Amilorrhea is the appearance of undigested starch grains in the stool. Normally, it occurs in adults when switching to a vegetarian diet. In other situations, the development of amilorrhea indicates a disruption of the small intestine and incomplete absorption of nutrients. A similar phenomenon occurs in pathology of the pancreas, enteritis, functional insufficiency of the stomach and some other conditions.
Types of starch in feces
Amilorrhea is the appearance of starch inclusions in solid excrement. A healthy person should not have such impurities, unless we are talking about vegetarianism or eating a large amount of plant foods. The same reasons for this disorder may be typical for children.
Starch grains that appear in feces are of 2 types:
- Extracellular starch. These are undigested membrane elements that remain from incompletely resolved cells. In a healthy person, amylase is responsible for the breakdown of starch. This enzyme is produced by pancreatic cells. If extracellular starch appears in the feces, then this, first of all, will be evidence of a disruption in the functioning of the pancreas. This deviation is typical for the rapid movement of food without its complete digestion.
- Intracellular starch in feces. It is an element enclosed in a cell membrane. Normally, the membranes should be completely broken down and well absorbed in the intestines. But if this does not happen, this may be a sign of hypersecretion of gastric juice or increased fermentation processes in the intestines.
Extracellular and intracellular starch in feces is considered abnormal by default. However, it is important to understand what causes such elements to appear. Without clarifying them, nothing can be done about the deviation, and all measures taken will give only short-term results.
This is interesting: Symptoms of viral gastroenteritis - what it is and how to treat it
Detailed description of the study
Stool consists of 75% water and 25% solids. About 30% of the solid matter is bacteria, 30% is undigested food such as fiber, 10 to 20% is cholesterol and other fats, 10 to 20% is inorganic matter such as calcium and iron, and another 2 to 3 % - protein.
A coprogram is a laboratory analysis of a stool sample, which includes microscopic examination, chemical indicators and microbiological analysis. During the research process, many indicators are assessed, from color to chemical composition.
The consistency of stool is related to its water content. With diarrhea, its percentage increases, and the stool becomes liquid, that is, unformed. Constipation is associated with a decrease in water content in feces, which leads to compaction. A formed stool is considered normal.
The color of stool depends on the amount of bile pigments in it. Normal variants can vary from brown to yellow. Discoloration of stool may indicate the development of jaundice, a pathological condition in which the pigment bilirubin does not enter the fecal mass. Black stool is often associated with taking medications, such as bismuth, but is sometimes a sign of bleeding from the stomach.
The smell of feces reflects the activity of intestinal microorganisms. The appearance of a sour or fetid odor reflects an imbalance between normal and opportunistic intestinal microflora.
reaction is assessed relative to the pH of the environment and also indirectly reflects the vital activity of the intestinal microflora and its changes. A neutral or slightly alkaline reaction is considered normal.
Blood in the stool may be found due to bleeding primarily in the gastrointestinal tract.
Mucus is normally found in small quantities in the coprogram. It is secreted by cells of the colon and rectum to protect the mucous membrane of the organ. With pathological processes in the intestines, the formation of mucus increases.
Remains of undigested food are found in the coprogram when the secretion of digestive juices is insufficient, but they can also be detected during accelerated elimination of food from the body.
Altered muscle fibers serve as a product of meat digestion and are detected when there is insufficiency of digestive juices.
Unchanged muscle fibers indicate a violation of the breakdown of protein foods.
Plant fiber is divided into digestible and indigestible. The detection of digestible fiber reflects the insufficiency of the processes of utilization of complex carbohydrates.
Neutral fat and soap can be detected in coprogram, when bile and pancreatic juice are secreted in insufficient quantities to break down fatty foods. This can be observed in various acute and chronic diseases of the liver, gall bladder, and pancreas.
Fatty acids are a product of fat metabolism in the body. Their detection indicates a decrease in the absorption capacity of the intestine or an increase in its peristalsis, due to which these metabolic products cannot enter the bloodstream and accumulate in the intestinal lumen.
Starch is found inside plant cells (intracellular) or outside cells when they are destroyed (extracellular); normally, this type of carbohydrate is broken down by digestive juices. Starch can be detected in a coprogram when there is insufficient secretion of hydrochloric acid in the stomach and pancreatic juice.
