General stool analysis
A general stool test is a common study that includes macroscopic, chemical and microscopic analysis. Macroscopic examination involves assessing the consistency, smell, and color of stool. Using a chemical test, you can determine the acidity, the presence of protein, bilirubin, and serotonin in a sample of biological material. If we are talking about a microscopic examination, doctors have the opportunity to detect in a sample undigested muscle fibers, plant fiber, elements of connective tissue, neutral fat, helminth eggs, protozoan cysts and much more, on the basis of which one can judge the presence of a number of serious diseases.
If a person follows a normal diet, the nature of stool depends on the following factors:
- Enzymatic breakdown of food at different stages of digestion;
- Absorption of food digestion products by the intestines - various vitamins and microelements;
- The current state of the intestines;
- The vital activity of bacteria living in the intestines.
General stool analysis transcript
The norm for fecal excretion in a healthy person is approximately 100-200g per day. Normal stool composition is 80% water and 20% dry matter. If a person is a vegetarian and eats foods exclusively of plant origin, the amount of feces can increase to 400-500g per day. If a person eats only easily digestible foods, the amount of feces excreted daily may decrease.
Consistency and texture
With normal indicators, stool has a moderately dense consistency. The discharge of mushy feces is also allowed if a person consumes mainly products of plant origin. The normal shape of stool is cylindrical. The smell should not be pungent. It can increase significantly if food products of animal origin predominate in the human diet. If a person is constipated or follows a dairy-plant diet, the smell of stool usually decreases. The normal color of stool is brown. Different variations of brown color are allowed: if you follow a vegetarian diet, the feces will be lighter. If a person eats animal products, the stool will be darker. If certain plant substances or medications enter the body, the stool may turn different colors - from burgundy to black. All of these are variations of the norm. There should be no mucous impurities in the stool, as well as bloody ones. There should be no pus or undigested food in the stool.
To interpret other indicators of the results of a general stool analysis, the help of specialists is necessary. A sample of biological material is studied for dozens of parameters. A person who is not knowledgeable in medicine will not be able to independently interpret the results.
| Age and type of feeding | ||||
| Analysis indicators | Breast-feeding | Artificial feeding | Older children | Adults |
| 40-50 g/day. | 30-40 g/day. | 100-250 g/day. | 100-250 g/day. |
| sticky, viscous (mushy) | putty-like consistency | Decorated | Decorated |
| yellow, golden yellow, yellow green | yellow-brown | brown | brown |
| sourish | putrefactive | Fecal, not sharp | Fecal, not sharp |
| 4,8-5,8 | 6,8-7,5 | 7,0-7,5 | 7,0-7,5 |
| absent | absent | absent | |
| absent | absent | absent | absent |
| absent | absent | absent | absent |
| present | present | 75-350 mg/day. | 75-350 mg/day. |
| present | present | absent | absent |
| 20-40 mmol/kg | 20-40 mmol/kg | ||
| Various quantity | Various quantity | Various quantity | Various quantity |
| Small quantity or none | Small quantity or none | absent | absent |
| absent | absent | absent | absent |
| absent | absent | absent | absent |
| absent | absent | absent | absent |
| Drops | A small amount of | absent | absent |
| Crystals in small quantities | Crystals in small quantities | absent | absent |
| In small quantities | In small quantities | Minor amount | Minor amount |
| single | single | Single in the preparation | Single in the preparation |
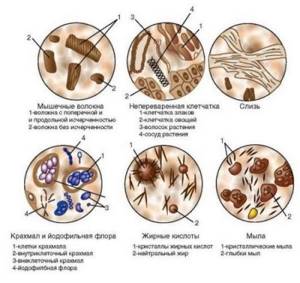
Microscopic examination
Muscle fibers - with striations (unchanged, undigested) and without striations (changed, digested). A large number of changed and unchanged muscle fibers in the feces (creatorrhoea) indicates a violation of proteolysis (protein digestion):
- in conditions accompanied by achlorhydria (lack of free HCl in gastric juice) and achylia (complete absence of secretion of HCl, pepsin and other components of gastric juice): atrophic pangastritis, a condition after gastric resection;
- with accelerated evacuation of food chyme from the intestines;
- in case of violation of the exocrine function of the pancreas;
- with putrefactive dyspepsia.
Connective tissue (remnants of undigested vessels, ligaments, fascia, cartilage). The presence of connective tissue in the feces indicates a deficiency of proteolytic enzymes of the stomach and is observed with hypo- and achlorhydria, achylia.
