Synonyms: determination of IgG antibodies to the rubella virus, Anti-Rubella-IgG, Rubella antibodies IgG, german measles specific IgG.
Related tests: determination of IgM antibodies to the rubella virus, determination of the avidity index of specific IgG, detection of rubella virus RNA.
IgG antibodies to the rubella virus indicate the presence of immunity to the rubella virus or a history of the disease. The rubella virus is most dangerous for pregnant women, as it causes defects in the development of the fetus, including its death.
Antibodies to rubella virus IgG, Rubella IgG quantity.
Antibodies to rubella virus IgG, Rubella IgG quantitative
— allows you to determine the presence of immunity to the Rubella virus. IgG antibodies begin to be produced 3–4 weeks after infection, reach their peak by a month from the onset of the disease and remain in the blood for life, which provides a person with immunity from re-infection.
Rubella virus causes rubella
is an acute viral infectious disease that affects mainly children, and in rare cases adults. Rubella (Rubella) is part of a group of reproductively significant infections referred to as the TORCH complex (Toxoplasma, Rubella, Cytomegalovirus, Herpes).
An anti-Rubella-IgG level of more than 10 U/ml is recommended as an indicator of the presence of immunity to this virus. Determination of anti-Rubella-IgG titers over time (in paired studies with an interval of 2-3 weeks) is used, if necessary, to confirm a recent infection with the rubella virus (in addition to the determination of anti-Rubella-IgM). A significant increase in IgG titers indicates the severity of the process. Positive anti-Rubella IgG results when testing umbilical cord blood or newborn blood should be interpreted with caution, since specific IgG can be transmitted to the fetus from the mother through the placenta.
Rubella
- an acute viral infectious disease that can occur in typical, erased and asymptomatic forms. The rubella virus is unstable in the external environment, so infection requires fairly long and close contact with the patient. Transmission of infection occurs by airborne droplets and transplacentally (from mother to fetus). Mostly children 1–7 years old are affected. When a pregnant woman becomes infected, severe malformations or spontaneous abortion occur. When transmitted by airborne droplets, the virus infects the epithelial tissue of the upper respiratory tract, enters the bloodstream, then into the lymph nodes, where it replicates. The incubation period lasts 15–21 days.
Rubella in childhood
In children, the disease is relatively mild. It begins with enlargement of the lymph nodes in the neck and back of the head; after 1–5 days, a finely spotted rash up to 5 mm in size appears on the face (not rising above the surface of the skin). During the day, the rash spreads from top to bottom to the extensor surfaces of the limbs, back, and buttocks. A slight fever and catarrh of the upper respiratory tract are present. After 1–3 days, the elements of the rash disappear without a trace.
Rubella in adults
In adults, rubella is more severe and complications develop more often. The most common is polyarthritis, lasting 1–2 weeks. Encephalitis occurs less frequently (1:5000), but the mortality rate in this case is 20–40%. Encephalitis may precede the rash by 1–12 days, but more often develops on the 3rd–4th day of the onset of the rash.
During transplacental transmission, the virus affects the endothelium of the capillaries of the placenta, causing fetal hypoxia, then – embryonic tissues, where it suppresses the mitotic activity of individual cell populations. If primary rubella infection occurs during the first 12 weeks of pregnancy, the virus crosses the placenta and causes generalized and persistent infection of the fetus, which almost always causes multisystem disease and congenital malformations. When infected later in pregnancy (13–16 weeks and later), the incidence of defects in intrauterinely infected infants decreases, but a certain danger remains until the third trimester.
Duration of infection. Developmental defects:
- Weeks 3–11: central nervous system;
- 4–7 weeks: organ of vision, heart;
- Weeks 7–12: hearing organ.
Laboratory diagnosis of rubella is of particular importance in the following categories of subjects:
- women preparing for pregnancy
1. Latent course in childhood (no diagnosis - there is immunity). 2. Errors in the differential diagnosis of rubella (there is a diagnosis - there is no immunity). 3. Resolving the issue of vaccination.
- Pregnant women
1. Congenital rubella. 2. Developmental defects. 3. Fetal hypotrophy.
- Adults
1. Severe course, complications.
Rubella and TORCH
Rubella is part of the group of TORCH infections (the name is formed by the initial letters in the Latin names - Toxoplasma, Rubella, Cytomegalovirus, Herpes), which are considered potentially dangerous for the development of a child. Ideally, a woman should consult a doctor and undergo laboratory testing for TORCH infection 2–3 months before the planned pregnancy, since in this case it will be possible to take appropriate therapeutic or preventive measures, and also, if necessary, compare the results of studies before pregnancy in the future with the results of examinations during pregnancy.
