Currently, a relatively new laboratory indicator, namely leukocyte esterase in urine, is becoming increasingly important. What does this study mean? What is it used for, and what routine and long-known tests can it replace?
The name itself—with the ending of the word “-aza”—denotes the name of the enzyme, or enzyme. In laboratory clinical practice, many enzymes are studied, but almost all of them are determined in blood serum. These are alpha-amylase, alanine aminotransferase (or ALT), lactate dehydrogenase (LDH), creatine phosphokinase (CPK), aspartate aminotransferase (AST), and many other enzymes. They enter the blood from various parenchymal organs, since they are synthesized in their cells, from muscle and glandular tissue. Thus, ALT and AST mainly enter the peripheral bloodstream from the liver, lactate dehydrogenase from muscle tissue, and so on.
There are no enzymes in urine at all. After all, it is not the internal environment of the body, in which certain necessary compounds are regularly found, but, in simple terms, waste. Quite simple molecules are secreted into the urine; many of the beneficial substances are reabsorbed into the blood (tubular reabsorption) so as not to lose anything unnecessary. So where does the enzyme come from, and what is leukocyte esterase in urine?
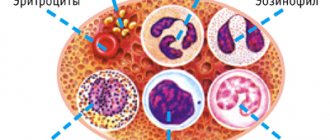
As the name suggests, this enzyme somehow belongs to leukocytes, or white blood cells, which have a protective function. But how did it get into the urine? Let's try to figure this out.
Norm of leukocytes in urine
Leukocytes are produced in the bone marrow, from where they enter the blood, where they protect the body from viruses and bacteria for a week to 20 days, and then die and are eliminated, including in the urine.
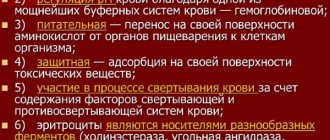
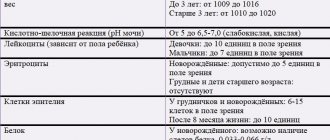
In a general urine analysis of a healthy man, the microscope will detect no more than 3 leukocytes. Women may have slightly more leukocytes - up to 6 pieces. A larger number is an alarming symptom. With the Nechiporenko test, the normal level of leukocytes is no more than 2000 cells per 1 ml (in women, up to 4000 cells are allowed). For children, reference values differ from those for adults. So, for infants, the normal indicator of white blood cells will be up to 8 leukocytes in the field of view of the microscope (for a general urine test). This amount may increase as your baby teethes.
In older children, normal values approach those in adults. To decipher children's results, there is a special table, according to which the normal number of leukocytes is:
- up to 28 days of life: 5-7 for boys, 8-10 for girls;
- up to one year: 5-6 for boys, 8-9 for girls;
- from one year: 0-5 for boys, 0-6 for girls.
In general, the lower your white blood cell count, the better. Above is a generally accepted scheme for interpreting the results of leukocyte levels in a general urine test, but some doctors are confident that any increase in their level above 3 in people of any gender and age is a reason for a thorough examination.
Free consultation with a urologist
Urinalysis helps identify hidden diseases that occur without obvious signs and symptoms, such as diabetes mellitus, various forms of glomerulonephritis and chronic urinary tract infections.
The most economical method of rapid urine analysis is a paper or plastic test strip. This simple microchemical system allows you to perform qualitative and semi-quantitative urine analysis in a minute. Results are determined by the change in color of each segment of the test strip compared to the table. Microscopic analysis of urine requires only a relatively inexpensive lightweight microscope.
Macroscopic urine analysis
The first stage of a urine test is a visual examination of the urine. Normal urine color ranges from pale yellow to dark yellow or amber, and the urine is clear. The normal volume of urine per day is 750–2000 milliliters.
Cloudiness or sediment may be caused by large numbers of cells or protein in the urine, or may result from crystallization or precipitation of salts when urine is stored at room temperature or in the refrigerator for long periods of time. If, after adding a small amount of acid, the cloudiness disappears, then the cloudiness of the urine is due to precipitation (precipitation) of salts.
