Pregnancy is a rather complex process, the course of which determines the life of the child, the mother, and their health. One of the most important components of the proper course of pregnancy is the Rh factor.
In order to understand which Rh factor the expectant mother has, a special test for alloimmune antibodies is carried out. It allows you to determine whether there is a special protein in the blood located on the surface of red blood cells. If it is not there, then the person has negative Rh blood (it occurs in 15% of the world's inhabitants). In everyday life it doesn’t bother us at all, but when carrying a child, everything changes, as it can cause many problems. For example, it can cause Rhesus conflict. Rhesus conflict is the interaction of negative and positive blood particles (erythrocytes), as a result of which they stick together (agglutination) and disturbances appear.
What are these antibodies?
As expected after vaccination, I checked IgG - a type of antibody that is responsible for immunological memory and remains in the blood after the active phase of the war with the virus is over. And these are, of course, antibodies to the coronavirus S protein. After an illness, they sometimes check for antibodies to the N-protein, but I shouldn’t have them, since I didn’t encounter the whole viral particle, but only a specific surface protein.
My test form says “neutralizing antibodies to the RBD domain of the S protein.” That is, in my blood they were looking not for any antibodies that could stick to the coronavirus particle (they are called binders), but only for those that would settle on the “master key” with which the virus should contact the cell and prevent it from penetrating inside (but these are already neutralizing). Strictly speaking, in an ordinary commercial laboratory no one checks whether, under the influence of my antibodies, the virus will not be able to infect cells - this is quite time-consuming and expensive, you will need to grow a cell culture and keep a supply of coronavirus (or its analogue, pseudovirus) on hand.
Therefore, a simpler test system is used: a known amount of ACE2 receptors is placed on a plate (a “lock” for the virus), and blood plasma and a known amount of the luminous RBD domain of the S protein (“master key”) are poured into the solution. After some time, you can pour out the liquid and see how many luminous master keys still got into the keyholes - and convert this into the concentration of antibodies. This parameter correlates with the results of tests on cells, and is thought to be useful as a measure of neutralization - although it is likely that not all antibodies that show up in such a surrogate test will be sufficiently sticky and persistent in real cellular life.
Dynamic control and diagnostics
To predict how the pregnancy will develop, it is important that the woman comes for a consultation as early as possible (this is especially true if this is the second or third pregnancy), and she has previously been diagnosed with antibody sensitization or hemolytic disease of the newborn/fetus.
To control the progress of pregnancy it is important:
- during registration, all pregnant women must undergo laboratory tests such as determining their blood group and Rh factor;
- if a woman is found to be Rh negative, the father is also recommended to undergo the test;
- if the fears are confirmed and the parents have different Rh factors, then the pregnant woman is tested for the presence of antibody titres every 8 days until the 20th week;
- determine the type of immunoglobulins (IgG or IgM);
- after 20 weeks, the pregnant woman is sent for observation to a specialized center;
- from 32 weeks, antibody titer tests are done once every 14 days, and from 35 weeks - once every 7 days;
- The situation can be predicted by the gestational age in which antibodies were detected. It will be the more unfavorable, the earlier immunoglobulins to the Rh factor were discovered.
If antibodies are detected during the second pregnancy, the occurrence of Rh conflict increases, so invasive or non-invasive treatment methods cannot be avoided.
How are they measured?
“AU” is an arbitrary unit, a standard unit in which the concentration of antibodies is measured. They do not directly correspond to either milligrams per milliliter (in which concentration is usually measured) or titer (that is, the limiting dilution at which antibodies do not lose their activity - this metric is often used by immunologists). These units are a proprietary scale that only works within a specific test system, in my case Abbott Architect. And each developer has his own scale.
In order to somehow unify the results, WHO introduced an international standard. Back in June 2021, doctors took blood samples from 11 people who had recovered from Covid and collected from them a plasma standard with antibodies - something in the spirit of the metrology of the past, when the kilogram and meter were “fixed” in real terms. This jar of plasma was designated as a reference point and assigned a concentration of 1000 IU (international units) and 1000 BAU (binding antibody units) - so that both neutralizing and binding antibodies could be calibrated against it (although their benefits are different, their concentrations correlate together). Now every test system manufacturer can order such a sample and figure out how to convert its own scale into an international one (here is an example).
