Full text of the article:
Examinations that provide information about the state of the gastrointestinal tract cannot be called pleasant procedures. Colonoscopy and gastroscopy are very often a reason for patients not to contact specialists. But modern medicine suggests performing a colonoscopy and FGDS under anesthesia at the same time, thereby relieving the patient of such unpleasant sensations and even minimal pain.
Indications and contraindications for gastroscopy under anesthesia (during sleep)
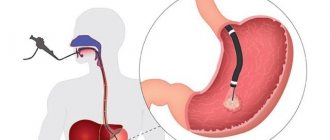
Gastroscopy
- This is one of the types of endoscopic examination. During the study, the endoscopist examines the mucous membrane of the esophagus and stomach, and, if necessary, other organs of the upper gastrointestinal tract. At the Central Clinical Hospital of the Russian Academy of Sciences, modern protocols and examination programs are used for gastroscopy, and the latest equipment is used.
As a rule, endoscopy is prescribed when the following signs of gastrointestinal diseases appear:
- burps of air;
- belching sour, bile, small amounts of food;
- sour, metallic, musty taste in the mouth;
- appetite disorders;
- nausea;
- heartburn;
- pain and other discomfort in the abdomen;
- pain when pressing on the abdomen;
- the appearance of discomfort after eating;
- cutting or aching pain on an empty stomach;
- bloating;
- difficulty swallowing;
- difficult or painful passage of food through the esophagus;
- bowel disorders;
- blood in stool;
- regular feeling of incomplete bowel movement.
Periodic EGD is necessary in the presence of chronic diseases to monitor changes in the patient's condition, assess the progress or regression of pathological changes. This type of examination is included in the dispensary program in the presence of such chronic diseases as:
- gastroptosis;
- gastritis of various nature;
- ulceration, scarring of the gastric mucosa;
- deformation of the biliary tract and other pathologies that can affect the general condition of the gastrointestinal tract.
Endoscopy allows you to identify incipient pathological changes in the tissues and mucous membranes of the gastrointestinal tract and detect in time:
- tumors;
- polyps;
- bleeding;
- changes in the gastric mucosa;
- gastroptosis;
- ulcers and perforations of the stomach;
- and other pathological changes.
There are several types of endoscopic examination. Esophagoscopy is prescribed if necessary to assess the condition of the esophagus. During gastroscopy, the stomach is examined. Esophagogastroduodenoscopy allows you to study the condition of the esophagus, stomach and duodenum.
The endoscopic method makes it possible to perform not only examinations, but also treatment procedures (if necessary) in a short time and with a minimum of complications:
- elimination of polyps;
- stopping bleeding;
- endobiliary manipulations for diseases of the pancreas and bile ducts.
To perform gastroscopy, a special flexible probe with a camera is inserted into the esophagus through the mouth, which captures the image along its path and transmits it to the monitor. Due to this, during the procedure the doctor can examine and assess the condition of the mucous membranes of the gastrointestinal tract in real time.
The procedure is very informative and is carried out quickly, that is, it allows you to obtain the most accurate data in a short time. However, gastroscopy without anesthesia has several features, due to which patients often refuse to perform this examination. This is primarily physical discomfort, due to which a person instinctively prevents the probe from moving through the esophagus, while resistance to the movement of the probe only increases the discomfort. In addition, gastroscopy without anesthesia often adversely affects the psychological state of the patient. Vomiting, stomach contractions and other factors complicate the examination, so today they try to carry out this procedure under anesthesia. The patient's condition is necessarily monitored by an anesthesiologist.
Advantages of performing gastroscopy under anesthesia:
- the patient does not experience psychological discomfort or unpleasant physical sensations;
- the physical reaction to the movement of the probe is reduced, which makes the study easier;
- the effectiveness of the examination increases (it is easier for the doctor to examine in detail all areas of the mucous membrane);
- Due to the absence of difficulties when advancing the probe, the procedure is faster.
Gastroscopy under anesthesia is to ensure the comfort and safety of the patient, as well as the accuracy of the examination results.
Using endoscopy during sleep, the doctor can conduct a painless examination of the mucous membranes:
- esophagus;
- stomach;
- duodenum.