Red or red-brown urine may be caused by food dyes, eating fresh beets, medications, or the presence of hemoglobin or myoglobin in the urine. If the urine test contains a lot of red blood cells (RBCs), the urine sample will not only be red, but also cloudy.
Chemical analysis of urine using test strips
pH factor in urine analysis
The glomerular filtrate of blood plasma is usually oxidized in the renal tubules and collecting ducts from a pH of 7.4 to approximately pH 6 in the final urine. However, depending on the acid-base state in the body, the pH factor of urine can vary from 4.5 to 8.0. A change in acidity from 7.4 is achieved in the distal convoluted renal tubules and collecting ducts.
Specific gravity
Specific gravity (a mass that is directly proportional to urine osmolarity and measures the concentration of a solution) measures the density of urine, or the ability of the kidneys to concentrate or dilute urine. There is a quick method for determining the specific gravity of urine using test strips. Most laboratories measure urine specific gravity using a refractometer.
A specific gravity in the range of 1.002 to 1.035 in a random sample is considered normal with normal renal function. Starting with a specific gravity of the glomerular filtrate ranging from 1.007 to 1.010, any change below this range indicates hydration, and any change in urine specific gravity above 1.010 indicates relative dehydration.
If the specific gravity of urine is not > 1.022 after a 12-hour period without food or water, then the ability of the kidneys to concentrate urine is reduced, that is, the patient suffers from chronic renal failure or nephrogenic diabetes insipidus. In end-stage renal failure, the specific gravity of urine ranges from 1.007 to 1.010.
If the urine has a specific gravity greater than 1.035, the sample is either contaminated, contains a large amount of glucose, or the patient has recently received intravenous X-ray contrast agent or low molecular weight dextran (blood substitute) solution. Subtract 0.004 for every 1% glucose to determine the concentration of the glucose-free solution.
Protein in urine test
Protein in urine is determined using test strips, but quantitation of protein in urine is done from the supernatant after centrifugation, since cells present in normal urine may give false results of high protein levels. Normally, only low molecular weight plasma proteins are filtered in the glomeruli and then reabsorbed in the renal tubules. However, small amounts of plasma proteins and a protein secreted in the nephron (Tamm-Horsfall protein) can be detected in normal urine. Total protein excretion normally does not exceed 150 mg per day or 10 mg per 100 ml in a single urine sample. Protein excretion of more than 150 mg per day is defined as proteinuria. Proteinuria of more than 3.5 grams per day is severe nephrotic syndrome.
Protein in urine is determined using test strips impregnated with the indicator, bromophenol blue, which are most sensitive to albumin, but do not respond to the appearance of globulins or Bence Jones protein in the urine. Heat precipitation is the best semi-quantitative but not very sensitive method. The sulfosalicylic acid test is a more sensitive precipitation test. This test detects albumins, globulins and Bence Jones protein in low concentrations.
Positive results are assessed in comparison with the norm of 10 mg in 100 ml or 150 mg per day (upper limit of normal): + corresponds to 200 – 500 mg per day, ++ corresponds to 0.5 – 1.5 grams of protein per day, +++ - 2-5 grams of protein per day, ++++ corresponds to more than 7 grams of protein per day.
Glucose in urine analysis
Normally, less than 0.1% glucose is detected in the urine, which is filtered in the renal glomeruli (<130 mg per day). Glucosuria (excess sugar in the urine) is a symptom of diabetes. Glucose in urine is detected using glucose oxidase test strips. The method is quite specific and sensitive, but may miss the appearance of other sugars in the urine, such as galactose and fructose. Therefore, other methods for determining sugars (such as Clinitest, modified Benedict test) are used to analyze urine in newborns and infants.
Ketones in urine analysis
The presence of ketones (acetone, acetoacetic acid, beta-hydroxybutyric acid) in the urine is a result of either diabetic ketosis or some other form of calorie deprivation (fasting) and is easily detected using sodium nitroprusside test strips or tablets.