Abbott came up with a coefficient of 0.142 - that is, to convert my result to international units, you need to divide it by 7. It turns out that there are 87 IU of neutralizing antibodies in my blood.
Not everyone can do such a recalculation, because not all test manufacturers publish their coefficients of compliance with the international standard. For Roche tests this is approximately 1:1 (on the forms of Moscow laboratories the sensitivity limit is indicated at 250 IU, although in scientific articles the limit is 2500 IU), for Diasorin 2.6:1 (that is, you need to multiply your result by 2.6) . For the Chinese Mindray test system, which is used, for example, at the Sklifosovsky Institute, I could not find this coefficient. And on the test forms from state clinics that several friends sent me, the manufacturer is not indicated at all.
What to compare them to?
On the website of any clinical laboratory (here is an example) there is a section “interpretation” - and nowhere is the protective concentration of antibodies indicated. To establish it for sure, we need experiments with deliberate infection (we wrote about them in the material “Sick for Us”): that is, you need to take people with a known antibody titer, infect them with a known dose of the virus - and see who gets sick and who doesn’t. Such experiments began only recently, and nothing is yet known about their results.
Therefore, I can only try to place myself on a scale from those who definitely do not have antibodies to those who certainly have a lot of them.
The lower limit of this scale is shown right on the test form: Abbott considers a result up to 50 AU (that is, up to 7 IU) negative. Everything above is suggested to be considered a positive answer (“there are antibodies!”) - but, I remind myself, at the same time no one promises that there will be enough of them for protection.
Abbott's test sensitivity limit is 40,000 AU. It has, however, a chemical rather than a biological meaning - this limitation is imposed by the design of the system, and not by the maximum power of human immunity. Therefore, it will be more useful to compare yourself with those who have already been sick or vaccinated.
Here, for example, is data from a sample of five hundred Poles. On this scale, with my 87 IU, I look like a person who was not vaccinated, but still had Covid, albeit without symptoms.
Andrzej Tretyn et al. /ResearchSquare
Share
But studies on several dozen Americans and a couple of hundred Germans show that, a month and a half after vaccination, they have an average of two to three thousand IU or BAU, and the elderly have an average of several hundred. There is also a comparison of the titers of healthy vaccinated people with those who were vaccinated against the background of immunosuppressive therapy: a week after vaccination, the first had 2.5 thousand BAU, and the second had only 2 thousand. Even compared to people with suppressed immune systems, my 87 IU looks pale.
Before I can get too upset, I remind myself that this comparison has many limitations.
First, the researchers caution people against comparing results obtained in different test systems. Since each developer selects the test S-protein himself, the systems can “catch” slightly different antibodies - and, as a result, produce different concentrations. Therefore, monitoring the numerical dynamics of your own antibodies may still make sense, scientists say, but comparing yourself with others is a useless and thankless task.
Secondly, all the data against which I consider my 87 IU were obtained in other countries, in a different epidemiological situation, and most importantly, after the injection of other vaccines. A similar sample for Sputnik has not been published - and who knows what range of concentrations would be measured in it?
Do they protect well?
How the number of antibodies relates to the mythical “level of protection” is an even less clear question. No one knows how many antibodies are needed to be 100 percent sure of not getting sick from Covid. Strictly speaking, such a ceiling may not exist - one can easily imagine a situation in which there are enough antibodies in the blood, but they do not have time to reach several viral particles, and then infected cells - and the virus begins to multiply in the body. At least, doctors met individual patients whom a high concentration of antibodies did not save from infection.
But should there be some rough estimates? I open a recent article in Nature Medicine
: its authors collected data from clinical trials of different vaccines and looked at how the concentration of antibodies shortly after vaccination correlates with “vaccine effectiveness” (that is, the ratio of sick people in groups of vaccinated and unvaccinated: more about how it is calculated in our text “The Magic of Numbers” "). They discovered some kind of relationship, but it turned out to be nonlinear.