Leukocytes are cells of the immune system that are detected in any organ during inflammation. Finding an increased number of white blood cells in a stool sample indicates inflammation in the gastrointestinal tract.
Red blood cells appear in the coprogram due to bleeding from the intestines.
epithelium tends to renew itself, and dead cells end up in feces. Inflammatory diseases lead to increased desquamation, which is reflected in the coprogram.
The detection of crystals reflects indigestion and specific inflammation in the gastrointestinal tract. Tripelphosphates are formed with a significant change in pH towards the alkaline side and are associated with the proliferation of opportunistic intestinal microflora. Charcot-Leyden crystals serve as a collection of eosinophils, cells associated with allergic reactions.
Iodophilic flora has this name due to its staining with iodine during research. An excess of representatives of this flora is a reflection of intestinal dysbiosis.
Yeast-like fungi are usually considered as opportunistic representatives of the intestinal microflora. Their detection in large numbers may also be a sign of dysbiosis.
helminth eggs in a coprogram serves as an important source for diagnosing parasitic infections. Microscopy allows you to determine not only the presence of eggs, but also the type of helminth. Determining these indicators when examining stool allows you to assess the condition of the digestive system and identify its diseases.
Method for detecting starchy compounds in feces in adults
Stool analysis to detect undigested starch is a coprogram. Here the entire digestive function is assessed. The coprogram includes the following indicators:
- consistency and color of stool;
- undigested food particles;
- fat;
- number of starch grains;
- muscle fibers;
- bacteria, protozoa, helminth eggs.
Using a coprogram, you can detect many pathologies that occur with damage to the gastrointestinal tract.
The presence of starchy compounds can be determined by the appearance of stool. They become abundant and soft. The color is yellowish-gray, the surface is shiny. The stool looks greasy and sticks to the walls of the toilet. A sharp unpleasant odor appears.
Extracellular starch in feces: the main causes of pathology
Pregnancy, children > Pregnancy > Examinations > Tests > Extracellular starch in feces: the main causes of pathology
Often, when conducting a coprogram (stool analysis), a specialist detects starch content. Under normal conditions, this substance should be absent from the material.
What does its appearance indicate and what causes the pathology?
What methods are used for treatment?
Stool analysis: main indicators
The study of feces and determination of its chemical composition and physical properties is called a coprogram.
This analysis is prescribed to diagnose pathological conditions of the digestive system.
The main indicators included in the study include:
- Form
- Color
- Smell
- Consistency
- Presence of mucus or blood
- Fecal reaction
- Unchanged and modified muscle fibers
- Leftover undigested food
- Red blood cells
- Digestible fiber (vegetable)
They also look at the absence or presence in the biological material of extracellular and intracellular starch, leukocytes, proteins, bilirubin, yeast-like fungi, crystals, fatty acids, detritus, clostridia, iodophilic flora, neutral fat.
Regarding starch in feces, two types of complex carbohydrate can be found in biological material:
- Extracellular
- Intracellular
Reasons for the appearance of extracellular starch in feces
This substance is undigested starch grains from cells that have collapsed.
A normal indicator is considered if there is no extracellular starch in the biomaterial. This is explained by the fact that the substance is properly broken down by enzymes of the gastrointestinal tract.
Stool analysis reveals pathologies of the digestive system
In medical terminology, an increase in starch in feces is called amilorrhea. It occurs due to dysfunction of the gastrointestinal tract.
The main reasons for the development of this condition are:
- Deficiency of amylase, a digestive enzyme, in saliva
- Decreased secretion of gastric juice
- Decreased activity of amylase, which is produced by the pancreas
Possible reasons for the appearance of starch in feces include the following pathologies:
- Enteritis is an inflammatory process in the intestinal walls, as a result of which food masses move faster through the digestive tract
- Gastritis and other diseases associated with dysfunction of the stomach
- Fermentative dyspepsia
- Intestinal dysbiosis affecting the absorption of starch
- Inflammation or atrophy of the pancreas, such as pancreatitis
Read: Why donate blood for hormones during pregnancy?
Among the common causes of amilorrhea are increased motility of the small intestine, as well as its diseases.