Absolute contraindications to gastroscopy are heart attack, stroke and aortic aneurysm, bleeding disorders, mental illness, and spinal curvature. Relative contraindications are stage 3 hypertension and some other diseases of the cardiovascular system. The examination cannot be performed in case of acute respiratory tract diseases (sore throat, ARVI). As a rule, gastroscopy under anesthesia is not performed on children under 12 years of age. The final decision to prescribe an endoscopic examination is made by the gastroenterologist after reviewing the patient’s medical history.
Make an appointment
+7
Colonoscopy.
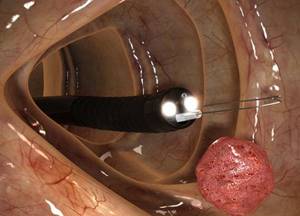
Colonoscopy is a diagnostic medical procedure for examining the colon from the inside, from its mucous membrane, using a special device - a colonoscope. Our clinic uses the OLYMPUS video colonoscope, Japan. This is a flexible, thin, long probe with a built-in video chip that allows you to transmit a color image from inside your body to a monitor. The image is transmitted in HD+ quality (high definition with precise detail and accurate color) with significant magnification, which allows the doctor not only to conduct an examination online and see all the nuances on the screen, but also to take still pictures, documenting the most important points of the examination necessary for further consultation with the doctor who prescribed the examination.
Colonoscopy is one of the most reliable and informative methods for examining the colon, providing not only diagnosis of the disease, but also the possibility of endoscopic treatment.
Indications for endoscopic examination of the colon are determined by a gastroenterologist, coloproctologist, therapist, surgeon, oncologist, or the endoscopist himself. This study is aimed at identifying inflammatory changes, diverticula (protrusions), polyps of the colon, as well as excluding its cancerous lesions and can be performed for both diagnostic and therapeutic purposes.
Diagnostic colonoscopy is performed if there are complaints of:
- Abdominal pain or pain in the large intestine.
- Frequently recurring constipation.
- Frequent bloating.
- Sharp weight loss.
- Bloody, mucous or purulent discharge from the anus.
- Anemia of unknown origin.
- Suspicion of the presence of a foreign body in the intestine.
In addition, diagnostic colonoscopy is performed for the purpose of observation to assess the condition of the mucous membrane of the organ over time, in the presence of polyps or after their removal through an endoscope; after surgery for colon tumors; in the presence of inflammatory diseases of the colon.
Diagnostic colonoscopy can be performed even if the patient has no complaints for screening purposes.
The main purpose of screening colonoscopy is to identify polyps (adenomas), formations that do not manifest themselves until they increase in size and develop into cancer.
According to international recommendations for screening for colorectal cancer, a colonoscopy should be performed on every healthy person starting at age 50 and repeated (if there are no changes during the initial colonoscopy) every 10 years. However, in people with additional risk factors (such as polyps, tumors, inflammatory diseases of the colon in relatives), it is recommended to perform the first study as early as 45 years of age and, depending on the changes detected, to conduct them at more frequent intervals.
A therapeutic colonoscopy is performed to treat diagnosed conditions, such as polyps, early forms of cancer, or a source of bleeding.
Preparing for a colonoscopy.
Before having a colonoscopy, you must go through the very important process of bowel preparation. This will allow you to perform a detailed examination of the entire colon and identify even small formations, as well as carry out the full range of necessary manipulations.
A week before the procedure.
1. Before the procedure, you may need to temporarily stop taking or change the dose of certain medications:
- If you take a medicine to thin your blood, such as to treat blood clots or prevent a heart attack or stroke, ask the doctor who prescribed the medicine when to stop taking it. Some examples of blood thinners are warfarin, heparin, clopidogrel.
- If you take insulin or other diabetes medications, you may need to change your dose. Ask the doctor who prescribed your diabetes medication what you should do the day before and the morning of your procedure.
- If you usually take laxatives for constipation, you will need to increase the amount you take one week before your colonoscopy. If you are not sure what to take or have any questions, contact your doctor.
- Iron supplements may make it difficult to see your bowels. They should be canceled 2-3 days before the procedure.
2. Select with your doctor the most suitable drug for bowel cleansing (FOTRANS, MOVIPREP).
3. Arrange for someone to drive you home after the procedure.
4. Follow a slag-free diet.
A zero-residue diet is a diet in which you eat very little foods that are high in fiber or foods that are difficult for your body to digest. Examples of foods high in dietary fiber include whole grain breads and cereals, nuts, seeds, and raw or dried fruit. By avoiding these foods before a colonoscopy, you can ensure that your colon is cleared for the procedure.
