 1) using immunochemiluminescence (ICL) and liquid chromatography-mass spectrometry (LC-MS) methods, in full agreement with previously published data, showed that the maximum differences are for low testosterone values, characteristic for women, reach 100%, with a tendency towards overestimation of the result by the ICL method; for high testosterone values, typical of healthy men, the relative error is smaller - about 55%, while the ICL method tends to underestimate the results. Interestingly, in quality control samples that are obtained by pooling serum, the LCL method systematically overestimates testosterone results [11].
Perhaps the inconsistency between laboratory results of TT obtained by immunochemical methods and clinical manifestations in SDT is due precisely to an analytical error in determining TT.
The error in determining the calculated value of free testosterone is determined by the sum of errors in measuring the concentrations of transporter proteins and their ligands, as well as the error in determining the corresponding binding constants [5]. A nomogram using the Vermeulen method allows you to clearly assess the dependence of the cFT value on the values of SHBG and TT (Fig. 2). It is obvious that the calculated cFT value is directly proportional to the concentration of TT, and, therefore, for diagnostic purposes for both total and free testosterone, it is advisable to use the results of the reference research method, that is, LC-MS. An alternative to serum testosterone for assessing androgen status in clinical studies can be a study of testosterone concentration in saliva, which serves as an additional diagnostic criterion [12, 13].
Summarizing the above, we believe that in the near future the following diagnostic algorithm will be adopted as the method of choice for assessing the androgen status of men with suspected TSD:
- Determination of total testosterone by LC-MS;
- Determination of sex hormone binding globulin using traditional enzyme immunoassay methods;
- Determination of free testosterone by calculation methods using data on the content of total testosterone obtained by LC-MS;
- Determination of [free] testosterone in saliva by LC-MS.
Table 1. Estimates of the consistency of total testosterone measurements by CL and LC-MS in the blood serum of men (M), women (F) and in quality control (QC) samples. Note: the average difference characterizes the systematic discrepancy, the standard deviation characterizes the degree of scattering of the results.
| Group | AND | M | QC |
| N, people | 109 | 205 | 19 |
| Average difference (LC-MS - ICL), nmol/l | -0,06 | 0,11 | -0,32 |
| Standard deviation of the mean difference, nmol/l | 0,42 | 0,25 | 0,24 |
Rice. 1 Bland-Altman plot: comparison of two methods (mass spectrometry and immunochemiluminescence) for measuring testosterone in the serum of men (M), women (F), and quality control (QC) samples.
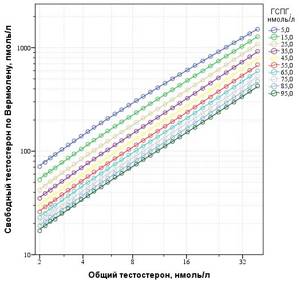
Rice. 2 Nomogram for determining free testosterone in the blood according to Vermeulen at various values of input variables – sex steroid binding globulin (SHBG) and total testosterone [14].
Literature
1. Emadi-Konjin, P., J. Bain, and IL Bromberg, Evaluation of an algorithm for calculation of serum “bioavailable” testosterone (BAT). Clin Biochem, 2003. 36 (8): p. 591-6.
2. Carruthers, M., Testosterone deficiency syndrome: cellular and molecular mechanism of action. Curr Aging Sci, 2013. 6 (1): p. 115-24.
3. Winters, S. J., D. E. Kelley, and B. Goodpaster, The analog free testosterone assay: are the results in men clinically useful? Clin Chem, 1998. 44 (10): p. 2178-82.
4. Dunn, J. F., B. C. Nisula, and D. Rodbard, Transport of steroid hormones: binding of 21 endogenous steroids to both testosterone-binding globulin and corticosteroid-binding globulin in human plasma. J Clin Endocrinol Metab 1981. 53 (1): p. 58-68.
5. Sodergard, R., et al., Calculation of free and bound fractions of testosterone and estradiol-17 beta to human plasma proteins at body temperature. J Steroid Biochem, 1982. 16 (6): p. 801-10.
6. Vermeulen, A., L. Verdonck, and J. M. Kaufman, A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 1999. 84 (10): p. 3666-72.
7. Mazer, N.A., A novel spreadsheet method for calculating the free serum concentrations of testosterone, dihydrotestosterone, estradiol, estrone and cortisol: with illustrative examples from male and female populations. Steroids, 2009. 74 (6): p. 512-519.