In infants, starch is usually also found in the feces, but this phenomenon is not considered a pathological condition and is associated with the immature functioning of the secretory glands.
Factors that influence this condition are:
- Excessive consumption of foods that contain starch (potatoes, bananas, pears)
- Use of medicinal products containing this component before testing
- Poor nutrition
- Excessive drinking and smoking
- Living in an area of unfavorable environmental situation
Only an experienced specialist can detect the main reason for the appearance of extracellular starch in stool. Depending on it, he will establish the correct treatment tactics.
Basic methods of treating the pathological condition
Therapy for the pathological condition is primarily aimed at eliminating the main cause of the appearance of extracellular starch in the stool.
The presence of starch in the feces of newborns is not a pathology
An important method for promoting effective treatment is following a diet, as well as limiting the consumption of vegetables and fruits containing this substance.
To treat pathologies in which starch is observed in the stool, the following medications are usually prescribed for complex treatment:
- Probiotics and mild laxatives that help normalize the functioning of the digestive system: Florin Forte, Duphalac, Bifidumbacterin, Normaze, Portalek, Probifor, Linex, Lactovit, Hilak Forte
- Enzyme complexes: Pancreatin, Panzinorm, Festal, Mezim
- Preparations for the treatment of diseases of the intestines and stomach.
These medications are prescribed by a specialist depending on the diagnosis.
In children under one year of age, the presence of starch in feces does not require treatment, as it is explained by the physiological characteristics of the baby.
It should be emphasized that it is especially important during treatment to adhere to the rules of a nutritious and balanced diet.
A stool test is included in a routine medical examination. It allows you to detect many pathologies occurring in the human body, so it is important not to ignore this diagnosis.
Read: Mushrooms in urine: what is the danger of ordinary thrush?
A specialist will tell you more about the analysis in the video:
Noticed a mistake? Select it and press Ctrl+Enter to let us know.
17 Sep 2021 Yuki 419
Decoding the result of fecal starch analysis
In young children who receive a lot of carbohydrate foods, a small content of starch in the stool is acceptable. In adults it should normally be absent. If starchy grains are found in the stool, this indicates a digestive disorder in the small intestine.
There are two types of starch grains in feces.
- Intracellular - found inside cells of plant origin that are not destroyed by gastric juice. The detection of such grains indicates a disruption in the functioning of the stomach, changes in the intestinal microflora and putrefactive processes in the gastrointestinal tract.
- Extracellular grains are lumps of starch that have not been treated with amylase. This is observed in pancreatitis, exocrine pancreatic insufficiency, as well as intestinal diseases with increased peristalsis.
Treatment for these pathologies of the digestive organs is different, so the analysis should only be carried out by an experienced specialist who knows the differences between extracellular and intracellular starch grains.
Possible consequences and prognosis for life
The appearance of starch in feces is not a disease, but only a symptom of it. It is important not only to remove negative phenomena, but also to eliminate their cause. Without treatment, disturbances in the functioning of the stomach, intestines and pancreas can lead to the following conditions:
- progressive weight loss;
- Iron-deficiency anemia;
- avitaminosis.
Be sure to read:
Bristol stool scale: description and interpretation
All these conditions are associated with insufficient digestion of food and lead to disruption of the functioning of internal organs.
Amilorrhea caused by pathology of the pancreas requires special attention. This organ is very sensitive to negative influences and easily fails. The most dangerous complication is pancreatic necrosis. Complete cessation of pancreatic function can be fatal.
The prognosis for amilorrhea depends on its cause and the severity of the pathology. The sooner the source of the problem is found and treatment is carried out, the higher the chances of a favorable outcome.
In continuation of the topic, be sure to read:
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- Diseases of the small intestine: symptoms and signs of the disease, treatment
- Causes of bloating and increased gas formation, treatment methods
- List of enzymes to improve digestion and their intake
- Steatorrhea: types, causes, symptoms and treatment
- Intestinal inflammation: signs of pathology, use of diet and drugs for treatment
- Extracellular and intracellular starch in a child’s feces: causes and treatment
- Undigested food in the feces (lientorrhea) in an adult: causes and diagnosis of pathologies
- Causes of white, dark lumps in stool and treatment methods (diet, medications)
- Why does blood appear in the stool of an adult: types, causes and what to do?
