The documented procedure sets out the rules for collecting and transporting biological materials to the laboratory of clinical microbiology (bacteriology) of the Murmansk Regional Clinical Hospital named after. P. A. Bayandin” in order to improve the quality of laboratory test results and organize anti-epidemic and preventive measures, as well as the prevention of nosocomial infections among medical personnel and patients.
The documented procedure is intended for use in the ICH, and can also be used by organizations submitting an order for laboratory diagnostic services.
General provisions
The proposed technique for collecting and transporting biological materials into the LCM of the Moscow Regional Clinical Clinical Hospital will reduce the level of preanalytical error and improve the quality of the laboratory’s work in objectifying the results.
The documented procedure defines the rules for protecting medical personnel and patients from infection when collecting and delivering to the laboratory samples of biomaterials that may be contaminated with bacteria, fungi, viruses, and parasites.
General requirements for collecting biomaterial samples for microbiological research
Material for research is collected in sufficient quantities.
The material must correspond to the nature of the infectious process.
When collecting material, it is necessary to use only sterile instruments and utensils, observing the rules of asepsis to exclude contamination (contamination) of the biosample with normal microflora, because its presence leads to erroneous interpretation of the results.
When collecting biomaterial, medical staff are required to use personal protective equipment (hereinafter referred to as PPE) (gloves, mask, cap, goggles, etc.).
It is necessary to collect biomaterial only in recommended transport media and containers .
Material for research, if possible, is collected before the start of antibacterial therapy. If this is not possible, it is collected immediately before the repeated administration (taking) of drugs.
The research referral form must indicate the name of the antibacterial drugs being taken.
Contamination of the outer surface of the container during sample collection and delivery is not allowed.
Contamination of accompanying documents (directions) is not allowed.
When collecting biomaterial in test tubes, it is necessary to use racks.
After taking the biomaterial, you must make a note about the procedure on the referral form: date, time of collection, other information.
Rules for labeling biomaterial samples for microbiological research
All biosamples entering the laboratory must undergo a barcoding procedure.
Stickers with barcodes are obtained in the centralized multifunctional laboratory (hereinafter referred to as TsML) of the Moscow Regional Clinical Clinical Hospital.
The purpose of barcoding is to identify the patient (the test tube (container, bottle) and the form must have the same barcode number).
The barcode is pasted onto the test tube (container, bottle) strictly vertically with a digital inscription from top to bottom, on the existing sticker. It is necessary to leave a transparent zone to monitor the condition of the biosample. Barcodes that are placed unevenly will not be read by device scanners.
The barcode must be pasted evenly and tightly, strictly vertically (with the long side along the tube or container) (Figure 2).
When marking a container, the barcode is glued directly to the container itself; markings are not applied to the lid.
Double labeling is recommended - in addition to barcoding, a short note is applied to the collection container (number, surname, clarification of the location of the biomaterial, etc.).
The choice of tapes with barcodes is determined by the number of test tubes, containers for research of one patient, taking into account the barcoding of the referral form (at least 2 barcodes on the tape: 1st for the test tube, 2nd for the form).
All biomaterial is marked with double barcodes.
Research Exception:
(63037) “Microbiological examination of blood and other normally sterile liquids for microflora”
Triple barcode must be used:
1 – referral form for research
2 – aerobic bottle
3 – anaerobic bottle
General requirements for storage conditions of biomaterial samples before delivery to the laboratory
Observe the storage conditions for biospecimens before delivery to the laboratory (Table 1).
It is recommended to organize a place for storing biosamples in the departments of a medical organization before sending them to the laboratory (Table 2).
The storage area for biological samples must be marked with a “Biohazard” sign.
Biosamples must be stored in closed containers marked with the “Biohazard” sign.
Regularly carry out disinfection treatment of the storage area of biosamples and containers.
Accompanying documents (reference forms for research) are placed in a plastic bag (file) to prevent contact with the biomaterial.
Table 1
general characteristics
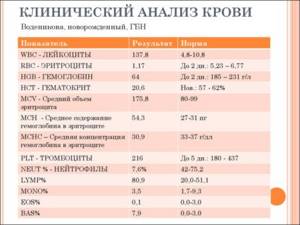
Blood cultures should be performed in all critically ill patients with fever, chills, or suspected endocarditis, intravascular infection, or immunosuppression. The cause of sepsis or bacteremia, especially in weakened patients, can be any microorganisms, including opportunistic and even saprophytic species. If the detection of pathogenic microorganisms in the blood almost always indicates their etiological significance, then the findings of opportunistic and saprophytic species may be a consequence of contamination of the blood during its collection or accidental contamination of crops during further work with them. Microorganisms that are released: Aerobes: streptococci, staphylococci, enterobacteria, non-fermenters, enterococci.
