Symptoms of NMO
NMO of the kidneys, as a rule, is clinically asymptomatic until the formation of urolithiasis or pyelonephritis, but in some cases it can manifest itself with the following symptoms:
- discomfort when urinating
- frequent urination
- aching pain or discomfort localized primarily in the lumbar region or abdomen
- paroxysmal (“renal colic”) or constant pain radiating to. iliac or groin area, inner thigh, genitals
- pain over the pubis can develop due to salt deposits or the presence of stones in the bladder
Diagnosis of NMO
The necessary comprehensive examination includes laboratory and instrumental methods.
Laboratory diagnostics
- A general urine test, which reveals crystals of salts of a particular acid. However, this study does not allow us to state with complete confidence about the presence of dysmetabolic nephropathy. The detection of salt crystals only in general urine tests is not a basis for diagnosing dysmetabolic nephropathy. It should be borne in mind that the excretion of crystals in the urine is often transient and does not appear to be associated with metabolic disorders. Therefore, to clarify the diagnosis, they resort to the second stage of the study - conducting a biochemical study of urine.
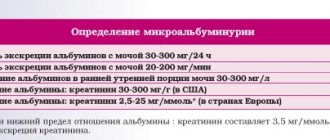
- Biochemical urine analysis allows you to evaluate the concentrations of certain salts in a portion of urine. The method is more accurate and sensitive for determining the quantitative level of oxalates, phosphates, urates and other salt crystals.
- ACOSM - determination of the anti-crystal-forming ability of urine. The method is quite complex and is not carried out in every medical institution.
- A series of tests for urinary peroxides and calciphylaxis. This technique makes it possible to identify calcium metabolism disorders and assess the degree of activity of peroxidation of the membranes of renal tissue cells, which is an important link in the development of dysmetabolic nephropathies.
Instrumental diagnostics
Ultrasound of the abdominal organs. Changes detected by ultrasound of the kidneys are usually not very specific. It is possible to detect microliths or “sand” (inclusions) in the kidney. Ultrasound of the kidneys, as a rule, is a nonspecific diagnostic method, but in some cases it allows you to track the formation of small stones and, thus, record the time of onset of urolithiasis.
Why is calcium so important?
Calcium in children's bodies is responsible for proper and harmonious development. If the mineral is present in the proper amount, then bones and teeth will also be in the correct condition, because calcium is the basic building material for these elements of the body. Among other things, calcium helps in maintaining the correct acid-base balance, metabolism, transmission of nerve impulses and is involved in normalizing the process of cell division.
The body's daily need for calcium is 1000 mg per day for a child from one to three years old. If there is not enough calcium, then a deficiency develops, which can cause the development of rickets and defects in the skeleton.
Treatment
Nutritional recommendations are the basis of therapy in both childhood and adulthood.
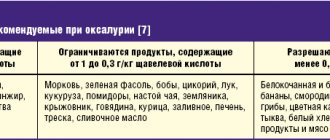
| Type of nephropathy | Prohibited Products |
| Oxalate nephropathy | Meat dishes, sorrel, spinach, cranberries, beets, carrots, cocoa, chocolate |
| Urate nephropathy | Liver, kidneys, meat broths, peas, beans, nuts, cocoa, alcoholic beverages |
| Phosphate nephropathy | Cheese, liver, caviar, chicken, legumes, chocolate |
| Cystine nephropathy | Cottage cheese, fish, eggs, meat |
Treatment of oxalate nephropathy
Diet
- when treating patients with oxalate nephropathy, a potato-cabbage diet is prescribed, which reduces the intake of oxalates from food and the load on the kidneys
- it is necessary to exclude jellied meat, strong meat broths, sorrel, spinach, cranberries, beets, carrots, cocoa, chocolate
- It is recommended to include dried apricots, prunes, pears in the diet
- from mineral waters such as Slavyanovskaya and Smirnovskaya are used, 3–5 ml/kg/day. in 3 doses, 1 month course 2-3 times a year
Drug therapy includes membranotropic drugs and antioxidants. Treatment should be long-term. Vitamins of group B, A, E are used. Special medications are prescribed for crystalluria. In addition, magnesium oxide is prescribed, especially with high oxalate levels.
Treatment of urate nephropathy
Diet
- in the treatment of urate nephropathy, the diet includes the exclusion of foods rich in purine bases (liver, kidneys, meat broths, peas, beans, nuts, cocoa, etc.)