Nitrites in urine analysis
A positive nitrite test indicates that bacteria are present in significant quantities in the urine. Gram-negative bacteria such as E. coli are more likely to test positive.
Leukocyte esterase in urine analysis
A positive leukocyte esterase test means that there are white blood cells in the urine. The test is positive even after destruction of leukocytes. Pyuria can be detected even if the urine sample contains damaged or destroyed white blood cells. A negative leukocyte esterase test means that infection is unlikely and that, without further testing, namely urine microscopy and/or urine culture, significant bacteriuria cannot be ruled out and a urinary tract infection cannot be concluded.
Microscopic urine analysis
Methodology
A urine sample (usually 10-15 ml) is centrifuged in a tube at a relatively low speed (approximately 2-3,000 rpm) for 5-10 minutes. Discard the supernatant liquid. The precipitate is shaken by gently tapping the bottom of the test tube on the table. A drop of the resulting suspension is applied to a glass slide, covered with a coverslip and examined under a microscope.
Study
The sediment is first examined under a low power microscope to determine the presence of most crystals, casts, epithelial cells, and other large objects. The number of cylinders is usually defined as the number of each type of cylinder found in the field of view (LPF, low power field). For example: 5-10 hyaline casts per field of view (casts/LPF). Since the number of elements in each field of view may vary, the average number of elements is given. Then, a high magnification examination is carried out in order to identify crystals, cells and bacteria. The different cell types are usually described as the number of cells of each type found in the field of view (HPF, high power field). Example: 1-5 leukocytes per field of view (WBC/HPF).
Red blood cells (erythrocytes)
Blood in the urine (hematuria). The presence of even a few red blood cells in the urine is a sign of pathology. The causes of blood in the urine are: glomerular damage, kidney and urinary tract tumors, kidney injuries, urinary tract stones, kidney infarction, acute tubular necrosis, upper and lower urinary tract infections, nephrotoxins, heavy physical activity. Red blood cells can enter the urine from the vagina in women during menstruation or as a result of trauma during bladder catheterization. In theory, red blood cells should not be present in a urine sample, but they can sometimes appear in the urine even in very healthy people. However, if one or more red blood cells are found in the high power field and contamination can be ruled out, then the preparation is probably incorrect.
Red blood cells in urine may have a normal shape, swell when exposed to dilute urine (in fact, only the cell membrane and free hemoglobin remain), or shrink when exposed to concentrated urine. Both swollen, partially hemolyzed, and shriveled red blood cells in the urine are sometimes difficult to distinguish from leukocytes in the urine. In addition, red blood cell membranes are difficult to differentiate from yeast fungi. The presence of altered red blood cells suggests damage to the glomeruli, such as glomerulonephritis. The changed red blood cells (erythrocytes) have an irregular shape due to their passage through the affected glomeruli.
Red blood cells in urine analysis. Changed red blood cells in urine analysis
Leukocytes
Pyuria is the presence of a large number of leukocytes in the urine, which appear with infections of the upper or lower urinary tract, or acute glomerulonephritis. Typically, leukocytes are granular cells. White blood cells can contaminate the urine, especially if the vagina, cervix, or urethra (urethra) is inflamed.
If two or more white blood cells in each high-resolution field of view appear in uncontaminated urine, the test is probably incorrect. Leukocytes have lobulated nuclei and granular cytoplasm.
Leukocytes in urine analysis
Epithelial cells
Renal tubular epithelial cells, usually larger than granulocytes, contain large round or oval nuclei and are normally excreted in the urine in small quantities. However, in nephrotic syndrome, under conditions leading to degeneration of the renal tubules, the number of epithelial cells in the urine increases sharply.
If lipiduria occurs, the epithelial cells contain endogenous fats. When epithelial cells are filled with numerous droplets of fat, such cells are called oval fat bodies. With polarized light microscopy, oval fat bodies are revealed in the form of a “Maltese cross”.