Extracellular and intracellular starch - what is the difference?
Starch grains in the coprogram can be in two versions:
- Intracellular starch. Enclosed inside a cell under a membrane. Normally, thin cell membranes are completely broken down and absorbed in the intestines. The appearance of intracellular starch indicates excessive production of gastric juice or increased fermentation processes in the intestines. These conditions prevent cells from breaking down and releasing starch.
- Extracellular starch. It represents undigested membrane elements from destroyed cells. Normally, extracellular starch must be broken down by amylase, a pancreatic enzyme. Its appearance indicates secretory failure of the organ. This symptom also occurs during the rapid passage of food through the intestines, when the enzyme simply does not have time to start working.

Diagnostics
During an external examination, the gastroenterologist draws attention to the lack of body weight of the patient with amilorrhea. Dryness and flaking of the skin, brittle nails, and jams are often detected, which indicates vitamin deficiency. The frequency and nature of stools, dietary habits, against which the symptoms appeared, are determined. To determine the causes of amilorrhea, laboratory and instrumental methods are used:
- Stool tests.
The coprogram contains an increased content of starch grains, neutral fats and undigested muscle fibers. To clarify pancreatic functions, the level of fecal elastase is measured. If there is a possible intestinal infection as the cause of amilorrhea, stool culture is indicated. - Functional tests.
To evaluate enzymatic activity, probe and probeless methods are performed. The pathology of the organ, manifested by amylorhea, is evidenced by an insufficient increase in the volume of secretions and the level of bicarbonates after drug stimulation. As a screening method, a blood test for amylase and lipase is performed. - Instrumental visualization.
To study the structure, contours and echogenicity of the organ, an ultrasound scan of the pancreas is performed. For a more detailed study of the parenchyma, a patient with amilorrhea needs an MRI. To exclude malignant neoplasms, selective angiography is informative. The condition of the pancreatic ducts is examined using ERCP. - Fibrogastroduodenoscopy.
The technique is recommended for suspected hyperacid gastritis, which provokes amilorrhea. With EGDS, specific inflammatory changes in the gastric wall, erosions are noticeable, and sometimes ulcerative defects are found. To change the level of hydrochloric acid secretion, intragastric pH-metry is performed. - Biopsy.
An invasive study with sampling of pancreatic tissue is necessary to assess the degree of fibrosis and destruction of the parenchyma, and to identify damage to the insular apparatus in patients suffering from amylorhea. The biopsy technique is very important for understanding the prognosis of the disease and choosing treatment tactics.
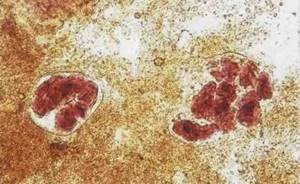
Starch grains in coprogram
Interpretation of results
The coprogram includes a list of indicators, the norms of which are given in the table.
| Coprogram indicator | Normative value |
| Form | Decorated |
| Consistency | Soft |
| Color | Brown |
| Smell | Fecal unsharp |
| Reaction | Neutral |
| Connective tissue | Not detected |
| Muscle fibers are indigestible | Not detected |
| Digestible muscle fibers | None |
| Striation of muscle fibers | Without striations |
| Neutral fat | Not detected In children under 1 month - in small quantities |
| Fatty acid | Not detected |
| Soap | Not detected |
| Indigestible fiber | In small or moderate quantities |
| Digestible fiber | Not detected |
| Extracellular starch grains | Not detected |
| Starch grains are intracellular | Not detected |
| Iodophilic bacteria | Not detected |
| Slime | Not detected |
| Leukocytes | Not detected or 0-2 in visual field. |
| Red blood cells | Not detected |
| Epithelium | Not detected |
| Protozoa | Not detected |
| Yeast fungus | Not detected |
| Helminth eggs | Not detected |
This is interesting: The whole truth about anal fissure surgery: when is it needed, and can there be complications?
What are the symptoms of amilorrhea, and is treatment necessary?
If intracellular starch appears in the feces of a child or adult, then such a deviation cannot occur latently. There are definitely some symptoms indicating disturbances in the gastrointestinal tract. An adult can notice them on his own, but as for children, parental vigilance is important.