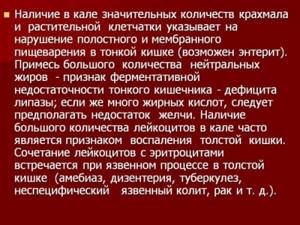
Fat is neutral. Fatty acid. Salts of fatty acids (soaps)
The appearance of large amounts of neutral fat, fatty acids and soaps in the stool is called steatorrhea. This happens:
- with exocrine pancreatic insufficiency, a mechanical obstruction to the outflow of pancreatic juice, when steatorrhea is represented by neutral fat;
- if the flow of bile into the duodenum is impaired and if the absorption of fatty acids in the small intestine is impaired, fatty acids or salts of fatty acids (soaps) are found in the feces.
Plant fiber
Digestible - found in the pulp of vegetables, fruits, legumes and grains. Indigestible fiber (the skin of fruits and vegetables, plant hairs, the epidermis of cereals) has no diagnostic value, since there are no enzymes in the human digestive system that break it down. It is found in large quantities during rapid evacuation of food from the stomach, achlorhydria, achylia, and the syndrome of bacterial overgrowth in the colon.
Starch
The presence of a large amount of starch in the feces is called amilorrhea and is observed more often with increased intestinal motility, fermentative dyspepsia, and less often with exocrine insufficiency of pancreatic digestion.
Iodophilic microflora (clostridia)
With a large amount of carbohydrates, clostridia multiply intensively. A large number of clostridia is regarded as fermentative dysbiosis.
Epithelium
A large amount of columnar epithelium in the feces is observed in acute and chronic colitis of various etiologies.
Leukocytes
A large number of leukocytes (usually neutrophils) are observed in acute and chronic enteritis and colitis of various etiologies, ulcerative necrotic lesions of the intestinal mucosa, intestinal tuberculosis, and dysentery.
Red blood cells
The appearance of slightly changed red blood cells in the stool indicates the presence of bleeding from the colon, mainly from its distal parts (ulceration of the mucous membrane, disintegrating tumor of the rectum and sigmoid colon, anal fissures, hemorrhoids). A large number of red blood cells in combination with leukocytes and columnar epithelium is characteristic of ulcerative colitis, Crohn's disease with damage to the colon, polyposis and malignant neoplasms of the colon.
Worm eggs
Eggs of roundworms, tapeworms, etc. indicate a corresponding helminthic infestation.
Pathogenic protozoa
Cysts of dysenteric amoeba, Giardia, etc. indicate a corresponding invasion by protozoa.
Yeast cells
Found in feces during treatment with antibiotics and corticosteroids. Identification of the fungus Candida albicans is carried out by culturing on special media (Sabouraud's medium, Microstix Candida) and indicates a fungal infection of the intestine.
Calcium oxalate (oxalic lime crystals)
Detection of crystals is a sign of achlorhydria.
Triple phosphate crystals (ammonium phosphate-magnesia)
Triple phosphate crystals found in feces (pH 8.5-10.0) immediately after defecation indicate increased protein putrefaction in the colon.
Tests for coronavirus
- Test for coronavirus
- Coronavirus test for organizations
- Testing for coronavirus at home
- Testing for coronavirus at home in 12 hours!
- Testing for coronavirus in Lyubertsy in 12 hours!
- Testing for coronavirus in Nekrasovka in 12 hours!
- Testing for coronavirus in Korolev in 12 hours!
- Test for coronavirus on the Sokol metro station
- Coronavirus test at Kolomenskaya metro station
- Coronavirus test at Voykovskaya metro station
- Test for coronavirus in Nekrasovka
- Coronavirus test in Korolev
- Test for coronavirus in Lyubertsy
- Test for coronavirus in Mytishchi
- Test for coronavirus at home Mytishchi
- Test for coronavirus at home Korolev
- Test for coronavirus at home Lyubertsy
- Test for coronavirus at home Nekrasovka
Any tests can be taken at clinics in the East Clinic network.
Extracellular and intracellular starch - what is the difference?
Starch grains in the coprogram can be in two versions:
Medical products (drugs, medicines, vitamins, dietary supplements) are mentioned for informational purposes only. We strongly do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
- Intracellular starch. Enclosed inside a cell under a membrane. Normally, thin cell membranes are completely broken down and absorbed in the intestines. The appearance of intracellular starch indicates excessive production of gastric juice or increased fermentation processes in the intestines. These conditions prevent cells from breaking down and releasing starch.
- Extracellular starch. It represents undigested membrane elements from destroyed cells. Normally, extracellular starch must be broken down by amylase, a pancreatic enzyme. Its appearance indicates secretory failure of the organ. This symptom also occurs during the rapid passage of food through the intestines, when the enzyme simply does not have time to start working.