Here's what they came up with:
- Vaccines that cause a person to produce the same amount of antibodies as if they had the disease have been shown to be about 80 percent effective.
- Vaccines that left people with more antibodies than those who had recovered from the disease were more effective—but not much.
- Vaccines, after which those vaccinated produced fewer antibodies than those who had been ill, turned out to be much less effective in clinical trials.
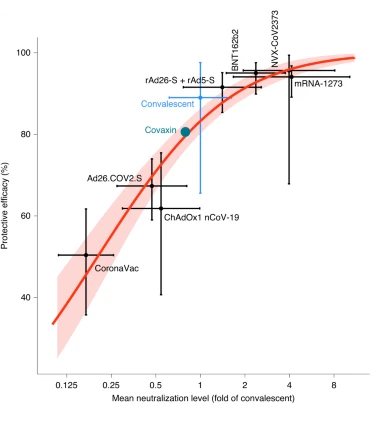
Horizontally - the average titer of neutralizing antibodies in vaccinated people in relation to those who have recovered from the disease (they are taken as one). Vertical - vaccine effectiveness (based on the results of the third phase of trials). The green dot is the Covaxin vaccine, people vaccinated with it produced the same number of antibodies as those who had recovered from the disease, and the effectiveness was about 80 percent. The red curve is the estimated dependence of efficiency on titer.
David S. Khoury et al. / Nature Medicine, 2021
Share
Similar curves are found quite often in biology. This is almost any “dose-effect” relationship: as long as the dose is less than a certain threshold, even a significant increase does not affect the result; after it is “taken,” a sharp increase in efficiency begins, then saturation occurs. At the beginning and at the end, such a curve will be flat, which is why it is called S-shaped. In the case of vaccines, the beginning of the curve, when there is very little antibody, simply did not interest anyone - but if we extend this graph to the left, we will certainly see a flat “bottom” there, the lower half of the “S”.
S-curves do not allow for accurate predictions. It is very easy to miss the center of the graph - the effect grows too quickly. Therefore, usually, using such graphs, only the dose is calculated, which provides 50 percent of the effect (aka PD50, from protective dose), in our case, protection against covid. For the authors of the article, this cutoff was equal to 20 percent of the average antibody titer in people who had recovered from the disease. From their sample, they estimated that this was approximately 54 IU (confidence interval 30-96). If we measure it by the Poles, whom I focused on before, it turns out even less - about 25 BAU.
It follows that the efficiency of my 87 IU is most likely higher than 50 percent - which means that all is not lost. According to these calculations, they provide me with some kind of protection. It is impossible to calculate which one exactly.
However, I need to be careful with this optimistic conclusion. Authors of the article in Nature Medicine
They did, of course, very important work: they brought to a single denominator all the antibody titers that the developers measured in the first phases of testing their vaccines. But they obtained all these titers on very small samples (which is probably where the wide confidence interval comes from). For example, only 20 people participated in the first phase of Sputnik testing.
Does this mean that the vaccine did not have the best effect on me from the very beginning? Or is it really outdated? The authors of the same article also calculated the rate of “decay” of antibodies in the blood. They suggested that if this happens after vaccination at the same pace as after recovery, then the relationship will also be non-linear. The more antibodies there were at the beginning, the slower they will disappear from the bloodstream. In six months, according to their calculations, a vaccine with 99% effectiveness (alas, we don’t have one yet) will practically not lose its power, but 90% effectiveness should drop to 70%.
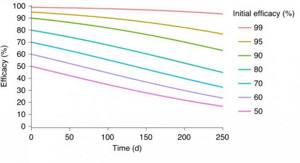
If the concentration of antibodies in vaccinated people fell as quickly as in the body of those who have recovered from the disease, then the effectiveness of vaccines would change according to this model: the higher it is at the start, the slower it decreases over time
David S. Khoury et al. / Nature Medicine, 2021
Share
This probably explains why medical agencies in many countries recommend that those who have recovered from the disease be vaccinated - their initial concentrations are lower and therefore run out faster. This probably explains my low result - apparently, it was low from the very beginning.
Will they save you from new variants?