Amilorrhea in children and adults is accompanied by the same clinical signs, namely:
- diarrhea;
- bloating;
- flatulence;
- gastralgia;
- rumbling in the stomach;
- pain around the navel;
- nausea;
- loss of body weight;
- sometimes vomiting.
Also, with amilorrhea, large volumes of feces are discharged. At the same time, it has an unpleasant odor and contains particles of undigested food.
Diagnostic features
The only way to help identify amilorrhea is a coprogram - a stool examination. It is prescribed for any ailments associated with disorders of the gastrointestinal tract. But to understand what extracellular starch in the coprogram means and says, an extensive examination is necessary. It involves carrying out:
- general and biochemical blood test;
- urine tests;
- ultrasound diagnostics of the abdominal organs;
- X-rays of the digestive tract;
- endoscopic examination of the intestine.
Thanks to a comprehensive examination, the doctor can make an accurate diagnosis. Amilorrhea is not an independent disease - it is only a symptom. Therefore, it cannot be treated in isolation.
It is for this purpose that a detailed examination of a patient with amilorrhea is prescribed. The sooner the cause of the deviation is clarified, the lower the risk of developing complications of existing pathologies.
How to treat?
In the treatment of amilorrhea, an important role is played by following a diet that completely excludes starchy foods from the diet, as well as any food that is harmful and difficult for the stomach. Patients are prescribed the following medications:
- Enzymes. Creon, Pancreatin, Pancreazym - all these drugs belong to this group. They help improve the production of pancreatic enzymes and facilitate the digestion process.
- Antacids. Medicines in this group reduce gastric acidity.
- Sorbents – activated or white carbon, Polysorb.
All medications are prescribed exclusively by a gastroenterologist. If necessary, the treatment regimen can be changed - it all depends on the achieved therapeutic effect. Self-medication for amilorrhea associated with gastrointestinal diseases is not only unacceptable, but also extremely dangerous. And the use of folk remedies does not have any reasonable grounds.
Causes of amilorrhea
Irritable bowel syndrome
The appearance of a symptom is possible with IBS with a predominance of diarrhea. Amilorrhea is caused by increased intestinal motility, as a result of which digestive enzymes do not have time to act on carbohydrates. It manifests itself as liquid yellow or light brown stool with an unpleasant, pungent odor. Before defecation, spasmodic pain in the abdomen intensifies, after bowel movement it decreases or disappears completely.
Intestinal infections
Amilorrhea in case of poisoning is caused not only by activation of peristalsis, but also by the direct toxic effect of pathogenic microorganisms on the wall of the small intestine. The symptom is more typical at the onset of the disease, when there is a sufficient amount of partially digested food in the stomach and intestines. Diarrhea occurs, the frequency of which depends on the severity of the intestinal infection. The stool is liquid and has a bright yellow, orange or greenish tint.
Hyperacid gastritis
The appearance of amilorrhea is due to two mechanisms: inactivation of salivary amylase in the acidic environment of the stomach and accelerated movement of chyme due to the irritating effect of acid on the small intestine. Stool disorders are associated with errors in diet - consuming large amounts of complex carbohydrates. One- or two-time diarrhea with the release of liquid, foul-smelling feces is observed. Amilorrhea is accompanied by abdominal cramps and epigastric pain.
Chronic pancreatitis
With inflammation of the pancreas, signs of amilorrhea are relatively rare, which is explained by the high enzymatic activity of intestinal amylase. The condition is more often observed in advanced forms of the disease. Amilorrhea occurs when the diet consists primarily of carbohydrate foods. A person is worried about severe flatulence and pain in the epigastric region. Then unformed, foul-smelling stool appears, which may contain particles of undigested food.
When following a diet, amilorrhea disappears. Chronic pancreatitis is characterized by a sequence of changes in the composition of feces. First, steatorrhea occurs, as evidenced by grayish soft feces with a greasy sheen. Later, creative rhea occurs; in the later stages of the disease, amilorrhea develops. The symptom is also typical of a complication of pancreatitis - pancreatic fibrosis.