Complications and consequences
Complications develop only if treatment is not started in a timely manner. There is a disruption in the absorption of nutrients in the intestinal tract. Against this background, hypo- and avitaminosis, protein deficiency and exhaustion of the body develop. Pathology of water and electrolyte balance is manifested by a constant feeling of thirst, edema, dehydration, and convulsive attacks.

The specialist diagnoses the appearance of oxaluria (excessive pathological excretion of oxalic acid salts from the body along with urine) and the formation of urinary stones of oxalate origin. This pathological condition occurs because, under normal conditions, oxalates do not enter the blood from the intestinal tract, since their combination with calcium makes them insoluble. With the development of steatorrhea, calcium is excreted in large quantities from the body along with feces. This leads to a significant release of oxalates from the intestines into the blood.
How to accurately determine the cause of the disease
At the first visit, the doctor palpates the abdomen. When you press on it in the lower left part, you can hear a rumbling sound, the sound of iridescent liquid. After the examination, the following types of diagnostics are prescribed:
- Rectoscopy
is an examination of the rectum with an endoscope (up to 30 cm). Allows you to identify swelling, atrophy, ulceration of the intestinal mucosa. - Colonoscopy
is a complete examination of the intestines. Allows you to identify pathologies in all areas. - Biopsy
is the removal of affected organ cells for examination. Allows you to confirm or exclude cancer. - Coprogram
(stool microscopy) allows you to identify drops of fat and fatty acids in the stool and determine at what stage the disease is. - Ultrasound of the digestive organs.
Identifies pathologies of internal organs. - MRI
is used if ultrasound examination turns out to be uninformative. Allows you to identify any pathologies and neoplasms. - A blood test
shows an increase in leukocytes and ESR. This is typical for this disease.
The doctor determines what type of diagnosis to prescribe depending on the suspicion of a particular pathology.

Is it possible to recognize steatorrhea on your own?
The clinical symptoms of the pathology are quite specific, so you can suspect an increased content of neutral fat in the feces on your own. The main signs are associated with a change in the consistency of feces - they become sticky, oily, shiny, and can stain underwear. Such feces are difficult to wash off from the surface, sometimes light yellow spots remain on the laundry after washing. The color of the stool may remain the same, but in most cases the stool will lighten and become greyish. There is no strong odor with steatorrhea - on the contrary, such feces usually smell weakly or not at all.
Severe dyspeptic symptoms with steatorrhea are usually absent, but sometimes patients complain of bloating, a feeling of heaviness and fullness in the abdomen, dry mucous membranes of the oral cavity, and appetite disorders. If it lasts for a long time, the child may experience other signs not related to the functioning of the digestive tract. It can be:
- frequent headaches that turn into dizziness (in school-age children this is manifested by a decrease in academic performance and difficulties in mastering the material);
- joint pain (mainly in the back and lower back);
- bleeding gums;
- weakness and drowsiness.

In children of the first year of life, steatorrhea is manifested by increased excitability, frequent bowel movements, refusal of the breast or bottle, and poor weight gain. Feces are oily, difficult to remove from diapers and nappies, and have a stronger odor compared to children of the older age group.
One of the manifestations of pancreatic or hepatic steatorrhea may be a cough, which externally manifests itself as infrequent coughing. The cough is usually dry, not painful, goes away easily after drinking liquid, but can last up to 2-3 months. If a child suddenly begins to cough, but there is no wheezing in the lungs, and overall health remains satisfactory, a stool test should be taken for a coprogram to check the functioning of the digestive system.
Treatment
Treatment will depend on the identified pathology, its severity and rate of development. If no organic disorders are detected, amilorrhea is considered functional. In this situation, only diet and regular monitoring by a gastroenterologist are indicated. For pathological amylorhea, medications are added to therapy.
Diet
The basis of nutrition for pathologies of the pancreas and small intestine is the rejection of spicy, fried and too fatty foods. It is recommended to steam, boil or bake all dishes in the oven. Reducing the usual volume of portions, frequent and split meals will be beneficial. Often, following a diet allows you to get rid of the problem and avoid drug therapy.
| Recommended Products | Not recommended products |
|
|
Diet should not be a one-time event, but a habit for life. This is the only way to avoid exacerbation of chronic pathology and prevent the progression of the disease.
Medications
- Enzymes that facilitate the digestion of food and replace pancreatic amylase.
- Drugs that reduce gastric acidity - antacids.
- Drugs that slow down intestinal motility.
- Antidiarrheal drugs.
- Sorbents (for diarrhea caused by intestinal infection).
After the exacerbation subsides, the following are prescribed:
- Vitamins to improve immunity and maintain overall body tone.
- Probiotics to restore normal intestinal flora and prevent dysbiosis.
The treatment regimen is determined by the gastroenterologist taking into account the identified pathology.