“The silent epidemic of the 21st century” is how osteoporosis is now figuratively called. More than 200 million people in the world suffer from this disease. Brittle bones, a hump-shaped curvature of the spine, and hip fractures in older people are manifestations of osteoporosis that can lead to disability and even death.
According to WHO statistics, osteoporosis ranks fourth in mortality, behind cardiovascular diseases, oncology and diabetes. In our country, osteoporosis is detected in every third woman over 50 years of age and in every fifth man.
1 Consultation with a rheumatologist

2 Diagnosis and treatment of osteoporosis

3 Consultation with a rheumatologist
So, what is osteoporosis? Translated from Greek, this means “porous bone” - thinning of bone tissue due to the loss of calcium salts, which leads to increased fragility and, as a consequence, frequent fractures and bone deformities. Already from the age of 35, bones gradually become thinner and less strong. This is typical for every person, but in some people the process is more intense and leads to earlier osteoporosis.
Osteoporosis affects the entire skeleton, but the bones most affected are the hips ( osteoporosis of the femoral neck ), forearms and vertebrae ( osteoporosis vertebrae ). Even a minor blow (for example, from a fall) can cause a fracture. Sometimes the load created by the body’s own weight is enough to cause a fracture - for example, fractures of the femoral neck and lumbar vertebrae can occur. Such fractures are called low-energy fractures. Sometimes “people” use names that are not entirely medically literate to indicate the location of osteoporosis, such as “osteoporosis of the shoulder joint,” “osteoporosis of the knee joint,” and “osteoporosis of the hip joint.” The joints as such are not affected by osteoporosis, but they can be involved in the pathological process when nearby bones affected by osteoporosis are fractured.
Etiology
Osteoporosis is characterized by a decrease in mineral density with concomitant changes in the quantity and microarchitecture of bone tissue, which is accompanied by impaired skeletal strength and an increased risk of fractures, especially of the spine, femoral neck and wrist. Bone mass depends on the interactions between the cells that form ( osteoblasts
) and break down (
osteoclasts
) bone.
Individual peak bone mass, which is normally achieved by 25-30 years, depends on genetic and non-hereditary factors: hormonal status, physical activity, nutrition. Hormonal imbalance, unbalanced diet, sedentary lifestyle, smoking, excessive alcohol consumption are risk factors for bone loss. Thus, osteoporosis is a heterogeneous disease, it can be classified as primary or secondary according to the causes responsible for bone loss .
Vertebroplasty
Among the methods of surgical treatment of uncomplicated fractures of the vertebral bodies in osteoporosis, it is necessary to highlight the technique of percutaneous vertebroplasty, developed and applied in France in 1984. Deramond EL, Depriester C, Galibert P., Le Gars V. This is a minimally invasive technology for the treatment of pain in the spine caused by various diseases affecting the vertebral body.
All manipulations are performed under X-ray control.
Indications for vertebroplasty are:
- compression fractures due to osteoporosis, both with pain and painless forms;
- tumor or metastatic lesions of the vertebral bodies;
- hemangioma of the vertebral body with its tendency to grow and cause pain;
- multiple myeloma.
The analgesic effect is associated with the elimination of micromobility of fragments, thermal and chemical effects during polymerization, causing dereception of nerve endings. Once hardened, the bone cement restores the supporting function of the vertebra. This allows you to avoid traumatic surgery or long-term wearing of an uncomfortable corset. Correction of deformity and strengthening of the vertebra occurs through direct injection of cement into the vertebral body through a special needle, usually under local anesthesia.
Contraindications to the procedure:
- Hemorrhagic diathesis;
- Infections;
- Damage to the posterior wall of the vertebra makes the procedure dangerous due to the risk of cement leakage into the spinal canal and compression of the spinal cord.
The manipulation is performed through a skin puncture. The patient can be discharged the very next day after surgery.
Diagnostics
The initial stage of diagnosing osteoporosis is identifying risk factors
based on patient data:
- low calcium content in the diet;
- vitamin D deficiency;
- gastrointestinal diseases (decreased calcium absorption);
- early menopause;
- long periods of immobilization
- long-term use of glucocorticoids, thyroid hormones;
- diseases of the thyroid gland, adrenal glands, kidneys, liver;
- low body mass index;
- bad habits (smoking, alcohol);
- low physical activity.