Pancreatic enzyme deficiency
Violation of the exocrine function of the organ is accompanied by a decrease in the production and release of pancreatic amylase into the small intestine. In the initial stages, the condition is compensated by intestinal enzymes, but in advanced stages of the disease, amilorrhea may begin. It has typical clinical manifestations specific to the chronic form of pancreatitis. The main causes of exocrine pancreatic insufficiency:
- Congenital pathologies
: genetic enzyme deficiency, agenesis or hypoplasia of the pancreas, Shwachman-Diamond syndrome. - Space-occupying formations
: congestive, tumor and parasitic cysts, pancreatic cancer. - Postoperative complications
: during operations on the stomach, small intestine, pancreatic gland.

Chronic enteritis
With inflammatory damage to the wall of the small intestine, the secretion of enzymes is disrupted, and the processes of cavity and parietal digestion are inhibited. Undigested carbohydrates in the form of starch move into the large intestine, increase peristalsis and increase the wateriness of stool. Therefore, with amilorrhea, repeated diarrhea occurs. The stool has a liquid consistency or is released in separate soft lumps.
Complications of pharmacotherapy
Amilorrhea is provoked by an overdose of laxatives, which affect intestinal motility. As a result, a person develops diarrhea. Food quickly passes through the gastrointestinal tract and does not have time to be completely broken down. Feces are abundant, liquid, and have a strong, unpleasant odor. Amilorrhea is combined with cramps and discomfort in the abdomen, flatulence. After 12-24 hours, the effect of the medications ends and the condition returns to normal.
Starch in a child’s stool - what is it, what causes it and how to treat it?

Starch is a polysaccharide that breaks down into its component parts (monosaccharides) and is absorbed by the child’s intestines. In case of gastrointestinal disorders, starch grains are found in the feces of children. In medical practice, such dysfunction is called amilorrhea. To clarify the diagnosis, a scatological examination is performed to determine the presence of starch in the child’s stool.
Treatment
Treatment will depend on the identified pathology, its severity and rate of development. If no organic disorders are detected, amilorrhea is considered functional. In this situation, only diet and regular monitoring by a gastroenterologist are indicated. For pathological amylorhea, medications are added to therapy.
Diet
The basis of nutrition for pathologies of the pancreas and small intestine is the rejection of spicy, fried and too fatty foods. It is recommended to steam, boil or bake all dishes in the oven. Reducing the usual volume of portions, frequent and split meals will be beneficial. Often, following a diet allows you to get rid of the problem and avoid drug therapy.
| Recommended Products | Not recommended products |
|
|
Diet should not be a one-time event, but a habit for life. This is the only way to avoid exacerbation of chronic pathology and prevent the progression of the disease.
Medications

Enzymes that facilitate the digestion of food and replace pancreatic amylase.- Drugs that reduce gastric acidity - antacids.
- Drugs that slow down intestinal motility.
- Antidiarrheal drugs.
- Sorbents (for diarrhea caused by intestinal infection).
After the exacerbation subsides, the following are prescribed:
- Vitamins to improve immunity and maintain overall body tone.
- Probiotics to restore normal intestinal flora and prevent dysbiosis.
The treatment regimen is determined by the gastroenterologist taking into account the identified pathology.
Features of stool analysis in a child, main indicators
If gastrointestinal dysfunction is suspected, the doctor prescribes a stool test, since amilorrhea cannot be suspected by the appearance of the child. With the help of stool analysis, the diagnosis will not only be confirmed, but also treatment will be selected. When conducting tests, the following indicators are taken into account:
- amount of material (depending on the age and weight of the person);
- shape (normally cylindrical);
- consistency (with sufficient water consumption it is soft);
- Brown color);
- specific smell;
- leftover food;
- secretions that are absent in healthy people (red blood cells, pus);
- parasites and their eggs.
Chemical studies are carried out to determine the acidity (ph) of feces and breakdown products that should be absent (red blood cells, proteins, bilirubin). In healthy children, stool acidity (ph) varies from slightly alkaline to slightly acidic. For an accurate result of stool coprogram, stool is examined under a microscope. It detects the presence of complex saccharides, which look like grains under a microscope.
The cause of amilorrhea depends on the type of starch detected in the baby's stool, any of which should not be observed in the feces.