Transitional epithelial cells from the renal pelvis, ureter, or bladder have clearer boundaries, larger nuclei, and are smaller in size than squamous epithelial cells. The epithelial cells of the renal tubules are smaller, more rounded in shape than transitional epithelial cells, and their nucleus occupies almost the entire volume of the cell.
Squamous epithelial cells appear in the urine from the surface of the skin or from the outer part of the urethra.
Their significance is that their appearance suggests possible contamination of the urine test with skin flora.
Various cells in urine analysis
Cylinders
Urinary casts form only in the distal convoluted tubules or collecting ducts (distal nephron). Casts are not formed in the proximal convoluted tubules and loop of Henle. Hyaline casts are composed primarily of Tamm–Horsfall protein, which is secreted by renal tubular cells.
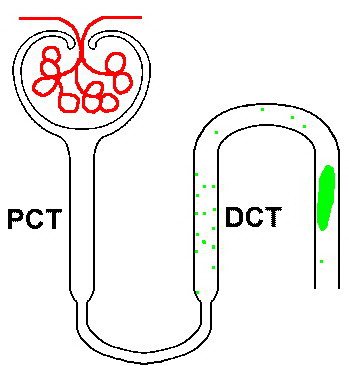
Loop of Henle
Even with glomerular injury, in which glomerular permeability to plasma proteins increases and proteinuria appears, most of the basis of the urinary casts is Tamm-Horsfold protein, although albumin and some globulins are also included in the composition of the casts.
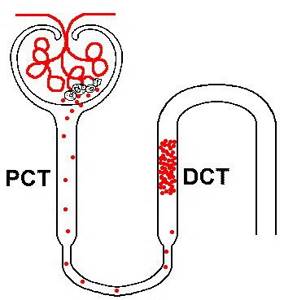
Loop of Henle
Factors that promote the formation of protein casts include decreased renal blood flow, high salt concentrations, and low pH. These factors promote denaturation and precipitation (precipitation) of proteins, especially the Tamm–Horsfold protein. Protein cylinders with long, thin tails that form at the junction of the loop of Henle and the distal convoluted tubule are called cylindroids. Hyaline casts can be found in the urine even in healthy patients.
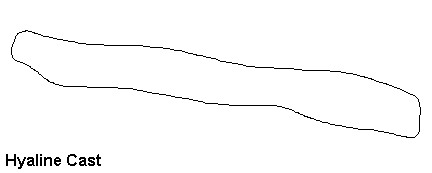
Hyaline casts in urine
Red blood cells can stick together and form red blood cell casts. Such casts are a sign of glomerulonephritis with blood leaking from the glomeruli, or severe damage to the renal tubules.
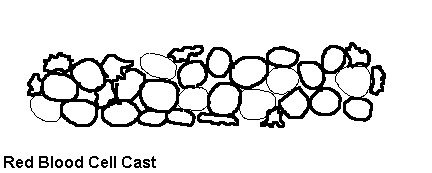
Red blood cell cast in urine
Leukocyte casts are typical of acute pyelonephritis, but can also appear with glomerulonephritis. Their presence indicates inflammation of the kidney, because such casts form only in the kidneys.
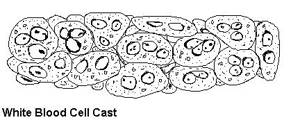
Leukocyte cast in urine
If the cell casts remain in the nephron for some time before entering the bladder, the cells break down and form coarse granular casts, then fine granular casts, and eventually waxy casts. Granular and waxy casts are formed from the cell casts of the renal tubules. Wide casts are believed to originate from damaged and dilated tubules and therefore appear in the final stages of chronic kidney disease.