Indications:
- preparation for pregnancy (women);
- lymphadenopathy and/or small-spotted rash during pregnancy if immunity to rubella was previously absent or not tested;
- enlargement of the occipital, posterior cervical, and/or parotid lymph nodes;
- finely spotted rash combined with lymphadenopathy (in adults);
- resolving the issue of vaccination (women).
Preparation
It is recommended to donate blood in the morning, between 8 am and 12 pm. Blood is drawn on an empty stomach, after 4–6 hours of fasting. It is allowed to drink water without gas and sugar. On the eve of the examination, food overload should be avoided.
Interpretation of results
Units of measurement: U/ml.
Reference values: 0–5 U/ml
- 5.0 - negative;
- 5.0–9.9 – doubtful (it may be advisable to repeat the study in 10–14 days);
- >=10.0 - positive.
Increasing reference values:
- presence of immunity to the rubella virus;
- current infection.
Within reference values:
- lack of stable immunity, evidence of susceptibility to the rubella virus;
- The seronegative period of current infection is the first two weeks after infection.
Rubella virus, IgG (quantitative)
Rubella virus causes rubella, an acute viral infectious disease that mainly affects children and, in rare cases, adults. It poses the greatest danger to pregnant women, as it can lead to severe congenital malformations of the child, and even intrauterine fetal death is possible. Therefore, determining antibodies to the rubella virus is very important when planning pregnancy. It may indicate the presence of immunity to this virus or a past illness.
Synonyms Russian
IgG antibodies to the rubella virus.
English synonyms
Rubella antibodies, IgG, german meats specific IgG, antirubella-IgG.
Research method
Solid-phase chemiluminescent enzyme-linked immunosorbent assay (“sandwich” method).
Units
IU/ml (international unit per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
Do not smoke for 30 minutes before the test.
General information about the study
This test detects antibodies to rubella in the blood. They are produced in response to infection by a virus. There are two types of antibodies: IgM and IgG. The production of IgG antibodies takes a little longer than IgM antibodies, but once it occurs, the antibodies remain in the blood for life, protecting a person from re-infection. The presence of IgG antibodies may indicate that you have already had rubella or that the rubella vaccine provides adequate protection.
Rubella is spread through the air and usually appears mild as a small red rash that appears on the face and neck and then spreads to the torso and limbs before disappearing after a few days, although symptoms such as fever, lymph nodes, runny nose, red eyes and joint pain.
However, in most patients, rubella goes away within a few days without any special treatment and does not cause further health problems. The main danger is that a pregnant woman comes into contact with the rubella virus for the first time during the first trimester of pregnancy - the developing fetus is most vulnerable to rubella at this time. If the virus is passed from mother to fetus, it can cause miscarriage, stillbirth, and/or congenital rubella syndrome (CRS), a group of serious birth defects that can cause developmental delays, mental retardation, deafness, cataracts, microcephaly, and liver problems. and heart defects.
What is the research used for?
- To test immunity to the rubella virus.
- To detect infections, including those suffered in the past.
- To identify those who have never been exposed to the virus and those who have not been vaccinated.
- To ensure that pregnant women (or those who are just planning a pregnancy) have sufficient anti-rubella antibodies to protect against infection.
When is the study scheduled?
- When planning or managing pregnancy.
- If rubella immunity testing is necessary.
- When a pregnant woman develops fever and rash and/or other symptoms of rubella. Since many diseases cause similar symptoms, the doctor should order tests that will help confirm this particular diagnosis.
- If the infant has congenital malformations (hearing loss, cardiovascular disorders, cataracts, diseases of the central nervous system) that may be associated with CRS, or if the mother was diagnosed with rubella during pregnancy.
Because it takes some time for rubella IgG antibodies to develop after infection, your doctor may order tests again after 2 to 3 weeks to see if antibodies show up (if they weren't present initially) or to assess whether their levels are rising or falling over time.
What do the results mean?
Reference values
Concentration: 0 - 10 IU/ml.
Result: negative.
Negative result
- Lack of stable immunity to the rubella virus.
- Recent infection (no immune response has been developed).
Positive result
- Current or past rubella.
- Having immunity to the rubella virus.
Presence of IgG antibodies in the absence of IgM antibodies
- Exposure to the virus or vaccination, as well as immunity to the rubella virus.
Presence of IgG antibodies in the absence of IgM antibodies in the newborn
- The IgG antibodies were passed on to him in the womb and may protect him from rubella during the first six months of life.
Presence of IgG antibodies together with IgM antibodies
- Recent infection with rubella virus.
Important Notes
- The examination for rubella must be comprehensive, i.e., include, in addition to the test for Rubella virus, IgG, and other tests.