- preference should be given to products of dairy and plant origin
- An important condition for successful therapy is sufficient fluid intake - from 1 to 2 liters per day. Preference should be given to slightly alkaline and low-mineralized waters, herbal decoctions (horsetail, dill, birch leaf, lingonberry leaf, clover, knotweed, etc.), oat decoction
Citrate mixtures can be used to maintain optimal urine acidity. In case of urate nephropathy, it is important to reduce the concentration of uric acid. For this purpose, agents that reduce the synthesis of uric acid are used.
Treatment of phosphate nephropathy
A diet is prescribed with a restriction of foods rich in phosphorus (cheese, liver, caviar, chicken, legumes, chocolate, etc.).
Treatment for phosphate nephropathy should be aimed at acidifying urine (mineral waters - Narzan, Arzni, Dzau-Suar, etc.; drugs - cystenal, ascorbic acid, methionine).
For any degree of severity of the disease, you must immediately consult a nephrologist or urologist for help, since long-term, generally reversible, metabolic disorders, if left untreated, can lead to the development of urolithiasis, followed by surgical intervention and chronic renal failure. Self-medication is not acceptable!
All types of drug therapy should be prescribed and monitored by a nephrologist or urologist, since:
- these medications have serious side effects on other organs and systems
- Some patients are initially unresponsive or gradually develop drug resistance
At the first stage of treatment, a treatment plan is drawn up. Treatment of any dysmetabolic nephropathy can be reduced to four basic principles:
- normalization of lifestyle
- correct drinking regime
- diet
- specific therapies
Taking large amounts of fluid is a universal way to treat any dysmetabolic nephropathy, as it helps reduce the concentration of soluble substances in the urine.
One of the goals of treatment is to increase the volume of urination at night, which is achieved by drinking fluids before bed. Preference should be given to plain or mineral water.
The diet can significantly reduce the salt load on the kidneys.
Specific therapy should be aimed at preventing specific crystal formation, removing salts, and normalizing metabolic processes.
At the second stage of therapy, the effectiveness of the diet is assessed, and control ultrasound examinations and analyzes are carried out.
The third stage of treatment is carried out after achieving stable remission. It represents a scheme of gradual reduction of doses of prescribed drugs to maintenance or their complete withdrawal while maintaining dietary recommendations.
Even after achieving the long-awaited remission, the patient is advised to be attentive to himself and regularly see a nephrologist or urologist, since the risk of relapse of diseases is high.
Almost all patients need to take anti-relapse therapy recommended by a doctor or adhere to a previously developed diet to prevent the formation or progression of urolithiasis and kidney inflammation.
Diet for phosphate nephropathy in a child
It is characterized by pathological excretion of phosphates in the urine. All types of disease are divided into true and false phosphaturia (excretion of phosphates in the urine). False phosphaturia (the presence of phosphates in the urine) occurs against the background of an excess of phosphorus-containing foods in the diet - cheese, caviar, beef liver, oatmeal, pearl barley, cottage cheese, chocolate, peas, eggs and river, as well as against the background of diseases of the parathyroid glands, edema, rickets, poisoning
True phosphate nephropathy can be hereditary or acquired. The first type is acquired from parents, most often on the maternal side. This is a rather severe metabolic disease, and was previously called phosphate diabetes, because in addition to salts in the urine, patients experience thirst and polyuria (excretion of very large volumes of urine), which is very similar to the first signs of diabetes. Disorders arise due to severe damage to the kidney tissue, which cannot filter urine normally, and in addition to phosphorus salts, many other substances, especially calcium, are lost into the urine, which also disrupts the structure of the skeleton. The clinical picture may resemble severe rickets, but changes in the urine help the doctor make the correct diagnosis. Fortunately, this condition is very rare.
In most cases, phosphates in the urine are found in children with an infection in the urinary tract caused by special organisms that can decompose urea - staphylococcus, Proteus, Pseudomonas aeruginosa, Klebsiella. Therefore, the presence of these salts in the baby’s urine should prompt the doctor and parents to conduct a more in-depth examination of the baby’s urinary system, even if there are no signs of infection. These microorganisms decompose urea into carbonic acid and ammonium in the urinary tract. Due to this, urine becomes alkalized and phosphates precipitate. Therefore, the appearance of tripelphosphates, amorphous phosphates in the urine and the alkaline reaction of urine are indicators of a urinary tract infection.