What does a blood test show for sterility?

Date: 02/15/2019
Not every patient knows why doctors in clinics write out referrals for various examinations, including blood tests for sterility. Doctors claim that this testing is prescribed to identify bacteremia in a patient, which indicates the presence of pathogenic processes in the body. To get a reliable result and the opportunity to begin competent treatment, the patient needs to know the rules for taking blood and strictly follow some recommendations for several days.
Characteristics of the study
Blood culture for sterility - what is it and why is it called that? This examination is one of the most important, as it gives doctors the opportunity to identify the presence of microorganisms in the blood, which indicate the development of various pathologies and internal inflammatory processes. In a healthy person, the blood and other body fluids should be sterile, and if the test shows the opposite result, this indicates the presence of some kind of disease. To determine a violation of sterility, hematological culture on various nutrient media is most often prescribed.
Indications for use
The main purpose of the analysis is to identify the presence of harmful microorganisms that provoke the inflammatory process. The diagnostician may prescribe the patient to donate blood for microbiological testing in the following cases
- if the patient suffers from specific symptoms, but doctors for a long time cannot determine what is the primary source of the pathological process;
- the physician assumes the presence of a septic infection in the patient;
- the presence of complications caused by improper surgical intervention;
- placing a catheter in internal organs for a long time;
- a person periodically suffers from high body temperature, but doctors cannot determine what causes such a reaction in the body;
- the presence in the body of an implant that is in direct contact with the biological media of the body.
The absolute indication for testing behavior is the presence of artificial myocardial valves. To obtain a reliable analysis result, you will have to wait at least 10 days, since the germination of pathogenic microorganisms will take several days.
Experts warn that the speed of this process depends on the type of pathogen. It is worth noting that after collecting biomaterial, many patients are prescribed antibiotics (based on the presenting symptoms), but choosing a more competent and optimal treatment regimen is possible only after receiving hemotest data.
What testing allows us to identify In most cases, bacterial culture for sterility is prescribed to detect harmful bacteria and microbes in the blood, such as:
Blood testing
- staphylococci;
- streptococci;
- yeast fungi;
- mold spores;
- enterobacteria.
This study is necessary for patients who have reduced body defenses, as well as for people suffering from dangerous pathologies such as HIV, tuberculosis, and acute infectious diseases. In addition, testing is often prescribed if doctors cannot decide on the optimal treatment regimen.
What diseases can culture help identify? Testing for the presence of pathogenic microorganisms allows us to determine the presence of the following pathologies:
Sepsis.
- Meningitis.
- Pyoderma.
- Endocarditis.
- Osteomyelitis.
To detect the type of blood culture, a thorough analysis of the suspected pathogen is required. If the study shows its presence in the body, doctors will need to find out how serious a danger the detected microbes pose to various systems and internal organs.
Where can testing be done? If a person needs to conduct such a test, it is better to make an appointment at a private diagnostic center. The main condition is the presence of a laboratory for microbiological research there. As practice shows, in such institutions the interpretation of the results is carried out in the shortest possible time. The cost of the procedure may vary depending on the type of clinic, but usually the price of testing varies between 400-700 rubles.
Features of preparation Since bacterial culture is a microbiological study, the reliability of the result can be affected by internal and external factors. To prevent obtaining a false result, the patient needs to perform certain preparations:
three days before the delivery of biological material, it is strictly forbidden to consume alcoholic beverages and medications (regardless of the pharmaceutical category);
- within 72 hours before the analysis, it is not recommended to eat fatty, overcooked foods and dishes with a lot of seasonings and spices;
- Smoking is prohibited 3 hours before blood collection.
If the patient ignores the rules, the likelihood of receiving an incorrect test result increases several times, which may lead to the need for secondary testing. There are contraindications. Consult your doctor. Sign up for PET-CT diagnostics!
Carrying out the procedure in adults The algorithm of actions is very simple, but the most important point is compliance with the sampling technique. The biomaterial must be taken strictly from the vein of the elbow. The physician must ensure that no external contaminants enter the bloodstream.
To prevent damage to the biomaterial, blood is drawn with a disposable sterile needle. Before proceeding, the area of the epidermis must be treated with an antiseptic solution. In most cases, about 10 ml of biomaterial is taken from the patient, after which it is placed in a bottle with a nutrient medium that prevents changes in the structure of the blood.
To reduce the risk of infection, blood is poured from a syringe into a vial placed above the burner flame. After these steps, the vial is sealed with a tight lid and placed in a special container until further research is carried out. In the rarest cases, the patient is injected with adrenaline before blood sampling, since the substance increases the accuracy of the analysis and helps to identify the maximum number of pathogens.