Three days before the procedure.
1. Pass all the necessary tests if your study will be carried out under sedation (in medicated sleep):
- General clinical blood tests with platelets.
- Indicators of the blood coagulation system (coagulogram).
- ECG with interpretation.
In case of failure to provide the necessary examination data or violation of the rules for preparing for the examination, the procedure may be cancelled.
Patients over 70 years of age are not allowed to undergo colonoscopy under general anesthesia.
2. Continue to follow a slag-free diet.
If you eat only easily digestible foods and start drinking a lot, you will be well prepared for the upcoming examination.
Two days before the procedure.
It is necessary to purchase a drug to prepare for colonoscopy and cleanse the intestines.
At the pharmacy of our medical center you can purchase FORTRANS and MOVIPREP drugs with a 5% discount.
One day before the procedure.
1. It is necessary to follow a diet of clear liquids.
Do not eat any solid food for the entire day before your procedure. Don't drink anything red, purple or orange. Drinking enough fluids is an important part of preparing for a colonoscopy.
2. Prepare a solution of the drug for bowel preparation.
The most effective scheme, using the example of the drug FORTRANS, providing the best quality of preparation and its easier perception, is presented below.
One FORTRANS pharmacy package contains 4 sachets. If your weight is up to 80 kg, use 3 sachets; if you weigh more, use all 4 sachets.
A solution for colon cleansing is prepared at the rate of: 1 sachet of FORTRANS per 1 liter of water. You cannot reduce the amount of liquid!
To improve the taste, you can add freshly squeezed citrus juice without pulp to the solution (1/2 orange or grapefruit per 1 liter of solution) or dissolve it in clear juice (apple), you can also dissolve it in iced tea. It is recommended to use the solution chilled.
Drink the solution gradually over an hour - 1 glass every 15 minutes in separate sips:
18:00 – 19:00 take 1 liter of FORTRANS solution.
19:00 – 20:00 take 1 liter of FORTRANS solution.
If it is difficult for you to take a volume of laxative (2 liters) within 2 hours or you experience a feeling of stomach fullness and nausea, you can increase the interval of taking the drug by 30-40 minutes in order to reduce nausea and prevent vomiting caused by taking a large amount liquids in a relatively short period of time.
Approximately 1 hour after starting to take the FORTRANS solution, loose stools will appear, not accompanied by painful sensations.
While taking FORTRANS solution, it is not recommended to lie down or sit for a long time. It is possible to do light housework and slow walking. If loose stools do not appear 4 hours after starting treatment or signs of an allergic reaction appear, you should contact the clinic’s medical staff or your doctor and refrain from taking the drug again.
On the day of the study.
1. Finish taking your bowel preparation solution.
5:30 – 6:30 take 1 liter of FORTRANS solution.
6:00 take simethicone 50 ml (for example, Espumisan), you can wash it down with water. Taking antifoaming agents (simethicone) will reduce foaming in the intestines, which will improve well-being during preparation and the quality of examination of the colon during colonoscopy.
6:30 – 7:30 take 1 liter of FORTRANS solution.
Bowel movement should end with the release of clear or slightly colored liquid 2-3 hours after taking the last dose of FORTRANS solution.
The specified start time for preparation must be changed depending on the time of the study.
It is important to remember that it is recommended to stop taking the drug no later than 3-4 hours before the start of the study!
2. Do not eat or drink anything after 8:00 on the morning of the procedure.
3. Take only the medications you were told to take on the morning of your procedure. Take them with a few sips of water.
4. Do not apply any lotion, cream, powder, makeup or perfume.
5. Remove all jewelry, including body piercings.
6. If you wear contact lenses, wear glasses instead.
7. Take your rescue inhaler if you have one.
8. You must come to the clinic 15 minutes before the start of the procedure to complete the Agreement and Informed Consent, as well as to pay for the procedure. Don't forget to take your passport or any other document proving your identity with you.
How is a colonoscopy performed?
The procedure is performed by a doctor together with a nurse.