Treatment is similar to previous nephropathies. Diet plays an important role. Moreover, dietary therapeutic measures are aimed not only at limiting foods rich in phosphates, but also at prescribing foods that inhibit the secretion of gastric juice and limiting the intake of calcium. For phosphaturia due to urinary tract infection, an acidifying milk-meat diet is used.
Allowed are butter, vegetable oil, rice, semolina, pasta, premium and first grade flour, potatoes, cabbage, carrots, cucumbers, beets, tomatoes, apricots, watermelon, pears, plums, strawberries, cherries. Limited to: beef, pork, boiled sausage, eggs, corn grits, second grade flour, milk, sour cream. Excluded are cheese, cottage cheese, beef liver, chicken, fish, caviar, beans, peas, chocolate, oatmeal, pearl barley, buckwheat, millet. In case of combined metabolic disorders (i.e. when there are several types of salts), the diet is prescribed individually.
The complex of therapeutic measures includes medications prescribed by a doctor, vitamins A and E.
Forecast
The prognosis for dysmetabolic nephropathy is generally favorable. In most cases, with the appropriate regimen, diet and drug therapy, it is possible to achieve stable normalization of the corresponding parameters in the urine. In the absence of treatment or if it is ineffective, the most natural outcome of dysmetabolic nephropathy is urolithiasis and kidney inflammation.
The most common complication of dysmetabolic nephropathy is the development of urinary tract infections, primarily pyelonephritis.
If you experience any of the symptoms listed above (impaired urination, changes in the properties of urine, pain), you should immediately consult a doctor for help.
Remember that it is very important to start treatment in the early stages of the disease, since NMO in the kidneys is a predominantly reversible condition, and in the absence of treatment, the result is the development of urolithiasis and pyelonephritis.
Recommendations
To prevent the development of the disease, as well as relapse, it is necessary to adhere to a proper, balanced and regular diet - avoid spicy foods, marinades, etc. During an exacerbation, patients are recommended to follow a gentle diet that meets the requirements of the biochemical type of nephropathy (oxalate, urate, etc.).
In order to prevent relapses, all patients are recommended to consult a nephrologist or urologist once a quarter for the necessary correction of drug therapy and nutritional recommendations.
Patients suffering from long-term NMO in the kidneys are at increased risk according to ICD. Therefore, during the period of remission, they need to undergo annual control examinations (general urinalysis, urine biochemistry, ultrasound of the kidneys, ureters, bladder) of the urinary system as prescribed by the doctor.
Interpretation:
- Hyperparathyroidism; vitamin D-resistant rickets; immobilization after paraplegia or fracture; vitamin D intoxication; damage to the renal tubules (for example, Fanconi syndrome); familial hypophosphatemia; non-renal acidosis (increased excretion of phosphates as a buffer for urine); predisposition to the formation of urinary stones; leukemia
- Hypoparathyroidism; pseudohypoparathyroidism; parathyroidectomy; acromegaly; bone metastases; infectious diseases, in particular tuberculosis; acute yellow atrophy.
Sample result (PDF)
FAQ
Are NMOs curable?
NMO is often caused by hereditary metabolic disorders, which requires constant adherence to at least dietary recommendations.
What causes the disease?
NMO may be associated with a hereditary predisposition, as well as with diseases of internal organs (gastrointestinal problems, blood diseases, etc.), and the use of certain groups of medications (diuretics, cytostatics, etc.).
Is the disease a contraindication to pregnancy?
CME in the kidneys itself requires observation throughout the entire period of pregnancy in compliance with dietary recommendations.
With the development of urolithiasis, pyelonephritis and their complications in the form of chronic renal failure, the possibility of pregnancy and its preservation depends on the exacerbation of the process and the stage of complications and is decided in each specific case.
Can kidney disease manifest as decreased potency?
Of course, CME does not directly affect potency, but in the event of complications of urolithiasis, kidney inflammation, or the development of chronic renal failure, a decrease in potency may appear as a reaction to a chronic disease.
Interference:
- Anabolic steroids, androgens, beta-blockers (eg, acebutol, pindolol), estrogens, ergocalciferol, furosemide, growth hormone, hydrochlorothiazide, methicillin (for nephrotoxicity), phosphates, sodium etidronate, tetracycline (for nephrotoxicity),
- Acetazolamide, albuterol, aluminum-containing antacids, amino acids, anesthetics, calcitonin, carbamazepine, epinephrine, estramustine, fructose, glucocorticoids, glucose, hydrochlorothiazide (long-term use), ifosfamide, insulin, isoniazid, oral contraceptives, phenytoin, sucralfate