8. Antonio, L., et al., Low Free Testosterone Is Associated with Hypogonadal Signs and Symptoms in Men with Normal Total Testosterone. J Clin Endocrinol Metab, 2021. 101 (7): p. 2647-57.
9. Herold, D. A. and R. L. Fitzgerald, Immunoassays for testosterone in women: better than a guess? Clin Chem, 2003. 49 (8): p. 1250-1.
10. Taylor, A. E., B. Keevil, and I. T. Huhtaniemi, Mass spectrometry and immunoassay: how to measure steroid hormones today and tomorrow. Eur J Endocrinol, 2015. 173 (2): p. D1-12.
11. Nizhnik, A.N., Belov D.A., Simenel E.S. , Experience in diagnosing steroidogenesis disorders using tandem gas chromatography-mass spectrometry among patients of the ArchiMed Clinic [unpublished data]
12. Goncharov, N., et al., Diagnostic significance of free salivary testosterone measurement using a direct luminescence immunoassay in healthy men and in patients with disorders of androgenic status. Aging Male, 2006. 9 (2): p. 111-22.
13. Keevil, B. G., et al., Salivary testosterone measurement by liquid chromatography tandem mass spectrometry in adult males and females. Ann Clin Biochem, 2014. 51 (Pt 3): p. 368-78.
14. Belov, D.A., Male testosterone calculator for Windows OS (developed at the ArchiMed Clinic). 2021.
What causes increased testosterone?
• Adrenogenital syndrome provokes high testosterone in women;
• New growth of the testes increases testosterone in men;
• Disease or Itsenko-Cushing syndrome;
• A neoplasm in a woman’s ovaries, leading to the development of “masculinity” (deepening of the voice, a figure similar to a man’s, etc.);
• Decreased sex steroid binding globulin, or SHBG, in the blood;
• Excess and high intensity physical activity;
• The use of certain medications, such as levonorgestrel, mifepristone and various oral contraceptives, as well as tamoxifen, finasterine, danazol, phenytoin, etc.
Complexes with this research
Expanded anti-aging diagnostics in postmenopause Expanded control of age-related changes during postmenopause 29,230 R Composition
Adrenogenital complex Analysis of excess male hormones in women 2,560 R Composition
Male hormones Assessment of hormonal levels in a man at any age RUR 6,180 Composition
IN OTHER COMPLEXES
- Male infertility. Extended examination RUB 29,030
- Female hormones. Follicular phase 5,930 R
- Men's check-up No. 1 RUB 18,570
- Advanced male anti-aging diagnostics RUB 33,710
- Anti-aging diagnostics in postmenopause RUB 12,630
Testosterone hormone in women - where does the danger lie?
Femininity does not mean that women should have no testosterone at all.
Everyone knows that excess testosterone in women causes masculinity, infertility, excess hair growth, as well as increased excitability and aggression. But low testosterone in women and men leads to decreased libido, physical weakness, hair loss, excess body weight, osteoporosis, atrophic changes in the skin, decreased mood, and even depression. Therefore, both high and low testosterone pose a danger to women’s health.
Having learned from your doctor about testosterone, how to increase its level, you can use simple methods that are available to everyone and approved by modern medicine.
Thyroid-stimulating hormone
It has a stimulating effect on all stages of the biosynthesis of thyroid hormones, which increase the utilization of carbohydrates, increase the absorption of glucose by muscles, stimulate protein synthesis, increase the breakdown of fats and the oxidation of fatty acids.
Helps maintain normal weight and stay slim. Thyroid dysfunction leads to the development of symptoms that cause metabolic disorders, as well as reproductive function. 31-20-001 — TSH (thyroid-stimulating hormone)
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
Reference values
| Patient age | Women, pg/ml | Men, pg/ml |
| 6 – 12 years | < 1,46 | < 4,6 |
| 12 – 19 years old | < 2,24 | 0,18 – 23,08 |
| 19 – 55 years old | < 2,85 | 1,0 – 28,28 |
| Over 55 years old | < 1,56 | 0,7 – 21,45 |
Factors influencing the result
- Presence of chronic diseases;
- Dysfunction of the endocrine system;
- Violation of the rules for preparing for analysis;
- Violation of the venipuncture algorithm, as well as the requirements for transportation and storage of biomaterial;
- Taking medications: nilutamide;
- rifampin;
- danazol;
- magnesium sulfate;
- ketoconazole;
- dexamethasone;
- methylprednisolone;
- prednisole;
- thioridazine;
- tetracycline, etc.