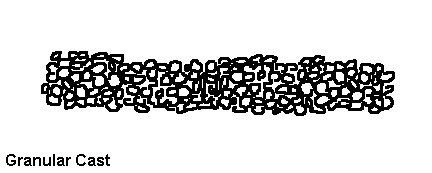
Grainy casts in urine
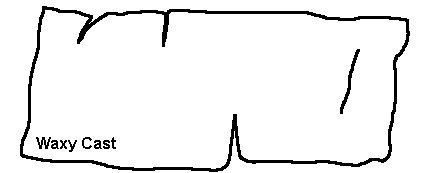
Waxy casts in urine
The so-called telescopic urinary sediment contains red blood cells, leukocytes, oval fat bodies and all types of casts in more or less equal proportions. Conditions that can lead to telescopic urinary sediment are: 1) lupus nephritis (lupus nephritis), 2) malignant hypertension, 3) diabetic glomerulosclerosis, and 4) rapidly progressive glomerulonephritis.
In the last stage of all kidney diseases, the urinary sediment often becomes very scanty because the few remaining nephrons produce dilute urine.
Bacteria
Bacteria usually appear in urine tests due to the abundant normal microflora of the vagina or anterior segment of the urethra, as well as due to the ability to multiply rapidly in urine at room temperature. Therefore, bacteria detected in any urine test other than a carefully collected urine sample must be interpreted based on the clinical presentation.
Diagnosis of bacteriuria in suspected urinary tract infections requires urine culture. The number of colonies must be counted to determine the number of bacteria. A bacterial count greater than 100,000/mL in one urine test reflects significant bacteriuria. Many microorganisms reflect pollution. However, the presence of any bacteria in urine samples collected by catheter or after suprapubic puncture is considered significant bacteriuria.
Yeast
Yeast in urine analysis
Yeast cells can contaminate the urine or be a true yeast infection. They are often difficult to distinguish from red cells and amorphous crystals. Yeast spores are arranged in clusters, have a greenish glow, and are often oval in shape. The most common fungus is Candida, which can affect the bladder, urethra or vagina.
Crystals
Crystals that may occur in the urine even in healthy patients include calcium oxalate, ternary phosphate crystals, and amorphous phosphate crystals.
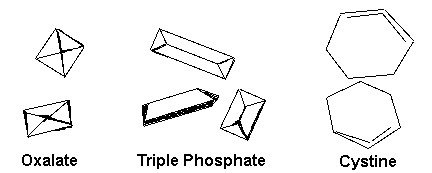
Crystals in urinalysis (oxalate crystals in urine, tripelphosphate in urine, cystine crystals in urine)
Uncommon crystals include: cystine crystals in the urine of newborns with congenital cystinuria or severe liver disease, tyrosine crystals with congenital tyrosinosis or renal failure, or leucine crystals in patients with severe liver disease or maple syrup disease (valinoleucinuria, Menkes syndrome).
Miscellaneous
Urine that looks like curdled milk or unidentifiable objects may be found in the urine sample, especially if patients collect urine samples at home.
Sperm may be found in a urine test. Rarely, pinworm eggs may be found in the urine. In Egypt, schistosome eggs can be detected in urine in cases of schistosomiasis of the bladder.
Methods for collecting urine samples
Random urine sample taken throughout the day, without precautions for contamination: The urine sample may be dilute, isotonic, or concentrated and may contain white blood cells (leukocytes), bacteria, and squamous epithelial cells as contaminants. In women, a urine sample from the vagina may be contaminated with: red blood cells from menstruation, trichomonas, or yeast.
Typically, a urine test is collected early in the morning before eating or drinking any liquid. Morning urine is usually concentrated and reflects the kidneys' ability to concentrate urine during overnight dehydration. If you do not drink liquid from 18:00 on the eve of collecting a urine test, then in healthy people the specific gravity of urine does not exceed 1.022.
The middle portion of urine is collected after toileting the external opening of the urethra (urethra). To treat the external opening, use a cotton sponge soaked in benzalkonium hydrochloride, which does not irritate the skin in the genital area. The first portion of urine is passed, the next portion of urine is collected in a special container, and then urination is completed. The first load of urine washes away cells and bacteria from the anterior segment of the urethra so that contaminants are not introduced into the urine sample. It seems simple, but it's not (try it before criticizing the patient).
Bladder catheterization for urine collection is performed only in special circumstances, such as in a comatose or confused patient.
Catheterization may cause infection and trauma to the urethra and bladder, thereby causing iatrogenic infection or hematuria.