If sedation (medication-induced sleep) is used, then an anesthesiological nurse and an anesthesiologist-reanimatologist are required to participate in the procedure, who administers a special drug to the patient. In our medical center, propofol is most often used. During medicated sleep, the patient does not experience pain or any discomfort.
The procedure takes on average 15 – 30 minutes and is carried out in a special room. You will need to remove all clothing from the waist down, including underwear, and you will be given special disposable underwear.
The examination is carried out while lying on your side. During the examination, the legs must be bent at the knees and moved towards the stomach. After anesthesia, the doctor inserts a video colonoscope into the anus and examines the walls of the large intestine, moving the probe and palpating along the surface of the abdomen, controlling the movement of the tube along the bends of the intestine. To make the picture more objective, the intestines expand with the help of supplied air. At the end of the study, the air introduced into the intestine will be removed by the doctor through a special channel of the colonoscope. If necessary, the doctor can also wash individual sections of the intestinal wall, but this takes research time, which is why high-quality intestinal cleansing performed by the patient is so important.
When performing a colonoscopy, it may be necessary to obtain tissue samples from the colon mucosa for subsequent examination under a microscope (histological examination). This procedure is called a biopsy. Biopsy results are usually ready in 7-10 days. Morphological examination of biopsy material allows for the most accurate diagnosis, including at the earliest stages of the disease.
In some cases, therapeutic procedures are also performed during colonoscopy, the most significant of which is the removal of a polyp (polypectomy).
After the procedure.
1. In the recovery room.
After the test is completed, the nurse anesthetist will continue to monitor your heart, breathing and blood pressure. When you are fully awake, the nurse will remove the IV line. After a colonoscopy, many patients experience a feeling of bloating and cramping in the abdominal area. This is normal and goes away after the gas is relieved. 2-3 hours after the procedure you can go home.
2. At home.
If you have had a biopsy, you may notice a few drops of blood from your rectum. This is normal after a biopsy, however it should not exceed a few drops and should not last more than 24 hours.
Drinking alcoholic beverages is prohibited for 24 hours after the procedure.
After 24 hours, you can return to your normal activities.
You can drink and eat light food 30 minutes after the test. Gradually transition to your normal diet. If your doctor wants to restrict your diet for a certain period of time, he will tell you about it.
If the procedure was performed under sedation, it is not recommended to drive a car, operate any machinery, or make important decisions for 24 hours after intravenous anesthesia.
If unusual symptoms or any alarming circumstances appear during the first hours and days after the examination, you should contact the clinic where the examination was performed and inform the doctor, especially if you:
- Body temperature is 38 degrees C or higher.
- Very severe pain or feeling of hardness in the abdomen.
- Bleeding from the rectum.
- Bleeding between bowel movements.
- Weakness, dizziness, nausea.
Possible risks.
Endoscopic examination is an invasive instrumental intervention. The risk of complications is extremely low (no more than 0.4%). Endoscopists, when conducting research, try to do everything possible to avoid complications and reduce this percentage to zero.
Undesirable consequences that may occur during this procedure include:
- Perforation of the organ.
- Pneumoperitorium (accumulation of gas in the free abdominal cavity).
- Bleeding.
- Respiratory and cardiovascular disorder.
- Allergic reactions.
- Exacerbation of a chronic disease.
If the above complications occur, hospitalization, emergency intensive, endoscopic and surgical treatment may be required.
Preparation for gastroscopy under anesthesia (in a dream)
Gastroscopy is prescribed by the patient's attending physician, usually a gastroenterologist. The procedure may be recommended after an MRI, in case of certain patient complaints, or in case of negative test results.
The study is usually carried out in the morning and is performed on an empty stomach. Eating is possible no later than 7 hours before the examination. You must refrain from smoking for at least 2 hours: it irritates the gastrointestinal mucosa, which negatively affects the accuracy of the study. During the examination, the patient lies on his left side, with a cushion placed under his head. When performing gastroscopy without anesthesia, immediately before the procedure, the patient receives local anesthesia: the oral cavity and pharynx are treated with lidocaine in the form of an aerosol. When performing gastroscopy under general anesthesia, intravenous anesthesia is used. With this type of examination, the patient is asleep, so he does not experience any discomfort when the doctor inserts a probe into the oral cavity, esophagus and stomach. To perform endoscopy under anesthesia, hospitalization for several hours in a day hospital is required. The duration of an endoscopic examination depends on its type and purpose. As a rule, the procedure takes from 5–7 minutes in the absence of serious pathological changes to 15–30 minutes in the presence of multiple disorders or the need to perform any therapeutic manipulations.