Decreased testosterone
- Hypogonadism;
- Violation of the production of gonadotropic hormones by the pituitary gland;
- Hyperprolactinemia (increased serum prolactin hormone);
- Impaired potency, chronic prostatitis in men;
- Obesity of all types (in men);
- Adrenal insufficiency.
On a note:
a decrease in testosterone production can occur due to changes in diet (low-carbohydrate or low-lipid diets, fasting, vegetarianism, fasting, etc.). Also, the concentration of the hormone decreases in case of prolonged alcohol intake.
Indications for analysis
The appointment, interpretation of the analysis and diagnosis are carried out by the following specialists: endocrinologist, gynecologist, urologist, andrologist, reproductive specialist, therapist, pediatrician, family doctor.
For representatives of both sexes, a testosterone test is prescribed in the following cases:
- infertility;
- pathological baldness (alopecia);
- acne in adulthood;
- oily seborrhea, dandruff;
- aplastic anemia (impaired production of blood cells by the bone marrow);
- adrenal neoplasms;
- control of the intake of certain medications: glucocorticoids, steroids, androgens, etc.
Additionally for men:
- Impaired potency and erectile dysfunction;
- decreased sex drive;
- pathological age-related changes;
- hypogonadism (testicular dysfunction) primary and secondary;
- osteoporosis (a chronic skeletal disease associated with increased fragility and fragility of bones).
Additionally for women:
- menstrual irregularities: anovulation (lack of ovulation);
- amenorrhea (absence of menstruation of primary or secondary nature);
- oligomenorrhea (extension of the menstrual cycle to 35 days or more);
Introduction
Good news, the World Health Organization considers the age group 45-59 to be “average”, but right behind it is “older” 60-74. That is why many doctors believe that up to 45 (a young age), in most cases, to maintain health, you can do without any serious therapy, including hormonal therapy. However, after 45 years, the functions of organs and systems may decline, which requires monitoring and, if necessary, treatment.
Hormones are substances produced by internal glands that regulate all metabolic processes in the human body. The change in their activity with age is considered by many scientists as a central link in the aging process (the theory of V.N. Dilman, 1983). The word "hormone", from the Greek "hormao", means "to quickly bring into action", "to raise" or "to excite". It was invented by the British physiologist Ernst Starling in 1905.
In her book The Brain of the Sexes, Anna Moire writes: “What really sets men and women apart, testosterone, literally shapes our brains and our creativity, intelligence, way of thinking, energy, desire to understand different things. It influences and controls not only the potential we possess, but also the benefit we derive from it. It controls our sexual and communicative behavior."
The steroid hormone testosterone in men is produced in the testicles. It is he who makes men out of men. It has a biological effect on almost all organs and tissues.
At 10-12 years of age (puberty), increased production of testosterone begins, which leads to:
- rapid growth of muscles and bones (anabolic effect)
- hair growth on the pubis, in the armpit
- deepening of the voice
- increased activity of the sebaceous glands (juvenile acne)
- change in character (adolescence)
- the emergence of interest in the opposite sex (appearance of libido)
Historically, the absence of all these changes could be seen in teenage singers in Italy, who were castrated in order to maintain a high timbre of the voice.
Testosterone levels peak at the age of 20, when we are active, energetic, cheerful, and in good physical shape (no obesity).
Starting at age 30, testosterone levels decline by about 1-2% per year. The prevalence of hypogonadism (low testosterone) in men is 6%, and in obesity and diabetes - more than 50%.
Unlike female menopause (“step” in French), the age-related decrease in testosterone occurs gradually, and therefore is not so acutely felt by men. As a rule, the first symptoms appear at the age of 50, their number increases like a “snowball”. Unsuspecting men begin to literally “fall apart before our eyes,” go to different doctors (cardiologist, endocrinologist, neurologist, urologist), and take handfuls of various medications for a large number of diseases. The trouble is that all of them do not treat the cause, but only act on the symptoms of the disease. And only competent doctors can assume the presence of age-related androgen deficiency and recommend donating blood from a vein to determine the level of total testosterone.