Suprapubic puncture of the bladder. When performed under ideal conditions, suprapubic puncture provides the cleanest method of collecting a urine sample from the bladder. This is a good method for babies and small children.
Summary
It can be concluded that a properly collected midstream urine sample after toileting the external urethral meatus is suitable for a complete urinalysis. In fact, this urine sample is sufficient even for urine culture. If determination of renal concentrating ability is desired, a period of dehydration may precede urinalysis collection, but any specific gravity > 1.022 measured in a random urine sample indicates adequate renal concentrating capacity if there are no abnormal solutions in the urine.
Another important factor is the length of time that elapses from urine collection to laboratory testing. Changes that occur over time after a urine sample is collected include:
- decrease in transparency due to crystallization of solutions,
- increase in pH factor,
- destruction of ketone bodies,
- destruction of bilirubin,
- decomposition of cells and casts, and
- excessive bacterial growth.
In general, a urine test may not reflect the results of completely fresh urine unless the urine sample is delivered to a laboratory for testing within one hour of collection. Therefore, take the urine to the laboratory as quickly as possible.
The article is for informational purposes only. For any health problems, do not self-diagnose and consult a doctor!
Author:
V.A. Shaderkina is a urologist, oncologist, scientific editor of Uroweb.ru. Chairman of the Association of Medical Journalists.
‹ Diagnostics in urology Up Analysis of daily urine (daily diuresis) ›
Elevated white blood cells in urine
Elevated leukocytes are a signal of the inflammatory process.
However, false leukocyturia associated with improper collection of biomaterial often occurs. For a general analysis, an average portion of morning urine is required. Before collecting it, you need to thoroughly wash the external genitalia with water at room temperature and pat the skin dry. Hot water, active friction, washing with a washcloth can trigger the release of leukocytes and lead to a falsely elevated result. There are other physiological reasons that may affect the test results:
- excessive physical activity;
- frequent visits to the bathhouse;
- insufficient hygiene;
- use of certain medications (antibiotics and anti-inflammatory drugs).
If the collection of biomaterial was performed correctly, and there were no external factors influencing the results, but the level of leukocytes is higher than normal, then an inflammatory process is present.
Moreover, any parts of the urinary tract can become inflamed: the urethra, ureters, bladder, kidneys. Inflammation is often caused by pathogenic microorganisms, which will also be identified during the analysis. If bacteria are found in the urine, an antibiotic sensitivity culture needs to be done to determine the most effective and safe treatment. Some of the most common causes of elevated white blood cells in urine are:
- A urinary tract infection is the most likely cause of white blood cells in the urine. With any infection, the immune system increases the production of white blood cells to fight bacteria. More than half of women and about one in five men will experience a UTI in their lifetime. Symptoms of a urinary tract infection: pain or burning when urinating, urinating more frequently, pain in the abdomen, back or side, cloudy urine.
- Urolithiasis disease. Most often, urolithiasis develops in people aged 20–45 years, and men suffer from it 2.5-3 times more often than women. As the stone moves down the ureter, it scratches the surrounding tissue. In response to this damage, more white blood cells are released into the blood.
- Diabetes. People with diabetes are more likely to experience asymptomatic bacteriuria.
- Damage to the glomeruli (glomerulonephritis). In these conditions, the kidneys are damaged and cannot fully perform their functions.
- Systemic diseases. Inflammatory processes localized in other organs and systems.
- Venereal and gynecological inflammatory diseases.
Leukocytes come in different groups: neutrophils, eosinophils, basophils, cells of the mononuclear phagocyte system (monocytes, tissue macrophages, dendritic cells) and lymphocytes. Each type is characteristic of different diseases. To determine the type of leukocyturia, additional urine testing will be required.
Menstruation, pregnancy and esterase
For the same reason, women are not recommended to undergo any urine test at all during menstruation, since at this time the urine may be abundantly “supplied” with red blood cells, and the phenomenon of hemoglobinuria will also appear, associated with the presence of hemoglobin from red blood cells in the urine. As for traces of leukocyte esterase in urine during pregnancy, this indicates the presence of microorganisms in the genital or urinary tract.