Evaluation of endoscopy results
The endoscopist deciphers the data obtained during the study and interprets it, and the final diagnosis and prescription of the course of treatment is carried out by the attending doctor, usually a gastroenterologist.
During the study, the doctor fills out a medical form, recording information about the condition:
- color of the mucous membrane, density, integrity, patency of the esophagus (normally there should be no adhesions or scar tissue);
- cardia of the stomach (this is the zone of connection of the esophagus with the stomach; in a healthy person it closes, but with gastroesophageal reflux it does not close);
- folds of the stomach - their color and integrity, as well as the size and location of pathological changes (if any);
- peristalsis;
- stomach contents (normally it is transparent, in the presence of pathologies it can be dark green, scarlet or otherwise colored);
- the pylorus, or pyloric region (in a healthy person this area is passable and unchanged; if a tumor or scar formation is detected, the doctor describes the nature and size of the lesion).
After gastroscopy, a second appointment with a gastroenterologist is required. If necessary, the doctor may prescribe additional diagnostic procedures: tests, MRI and others.
The following diagnostic procedures are performed at the Central Clinical Hospital of the Russian Academy of Sciences:
- taking a biopsy;
- intragastric pH-metry;
- chromoscopy;
- determination of the presence of Helicobacter pylori bacteria using an express method;
- NBI examination of the mucous membrane to detect pathological changes in the initial stages.
Based on the data obtained during the study, the doctor makes a diagnosis and prescribes a further treatment program.
Hysteroscopy.
Hysteroscopy is the only modern examination method that allows using a special optical device (hysteroscope) to examine the inner surface of the uterus. This procedure is quite quick, painless and extremely informative.
Indications for hysteroscopy:
- Menstrual irregularities.
- Bleeding during postmenopause.
- Suspicion of the presence of intrauterine pathologies.
- Infertility.
- Miscarriage.
- Control studies after surgery or after drug therapy.
Preparation and performance of hysteroscopy.
The best time to perform diagnostic hysteroscopy is days 9-13 of the menstrual cycle.
Before the procedure, it is necessary to carry out a series of tests and studies prescribed by a gynecologist.
No special preparation is required. The study is carried out on an empty stomach, no earlier than 6 hours after the last meal and water.
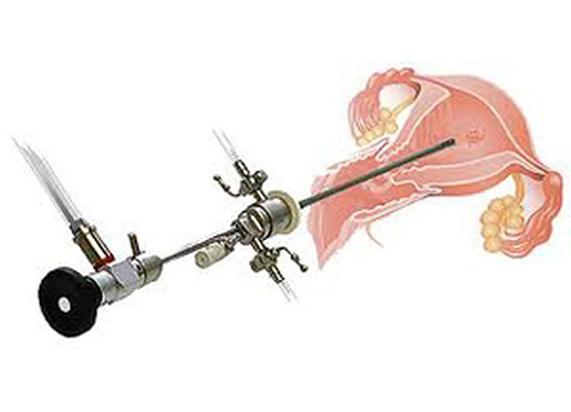
As a rule, hysteroscopy is performed on an outpatient basis under local anesthesia. During the procedure, an ultra-thin tube with a diameter of about 3 mm is inserted into the uterine cavity through the vagina, the cervical canal, with a video camera at the end, allowing the gynecologist to assess the condition of the internal surface of the organs on the monitor screen.
Diagnostic hysteroscopy lasts 5–10 minutes. During this time, the specialist confirms or refutes the presumptive diagnosis. If necessary, the doctor may take a biopsy or remove polyps. To carry out these manipulations, special channels are provided inside the hysteroscope tube for introducing miniature instruments. In this case, the procedure can last up to 30 minutes. All collected material is transferred for further research by histologists.
After hysteroscopy.
Almost immediately after the procedure, the patient returns home. In the first 2-4 days, slight cramps in the lower abdomen may be felt, and bloody discharge is possible. If necessary, the doctor may prescribe painkillers and antibiotics.
Most patients can start working the very next day after the procedure.