X-ray methods
are the most accessible and widely used in clinical practice when examining bones.
However, X-rays can detect the presence of osteopenia only when there is a loss of more than 30% of bone mass, so this method more often detects late signs of osteoporosis - vertebral deformities or fractures of long bones. Densitometry
is a measurement of bone tissue density based on the measurement of the mineral component of bone tissue - calcium.
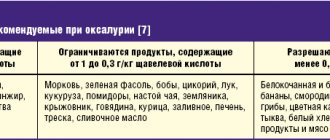
Currently, for the early diagnosis of osteoporosis, various methods of bone densitometry are used, which make it possible to detect as little as 2-5% loss of bone mass, to assess the dynamics of bone tissue density during the development of the disease or the effectiveness of treatment. Isotope methods (mono- and two-photon absorptiometry), X-ray (mono- and dual-energy absorptiometry, quantitative computed tomography) and ultrasound methods are used. Using monophoton, monoenergetic and ultrasound densitometry, peripheral parts of the skeleton are examined. These methods are most suitable for osteoporosis screening or preliminary diagnosis. The most versatile is the use of dual-energy X-ray absorptiometry (DEXA) - the gold standard, which allows you to measure the content of bone mineral in any part of the skeleton, as well as determine the content of calcium salts, fat and muscle mass throughout the body. Standard (automatic) programs for such densitometers are programs for the lumbar vertebrae, proximal femur, forearm bones and the “whole body” program. Regardless of whether osteoporosis is considered as a disease or a syndrome, the risk of fractures determined by densitometry cannot be the same for all bones of the skeleton. Therefore, the choice of its areas for study is extremely important. To make this choice, it is necessary to remember that there are two different layers in the bone tissue. The compact (cortical) substance makes the main contribution to bone strength, but is characterized by a low rate of metabolic processes. Spongy (trabecular) substance, on the contrary, is very active in terms of metabolism. It has been noted that different types of osteoporosis affect these two layers differently. With predominant damage to the trabecular substance, postmenopausal, hypogonadal, and steroid osteoporosis develops; cortical substance – senile, hyperthyroid, hyperparathyroid, diabetic osteoporosis. With many types of osteoporosis, there is a tendency for osteoporosis to gradually “spread” from the axial skeleton (primarily the vertebrae), where the first signs of osteoporosis appear, to the peripheral. Therefore, given the extreme value of early diagnosis of osteoporosis, examination of the axial skeleton should generally be preferred. The study of the peripheral parts (tibia, calcaneus, phalanges of the fingers) is often called screening.
The difference between spotty and diffuse
The main types of osteoporosis are spotty and uniform (diffuse). What they have in common is increased transparency of the bone pattern. In the spotted form, even lighter lesions appear on a light gray or normal background. They can be single or numerous, round, polygonal or oval. Their outline is not clear, and their size is 2-5 mm. The cortical zone does not change or acquires a loose (spongy) structure.

Diffuse osteoporosis has a uniformly transparent appearance without a spotty pattern. Bone substance consists of thin partitions (trabeculae) that do not block x-rays much. The bones are like glass with an accentuated shell (cortex).
These two types are often successive stages of osteoporosis - spotty early, and uniform later, but can also occur as independent variants of the disease.
Clinical laboratory tests
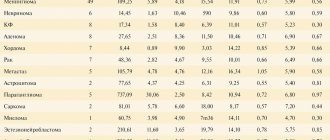
The pathogenesis of osteoporosis development is based on an imbalance in the processes of bone remodeling (bone formation) and bone resorption: either accelerated resorption predominates, or reduced bone formation, or a slowdown in both components of bone turnover. Normally, the amount of newly formed tissue is equivalent to that destroyed. The main goal of early biochemical diagnosis of osteoporosis is to assess the intensity of bone metabolism. For this purpose, special biochemical markers are used, which can be divided into three groups. The greatest importance in the differential diagnosis of skeletal diseases of a metabolic nature is the assessment of the hormonal status of patients, in particular parathyroid hormone (PTH), sex steroid and gonadotropic hormones, as well as vitamin D, which is involved with PTH in the regulation of calcium metabolism. Determination of the concentration of calcium, phosphorus and total activity of alkaline phosphatase in blood serum is used in assessing the general status of the patient and has an auxiliary, but not diagnostic value.