- This study is recommended primarily when planning pregnancy.
- In adults, rubella disease is often more severe than in children.
- In the absence of IgG and IgM antibodies in an unvaccinated person, vaccination is recommended.
Also recommended
- Rubella virus, IgM (quantitative)
Who orders the study?
Gynecologist, infectious disease specialist, therapist, pediatrician.
References
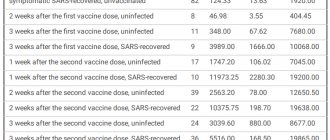
- Temporary guidelines. Prevention, diagnosis and treatment of new coronavirus infection (COVID-19). Version 10. 02/08/2021.
- Lize M. Grobbelaar et al. SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: Implications for microclot formation in COVID-19/ medRxiv, 2021.
- Elizabeth M. Rhea et al. The S1 protein of SARS-CoV-2 crosses the blood-brain barrier in mice/ Nature Neuroscience, 2021, Vol. 24, pp. 368–378.
- Andrey V. Letarov et al. Free SARSCoV2 Spike Protein S1 Particles May Play a Role in the Pathogenesis of COVID19 Infection/ Biochemistry (Moscow), 2021, Vol. 86, No. 3, pp. 257–261.
- https://www.rospotrebnadzor.ru/about/info/news/news_details.php?ELEMENT_ID=15649
- https://sputnikvaccine.com/rus/
- Materials from the test system manufacturer.
Detailed description of the study
SARS-CoV-2 is a beta coronavirus of the Coronaviridae family. A virion, or viral particle, is genetic material - ribonucleic acid (RNA) - associated with a special nucleocapsid protein (N-protein), packaged in a spherical protein shell.
On the outer surface of the virion shell there are “spikes” formed by the S-protein (from the English Spike - spike). Thanks to the “spikes,” the virion penetrates the cell. The S protein consists of two functional subunits: S1 (containing the RBD domain) ensures binding to the target cell receptor, S2 promotes the fusion of the virus and the cell membrane. Also, the S-protein, which is capable of independently circulating in the blood and even penetrating the blood-brain barrier, is associated with disturbances in the hemostasis system and other pathological conditions in patients and survivors of COVID-19.
As a rule, the infectious process begins after the virus penetrates the epithelial cells lining the mucous membranes of the upper respiratory tract. In infected cells, active replication of the virus begins - a multiple increase in the number of copies of viral particles, or virions. New virions emerge from the affected cells and infect an increasing number of healthy cells, not only of the upper, but also of the lower respiratory tract. Including possible damage to type II alveolar cells, which determines the development of pneumonia.
SARS-CoV-2 virions are able to penetrate cells on the surface of which there is a membrane protein called angiotensin-converting enzyme type II (ACE2), which serves as a receptor for the viral particle. ACE2 is present on the cell membranes of the organs of the respiratory and central nervous systems, esophagus, ileum, kidneys, bladder, and heart. The new coronavirus can infect nerve cells, including brain cells, which has been linked to odor perception disorder in some patients.
SARS-CoV-2 infection can be asymptomatic (up to 50% of cases), in mild and severe forms. In the latter case, the development of acute respiratory syndrome (Severe Acute Respiratory Syndrome, SARS) is possible against the background of bilateral pneumonia. The incubation period lasts 2–14 days, more often 5–7 days. After which the patient develops symptoms of acute respiratory viral infection (ARVI).
All people infected with coronavirus, even those whose infection occurs in an erased or asymptomatic form, are a source of infection already in the first days after infection. Since they release viral particles into the environment with exhaled air, when talking, coughing, sneezing. On average, viral shedding lasts about 20 days, but in some cases it can last longer than a month.
Due to the fact that the new coronavirus infection has not yet been sufficiently studied, as well as the short period of use of vaccines, the period of circulation of neutralizing antibodies in the blood is not yet reliably known.
The test will allow your doctor to:
- Diagnose rubella disease;
- Confirm the presence of immunity to the rubella virus when planning and during pregnancy;
- Detect the presence of TORCH infections.
The study is recommended for:
- Planning pregnancy;
- Screening pregnant women for TORCH infections;
- Pregnancy, if symptoms of rubella appear;
- A small red rash on the face and neck that spreads to the trunk and limbs;
- Enlarged lymph nodes;
- Increased temperature;
- Runny nose;
- Joint pain;
- Newborns with congenital malformations (visual damage, heart defects, damage to the bones of the limbs and skull, developmental delay, etc.).
Method:
Enzyme-linked immunosorbent assay (ELISA).
Sensitivity:
Not less than 2 IU/ml.
Material for research:
Blood serum.