However, after diagnostic hysteroscopy for several days, to minimize the risks of infection and the development of inflammatory processes, you should refrain from sexual intercourse and physical activity; it is not recommended to use tampons, douche, or take a bath.
After a biopsy and removal of polyps, this period can last up to two weeks.
Contraindications:
- Inflammatory processes in the pelvic organs.
- Pregnancy.
- Heavy uterine bleeding.
- Stenosis (sharp narrowing) of the cervix.
- Pathological changes in the cervix.
- Viral diseases are in the acute stage.
Gastroscopy at the Central Clinical Hospital of the Russian Academy of Sciences (in a dream)
At the Central Clinical Hospital of the Russian Academy of Sciences, modern equipment is used to perform gastroscopy; the examination is carried out by a highly qualified endoscopist. When performing gastroscopy under anesthesia, the patient's condition is monitored throughout the entire study by an experienced anesthesiologist. After completing the procedure, the patient spends several hours in a comfortable day hospital at the clinic - this is necessary to monitor his condition while recovering from anesthesia.
Advantages of visiting the RAS clinic:
- reliable protection of personal data;
- highly qualified endoscopists;
- consultations with doctors of the highest qualification category;
- attentive and caring nursing staff;
- modern equipment;
- quick receipt of examination results;
- the possibility of performing gastroscopy in a dream.
After undergoing gastroscopy, a consultation with a gastroenterologist is necessary. At the Central Clinical Hospital of the Russian Academy of Sciences, consultations are conducted by doctors with extensive experience in clinical practice - professors, doctors of medical sciences. The study of modern therapeutic and diagnostic methods allows our specialists to detect diseases of the stomach and other digestive organs at the earliest stages and begin treatment on time. This allows us to achieve positive results in the treatment of most gastrointestinal pathologies: both common and rare.
Appointment with a gastroenterologist – 2000 rubles.
+7 (499) 400-47-33
Prices for services at the Central Clinical Hospital of the Russian Academy of Sciences
| Primary appointment (examination, consultation) with a gastroenterologist | 2000 rub. |
| Gastroscopy | 3000 rub. |
| Colonoscopy under sedation | 13000 rub. |
| Gastroscopy under sedation | 11000 rub. |
| Colonoscopy and gastroscopy under sedation (comprehensive service) | 16,000 rub. |
| Additional services | |
| Taking material for biopsy | 750 rub. |
| Biopsy | 2500 rub. |
| ECG | 1000 rub. |
| Determination of urease activity of a biopsy of the gastric or duodenal mucosa for Helicobacter pylori (HELPIL test) | 2150 rub. |
| Appointment with a gastroenterologist | 2000 rub. |
| Appointment with a coloproctologist | 2000 rub. |
Prices
- Endoscopy
EFGDS (videoesophagogastroduodenoscopy)
1850.00 rub.
EFGDS (videoesophagogastroduodenoscopy) under intravenous anesthesia (without the cost of anesthetic)
5050.00 rub.
Video sigmoidoscopy
1950.00 rub.
Colonoscopy (video colonoscopy)
3550.00 rub.
Colonoscopy (video colonoscopy) under intravenous anesthesia (without the cost of anesthetic)
7550.00 rub.
Colonoscopy (video colonoscopy) under intravenous anesthesia “all inclusive”
10200.00 rub.
Simultaneous video esophagogastroduodenoscopy and colonoscopy under anesthesia
12500.00 rub.
Recording research results on electronic media (with the cost of USB Flash, 4 GB)
550.00 rub.
Endoscopic polypectomy of the stomach, esophagus, duodenum of category II (1 polyp 0.6 – 1.0 cm) (without the cost of histological examination)
6550.00 rub.
Endoscopic polypectomy of the stomach, esophagus, duodenum of category I complexity (1 polyp up to 0.4 - 0.6 cm) (without the cost of histological examination)
4850.00 rub.
Endoscopic polypectomy during colonoscopy: formation less than 6 mm (without the cost of histological examination)
1550.00 rub.
Endoscopic polypectomy during colonoscopy: formation 6 - 10 mm (without the cost of histological examination)
2050.00 rub.
Endoscopic polypectomy during colonoscopy: formation more than 10 mm (without the cost of histological examination)
2550.00 rub.
Endoscopic EZ-Clip hemostatic clips (Olympus, 1 pc.)
1250.00 rub.