Pregnant women simply often do not know that leukocyte esterase and the presence of microbes can be equated. Therefore, a typical question on the forum may sound like this: “Girls, I’m finishing my sixth month of pregnancy, yesterday I took the test. It showed an increased amount of protein, salt, a lot of bacteria and also traces of some mysterious leukocyte esterase, which worries me very much, since the doctor is silent, and nothing has been written about this anywhere. How dangerous is leukocyte esterase in urine during pregnancy?
If we explain to this woman that esterase is a weapon of defense against bacteria, and it is simply a reflection of the activity of local immunity, then everything will fall into place.
So, in this little piece it was explained that this is leukocyte esterase in urine. In order not to give cause for concern and false positive results, you must carefully follow the rules for taking a urine test, which can be found on any website of a private or public laboratory, or simply take a note from your doctor.
It is known that leukocyte enzyme is not detected in the urine of a completely healthy person. In the same case, if there is a large number of leukocytes in it, then it simply does not make sense to conduct research, since “you should not suspect if you are quite sure.”

Currently, high-quality test strips have appeared that can detect the presence of protein, bile pigments, its pH, and identify the activity of this enzyme in one immersion in urine.
If you have leukocyte esterase in your urine, you must first rule out an infectious process. Damage to the renal glomeruli may also be the cause. If traces of esterase are detected without signs of inflammatory kidney damage, without microbes in the urine and with a negative result of bacteriological examination, then this condition is highly suspicious for a tumor of the urinary system, and a more thorough examination, including instrumental, is necessary.
Reduced leukocytes in urine
A healthy person has the lowest possible concentration of leukocytes in the urine.
Therefore, there is no such thing as low white blood cells in the urine. A low level of leukocytes in the urine is the norm. The situation is completely different with a blood test. A reduced level of white blood cells in the blood may indicate reduced bone marrow function, autoimmune disorders, congenital pathologies, and acute infectious processes.
Read more in the article about leukocytes in the blood.
Tests for leukocytes in urine
To determine the number of leukocytes in urine, two tests are most often used:
- General clinical urine test (code: 85-85-001). The simplest and most common, but no less informative urine test. During the study, the color, transparency and acidity level of urine are determined, as well as the number of the following indicators: red blood cells, white blood cells, protein, sugar, bilirubin, hemoglobin, ketone bodies, casts and epithelial tissue cells.
- Test according to Nechiporenko (counting of formed elements, code: 85-85-009). Prescribed based on the results of a general urinalysis if abnormalities in the test results were detected. Determines the number of red blood cells, leukocytes, casts and bacteria in the biomaterial. This is an additional test in the diagnosis of inflammatory diseases of the urinary tract.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
Benefits of Enzyme Research
Urologists and specialists in infectious pathology of the urinary tract like to prescribe this test as a screening test when monitoring the quality of treatment of pyelonephritis, urethritis, cystitis and other inflammatory lesions. After all, the presence of this enzyme indicates inflammation even in the case when there are no more leukocytes, and there are not even traces of their cells. This allows one to confidently, based on this indirect sign, suspect bacteriuria and an inflammatory infectious process, even if microscopy of the urine sediment did not show the presence of either leukocytes or microbial cells.
Of course, this result of the analysis should not be considered in isolation. Thus, traces of leukocyte esterase in urine must be taken into account together with the results of sediment microscopy, as well as with other reactions. Indirect markers of inflammatory lesions will be the presence of protein in the urine, its cloudiness, the presence of bacteria, and so on. Therefore, the reliability of microbial contamination of urine will be much higher if all these signs are simultaneously detected in the tests, and it will be possible to accurately make a diagnosis, including identifying the pathogen, based on the results of bacteriological culture. The only “minus” of sowing is that it can take several days, or even up to 2 weeks, for the growth of a pure colony and determination of the sensitivity of pathogens to antibiotics.