As in the case of the “regular” coronavirus, with the delta variant it is completely unclear what antibody titer provides protection - and, as we remember, there is no certainty that this very titer is the issue. The developers of Sputnik promised that their vaccine would remain effective, but so far they have not clearly proven this. But it was calculated that the activity of antibodies in neutralizing the beta (“South African”) and delta variants is approximately two times lower than for their “British” predecessor (alpha variant). If the results of laboratory research could be directly transferred to a living organism, then we would have to conclude that it would no longer be 87, but 43.5 IU that would protect me from the “delta”.
Recently, French scientists also tried to determine the threshold concentration of antibodies for neutralizing coronavirus variants in vitro
. At that time, they had not yet dealt with “delta”, but they tested the serum of recovered people against the “alpha” (“British”) and “beta” variants. They found that to neutralize alpha by more than 50 percent, 200 according to Abbott is enough (that is, about 30 IU, if this coefficient is the same for all Abbott test systems) - approximately this is what they counted in people who recovered from Covid during the year (this is is very different from the results from other works, which once again shows how difficult it is to compare different samples and test systems with each other). And to cope with the “beta”, according to them, 1000 AU (142 IU) will be required.
This data would seem to indicate that my chances of holding out against delta are slim. But I’m not in a hurry to get upset here either: to come to this conclusion, I needed to make many assumptions. I had to assume, among other things, that the delta strain behaves the same as beta, that the neutralizing activity of antibodies falls linearly, that neutralization of the virus in vitro
(which evaluates the evasion of antibodies by variants) works the same way as inside the human body - and finally, that my immunity works the same as that of an average employee of a French hospital who has recovered from Covid. In reality, everything may turn out to be completely different.
Possible complications from Rhesus conflict

The most important issue for the mother is the consequences that can await the child after the occurrence of Rhesus conflict. Some of the most dangerous consequences are oxygen starvation of the brain, as well as the accumulation of fluid in all cavities and organs of the baby. As a result, the normal functioning of all systems is disrupted, and edema, which is very dangerous for the child, may appear. In this case, only intensive therapy can help the baby, since without treatment, it is unlikely that the child will be saved.
Also, pregnancy with Rhesus conflict causes the following complications:
- anemia;
- premature birth;
- bleeding;
- gestosis;
- miscarriage;
- complications after pregnancy.
It is worth noting that fetal death is possible only in the case of a complex Rhesus conflict; in other cases, the consequences may not be so tragic, but they should not be underestimated.
***
Giving up attempts to recalculate my antibody titer into something more meaningful, I once again remind myself (and you) that my immune system is not limited to antibodies alone. We still don't know exactly what contribution they make to protection against Covid. It is possible that someone manages to do without them altogether. There is also immunological memory - memory B and T cells, data on which is much more problematic (and more expensive) to access. Therefore, no matter how dissatisfied I am with the work of my B lymphocytes and the titers of my antibodies, only time will tell how protected I really am.
The FDA does not recommend that anyone interpret test results on their own—and now, after four agonizing days spent recalculating titers and concentrations, I understand why.
Symptoms of Rhesus conflict
In fact, it is quite difficult to immediately understand that there is a rhesus conflict. Some women may experience symptoms similar to gestosis (the baby’s body spends a lot of energy creating more and more new red blood cells).
You can find out if there is a Rhesus conflict with the help of special tests and ultrasound examination. They can show:

- condition of the fetal organs: have the kidneys, liver, heart, spleen increased in size;
- is there swelling of the placenta, which causes thickening of the umbilical cord and enlargement of the placenta;
- whether swelling of the fetus has occurred, or there is an accumulation of fluid in the chest or abdominal cavity;
- are there any changes in the child’s position (he takes the “Buddha” pose, when the legs move to the sides through the enlarged abdomen and chest);
- whether swelling of the soft tissues of the brain has occurred, which leads to a bifurcation of the contour of the head.
The manifestation of such symptoms can cause fetal death as early as 20-30 weeks of development. If a child is born, he is usually found to have anemia or jaundice. In more severe cases, serious damage to important organs may occur (body weight increases by 1.5 times, which is very dangerous for newborns and can cause death).