Bone formation markers
Osteocalcin
– the main non-collagenous protein of the bone matrix, which is synthesized by osteoblasts.
The synthesis of osteocalcin depends on vitamin K and D
, which to some extent reduces the sensitivity and specificity of determining osteocalcin as a marker of bone metabolism.
But, precisely, its concentration in the blood reflects the metabolic activity of osteoblasts of bone tissue, since osteocalcin in the blood is the result of new synthesis, and not its release during bone resorption. It is synthesized by osteoblasts into the extracellular space of the bone, some of it enters the bloodstream, where it can be analyzed. High levels of PTH suppress the production of protein by osteoblasts, resulting in a decrease in its concentration in bone tissue and in the blood. According to many authors, this indicator is a “possible” prognostic indicator of increasing bone disease. Calcitonin
is a polypeptide hormone secreted by C-cells of the thyroid gland.
The main effect of calcitonin is to reduce calcium levels in the blood and deposition in the bones. In its action it is an antagonist of parathyroid hormone. Calcitonin acts through specific receptors (in bones, kidneys), as a result of which bone resorption and the release of calcium from bone are inhibited. Bone enzyme alkaline phosphatase (b ALP)
Its study, along with the general activity of alkaline phosphatase (ALP), significantly increases the information content in the differential diagnosis of diseases of the skeleton and liver.
Alkaline phosphatase
is associated with osteoblast activity and therefore its determination complements the picture of bone tissue formation.
Read also
Humeroscapular periarthritis
Humeral-scapular periarthritis - (humeral-scapular periarthrosis, glenohumeral periatropathy) is the most common cause of shoulder pain.
The disease is associated with the pathology of soft tissues around the joints.… Read more
Cervicalgia
Many people experience neck pain, or cervicalgia. Everyone has experienced cervical pain at least once in their life, which is pain localized in the neck, not spreading to other areas...
More details
Thoracalgia
Thoracalgia is pain localized in the chest, the intensity of which varies from dull, aching to sharp, sharp pain. Sometimes the pain can radiate to the neck, lower jaw, back, one...
More details
Schmorl's hernia
When a person undergoes magnetic resonance imaging of the spine for the first time and sees the phrase “Schmorl’s hernia” in the conclusion, he is naturally overcome by a feeling of anxiety. After all, according to the patient, the terms...
More details
Rotational subluxation of the C1 vertebra
Dislocation or subluxation of a vertebra is a partial or complete disruption of the shape of the connecting articular surfaces of two adjacent vertebrae, and the overlying ones are considered dislocated. The reason for the rotational...
More details
Exchange status markers
Parathyroid hormone (PTH)
– is one of the main regulators of calcium-phosphorus metabolism, synthesized by the parathyroid glands in response to a decrease in extracellular calcium concentration.
It activates bone resorption and leads to the entry of calcium and phosphorus into the blood. Thyroid stimulating hormone (TSH), on the contrary, promotes the absorption of calcium and prevents its removal from bone tissue. Meanwhile, the level of calcium in the blood must be constant; if it is low, then the risk of developing cardiac pathology is high and the regulatory system of our body goes to great lengths to ensure that the calcium level in the blood is normal, “taking” it from the skeleton and muscles. Calcium and phosphorus
are the main mineral components of bone tissue. Different forms and stages of osteoporosis may exhibit different shifts in the concentrations of these minerals. Another aspect of the problem of impaired calcium homeostasis is vitamin D deficiency. It is well known that with age there is a progressive decrease in intestinal absorption of not only calcium, but also vitamin D, as well as the formation of vitamin D in the skin. In 2006, a panel of experts from the National Osteoporosis Foundation of America showed that treatment with calcium and vitamin D supplements is cost-effective and beneficial in preventing osteoporosis.
Markers of bone resorption
To assess the effectiveness of osteoporosis treatment, resorption markers are usually used, since their decrease under the influence of therapy begins after 2-3 weeks and reaches a plateau after 3-6 months (Research Institute of Transplantology and Artificial Organs of the Ministry of Health of the Russian Federation). Detection of normal or significantly increased levels of resorption markers with a single determination
already has diagnostic value.