Analysis in children In a child, manipulations with blood are carried out differently. Biomaterial is removed only from the toe or heel. For bacterial culture, no more than 5 ml of blood is taken from children for sterility testing.
How long to wait for the result?
How long it takes to prepare an analysis is of interest to all patients. If the procedure was carried out in a modern diagnostic center, the first data can be obtained within a couple of days, but the form with the final results will be given to the patient no earlier than 10 days later. This is due to the fact that the blood will be subjected to various studies, and various reagents and substances will be added to the biomaterial.
Accuracy of the study
Doctors assure that this testing is guaranteed to provide the correct result and the ability to assess the general condition of the patient and identify the presence of certain pathologies. Inaccurate data can only appear if the patient ignored medical recommendations and preparation rules before donating the biomaterial. If all requirements are met, the probability that a person will receive reliable information about his condition reaches 95%.
What conclusions can be drawn after the analysis?
Today, sterility testing is indispensable, as it makes it possible to evaluate blood cultures and conduct research using various pathogenic organisms. In addition, during the study, you can find out how the body reacts to the consumption of certain drugs, thanks to which doctors will be able to choose the best treatment regimen. If a person periodically increases body temperature for no apparent reason, you should not hesitate to make an appointment with a specialist, who, after conducting a physiological examination and collecting an anamnesis, will issue a referral for further diagnostics. We cannot exclude the possibility that one of the first on the list will be a blood test for sterility, since based on this testing it is possible to draw conclusions about the general condition of the patient and prescribe a competent treatment regimen.
Author: : Alsherieva Kuralai Kurmanalievna
head of the bacteriological laboratory
Regional medical center. 02/15/2019
Indications for use
1. Conditions and infectious (bacterial origin) diseases, accompanied by repeated rises in temperature when the pathogen circulates in the blood. 2. Patients after surgical interventions, with pathology of the cardiovascular system, having vascular catheters, artificial heart valves and pacemakers.3. Bacteremia in infective endocarditis, osteomyelitis, arthritis, meningitis, pneumonia, intra-abdominal infections, infections of the skin, soft tissues and urinary tract.
Who needs to get tested?
Decreased immunity and fever may indicate the development of an infectious disease. Therefore, people who feel a sharp loss of energy, accompanied by constant temperature fluctuations, should undergo a sterility test.
Testing is necessary in some specific cases:
- the patient is feeling unwell;
- decreased immunity;
- suspected tuberculosis;
- suspected sepsis or meningitis;
- persistently high body temperature;
- ineffective antibiotic treatment;
- the patient is a blood donor.

Ineffective antibiotic treatment most often indicates that you are being treated for a misdiagnosis. In order not to injure the body with medications that will not help it in any way, it is necessary to donate blood for sterility. It's possible that you have more than one type of bacteria and the antibiotic only kills one of them. In this case, complex treatment is necessary.
If a person is a donor, then he must undergo this test so as not to infect the recipient. Infections that are transmitted through blood are very persistent, so the likelihood that they are transmitted through transfusion is very high.
Interpretation:
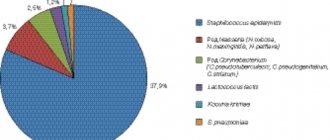
- 1. In case of accidental contamination of blood, microorganisms most often isolated are those that are part of the normal microflora of the skin or that are widespread in the environment: Staphylococcus epidermidis, Corynebacterium spp., Bacillus spp. and others. As a rule, they are the cause of sepsis only in patients with reduced resistance.2. The simultaneous isolation of several types of microorganisms from the blood most often indicates accidental blood contamination, but in patients with reduced resistance a mixed infection is possible.3. The etiological significance of the microorganism is indicated by its repeated isolation from the blood or simultaneous isolation from the blood and other types of test material; rapid detection of the microorganism within 48 hours. Approximately 65% of blood cultures from patients with bacteremia give a positive result in the first 24 hours of cultivation, and 90% within 3 days.
Sample result (PDF)
Recommendations for organizing the storage location of biospecimens before delivery to the laboratory
| Storage temperature, etc. | Biosample storage location |
| at room temperature (18-20°C), in a dark place | Closed “cold” cabinet, bedside table away from heating appliances |
| In a closed container for delivery | |
| at a temperature of 2-80C | In a refrigerator |
| In a thermal container with cold elements | |
| at a temperature of 370C | Thermostat |
| In a container with thermoelements heated to the required temperature (a heating pad, wrap in a disposable diaper, rags) |
General requirements for the delivery of biomaterial samples for microbiological research
Delivery of biomaterial samples is carried out on working days and LKM (bacteriology) time, according to the delivery mode to LKM.
The exception is the round-the-clock reception of the following biomaterials from the departments of the Moscow Clinical Clinical Hospital:
CSF samples - for latex agglutination reaction and bacteriological culture.