Deoxypyridinoline (DPID).
Today, DPID is considered the most adequate marker of bone resorption.
Bone collagen is characterized by the presence of cross-links between individual collagen molecules, which play a large role in its stabilization and are presented in the form of deoxypyridinoline. The release of DPID into the vascular bed from the bone occurs as a result of its destruction by osteoclasts. DPID does not undergo further metabolic transformations and is excreted unchanged in the urine. Its excretion is increased in many types of osteoporosis. beta-CrossLaps
– (C-terminal telopeptides) formed during the degradation of type 1 collagen, which makes up more than 90% of the organic matrix of bone. Measuring beta-CrossLaps allows one to assess the rate of degradation of relatively “old” bone tissue. Normally, small fragments of collagen formed during its degradation enter the blood and are excreted by the kidneys in the urine. In patients with reduced renal function, the content of beta-CrossLaps in the blood serum increases due to decreased excretion. With a pathological increase in bone resorption (old age, osteoporosis), type 1 collagen degrades to a large extent, which leads to an increase in the level of collagen fragments in the blood. Currently, more and more data are emerging on the effect of gene polymorphisms on bone mineral density (BMD). A group of scientists from the State Institute of Rheumatology of the Russian Academy of Medical Sciences obtained data on the effect of polymorphism of the BMP4 gene on bone mineral density and markers of bone remodeling in groups of postmenopausal women with osteoporosis. A significant association was found between the polymorphism of this gene (6007C - T polymorphism of exon 4) with Lumbar BMD and bone remodeling markers. At the same time, the average level of alkaline phosphatase was reduced, and the CrossLaps level was high. These data indicate a lower intensity of bone formation processes and a higher intensity of bone resorption processes. The study of allelic polymorphism of the bone remodeling gene network is a promising direction for identifying genotypes of susceptibility to osteoporosis. Thus, determining the level of biochemical markers of bone resorption and remodeling allows:
- during a preventive examination, identify patients with metabolic disorders of the processes of bone tissue remodeling and resorption;
- assess and predict the level of bone loss;
- evaluate the effectiveness of the therapy within 2-3 months
Treatment
Carrying out functional treatment of vertebral fractures in elderly people due to osteoporosis is largely difficult due to the risk of developing hypodynamic complications; the use of fixing corsets and orthoses in such patients is significantly limited due to their intolerance and the risk of exacerbation of cardiopulmonary failure. Traditional surgical methods for treating vertebral fractures are associated with significant trauma and blood loss, which can be fatal for the body of an elderly person.
Prognostic significance
High levels of bone resorption markers, twice the normal level, are associated with a twofold increase in the risk of fractures; Patients with osteoporosis who have levels of bone resorption markers 3 times higher than normal have other metabolic bone pathologies (including malignancy). Thus, indications for studying markers of bone metabolism are:
- determining the risk of developing osteoporosis;
- monitoring during menopause and postmenopause;
- monitoring during hormone replacement therapy;
- assessment of the effectiveness of therapy with antiresorption drugs
Today, each of you can independently diagnose osteoporosis using a specially developed laboratory program “Bone Tissue Metabolism”. This diagnosis will help to identify metabolic abnormalities at a very early stage and promptly consult a doctor for prevention and treatment.
Common symptoms of osteoporosis
The development of osteoporosis in women after 50 years is associated with a decrease in the amount of estrogen produced.
Early symptoms of osteoporosis are very nonspecific, which is why they do not allow early suspicion of the development of this disease:
- painful sensations in the bones, especially when the weather changes;
- brittle bones;
- increased fatigue;
- painful contraction of the muscles of the legs at night.
The main manifestations of osteoporosis in later stages are associated with damage to the spine and other bones with a high proportion of spongy substance (femoral neck, ribs, lower part of the forearm bones, calcaneus).
Main symptoms of spinal osteoporosis
The main symptoms of spinal osteoporosis look like this:
- dull pain in the area of vertebral deformation (may have the character of attacks);
- changes in the shape of the spine (scoliosis, stooping, decreased height);
- appearance of a hump;
- pain and heaviness in the thoracic and lumbar regions (lumbar osteoporosis).

1 Radiography

2 Diagnosis of osteoporosis
3 General blood test