Blood samples - for culture for sterility.
The collected material is delivered to the laboratory within the recommended time frame (Table 1).
Delivery of biomaterial is carried out by courier.
Delivery of biomaterial by patients is not allowed.
To deliver biomaterial, it is necessary to use closed containers, bags or cooler bags, and must be marked with the “Biohazard” sign.
Delivery of biomaterial in hands, pockets, shopping bags and other personal items is not allowed.
The bottom of the containers should be covered with dry absorbent material (gauze, cloth, cotton wool, etc.).
Delivered containers with biomaterials must be closed with stoppers and lids to prevent the contents from spilling during transportation.
Delivery of liquid biomaterial is carried out strictly in a vertical position, in tripods.
Accompanying documents (reference forms for research) are placed in a waterproof bag (file, folder) to prevent contact with biomaterial.
The analysis of the delivered biomaterial must be carried out in compliance with safety precautions. Containers with biomaterials should be placed on a tray or tray. Personnel must use personal protective equipment (rubber gloves, mask).
Table 1
Decoding the results
A blood sterility level of less than 100% may indicate the presence of bacteremia. The more pathogenic bacteria are detected, the more extensive their activity throughout the body. Moreover, they are also found in biological materials such as urine and sputum.
The greatest accuracy is obtained by parallel cultivation of microorganisms in different substrates.
Tank culture can determine both the type of pathogen and the stage of infection in the body:
- The first stage of infection shows that there are no bacteria in the solid substrate, and a minimal amount is observed in the liquid substrate.
- The second is determined if a laboratory assistant identifies 5-8 colonies in a dense substrate.
- The third is due to the presence of bacteria in a dense substrate in a volume of up to 100 colonies.
- The corresponding indicator for setting the fourth stage will be the detection of colonies in quantities exceeding 100 pieces.
How to prepare for the analysis?
The procedure is carried out in a laboratory setting. Doctors, by culturing blood on a specific medium, can see whether you have bacteria in your body and how quickly they multiply. The types of bacteria are also determined. In order to donate blood for sterility, you need to follow only a few rules. First, don't drink alcohol or eat fatty foods. Secondly, don't smoke. These recommendations must be followed at least a few days before the procedure. You should stop smoking a few hours before taking a blood test.
Patients should also refrain from eating at least eight hours before the procedure. Blood is donated in the morning on an empty stomach, as this significantly increases the chances of the test results being reliable. The tests will be ready within about a week (for donors the verification period may be longer).
How long does it take for the result to be ready?
After about 3 days, the person being studied can learn that their blood is sterile. Within a few days, doctors can tell about the presence of bacteria and their approximate quantity.
The exact final result is ready in about 10 days. During this time, specialists “grow” infectious pathogens in special dishes. Also during this period, the resistance of bacteria and fungi to various antibiotics is studied.
Bacteriological culture process
During bacterial culture, the blood is placed on a nutrient culture, due to which the bacteria begin to actively multiply and “build” colonies.
The following substances can be used as nutrient media:
- casein or whey agar;
- egg medium;
- broth made from agar and animal blood.
The nutrient medium can be of two types:
- Liquid medium. Used for small numbers of bacteria. Test tubes are used as instruments.
- Dense environment. Used for large numbers of bacteria and fungi. A Petri dish is used as a tool. It is a carefully sterilized glass or plastic round flat bowl.
The material to be studied is placed into the nutrient medium using glass or metal needles, as well as special devices called a bacterial loop. To count the number of bacteria in the blood, the designation CFU is used - the number of units (microorganisms) in a milliliter of blood that are capable of forming a colony.
There are the following degrees of growth:
- First degree. In a dense structure, colonies are completely absent; a tiny amount of them is observed in a liquid medium.
- Second degree. In a dense environment, 5-8 colonies appear.
- Third degree. In a dense environment, up to 100 colonies can be counted.
- Fourth degree. There are more than 100 colonies of microorganisms in the environment.
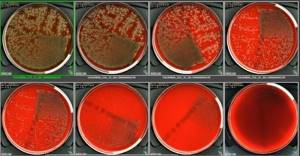
In the first and second degrees, a small amount of bacteria may indicate a violation of the blood sampling rules and insufficient sterility. A sign of contamination of material and equipment can also be a mixed result when colonies of different types of bacteria grow.
The advantage of bacterial culture is the possibility of conducting an antibiogram. This is a method for studying the resistance of bacteria to certain antibiotics.
The following methods can be used for this:
- Mixed disk method. Discs soaked in various antibiotics are placed in the environment with bacteria. The sensitivity of microorganisms to the drug can be judged by the zones of growth inhibition and reduction of the colony.
- E-test. The technique is the same as above, but instead of disks, pieces of paper with different concentrations of the same antibiotic are used.