- Intracellular starch is covered with a membrane that is broken down by enzymes. Completely digestible. The presence of this type indicates impaired intestinal function and decreased peristalsis. The carbohydrate is evacuated without having time to be absorbed.
- Extracellular starch - found when there is a lack of amylase in parts of the digestive system, insufficient production of gastric juice.
Based on the obtained stool coprogram, the attending physician will select therapy based on the collected medical history. It takes into account the patient's age.
Important! When transferring the collected material, the patient’s age is signed; the presence of a small amount of complex carbohydrates (starch) in children under 2 years of age is the norm.
Explanations for the table
Typically, the number of detected bacteria in the analysis form is indicated by the number 10 to some degree: 103, 105, 106, etc. and the abbreviation CFU/g, which means the number of living bacteria capable of growing in 1 g of feces.
The abbreviation “abs” next to the name of the bacterium means that this microorganism was not found within the normal range or above it, and values below the norm (subnormal) were not considered as insignificant.
Bifidobacteria
Bifidobacteria are the basis of the normal microflora of the large intestine. Normally, their content in the intestines should be 1010-1011 in children under one year old, and 109-1010 CFU/g in adults. A noticeable decrease in the number of bifidobacteria is the main sign of the presence of dysbiosis and immune disorders.
Deficiency of bifidobacteria leads to increased intoxication, disruption of carbohydrate metabolism, absorption and assimilation of vitamins, calcium, iron and other micro- and macroelements in the intestines. Without a biofilm of bifidobacteria, the structure of the intestinal mucosa changes and the functions of the intestinal mucosa are disrupted, the number of immune cells and their activity decreases, and intestinal permeability to foreign agents (toxins, harmful microbes, etc.) increases. As a result, the toxic load on the liver and kidneys significantly increases, the risk of developing infections and inflammations, vitamin deficiencies and various microelementoses increases.
Lactobacilli
Lactobacilli, as well as bifidobacteria, are one of the main components of normal human microflora. The normal content in the intestines of children under one year of age is 106 - 107, in adults - 107-108 CFU/g. A significant decrease in the number of lactobacilli indicates not only dysbiotic disorders, but also that the body is in a state of chronic stress, as well as a decrease in antiviral and antiallergic protection, disorders of lipid metabolism, histamine metabolism, etc. Lactobacillus deficiency greatly increases the risk of developing allergic reactions, atherosclerosis, neurological disorders, cardiovascular diseases, can also cause constipation and the development of lactase deficiency.
Bacteroides
Bacteroides are opportunistic bacteria. The second largest group (after bifidobacteria) of intestinal microorganisms, especially in adults (the norm is up to 1010 CFU/g), in children under one year of age - 107-108. When kept within normal limits, they perform many beneficial functions for the body. But if the balance in the intestinal microcenosis is disturbed or if the norm is exceeded, bacteroids can lead to a variety of infectious and septic complications. With excessive growth, bacteroids can suppress the growth of E. coli by competing with it for oxygen. The uncontrolled growth of bacteroids and their manifestation of aggressive properties limit the main components of the protective flora - bifidobacteria, lactobacilli and propionic acid bacteria.
Enterococci
Enterococci are the most common opportunistic microorganisms found in the intestines of healthy people. The content norm for children under one year is 105-107, for adults – 105-108 (up to 25% of the total number of coccal forms). Some experts consider them harmless. In fact, many enterococci are capable of causing inflammatory diseases of the intestines, kidneys, bladder, reproductive organs, not only when they exceed the permissible amount (with a content of more than 107), but also in an amount corresponding to the upper limit of normal (106-107), especially in humans with reduced immunity.
Fusobacteria
Fusobacteria are opportunistic bacteria, the main habitats of which in the human body are the large intestine and the respiratory tract. The oral cavity of an adult contains 102-104 CFU/g of fusobacteria. The permissible amount in the intestines in children under one year of age is < 106, in adults - 108 - 109.
Some types of fusobacteria in immunodeficiencies can cause secondary gangrenous and purulent-gangrenous processes. With tonsillitis, herpetic stomatitis, malnutrition in children, and immunodeficiency states, the development of fusospirochetosis is possible - a necrotic inflammatory process on the tonsils and oral mucosa.
Eubacteria (lat. Eubacterium)
They belong to the main resident microflora of both the small and large intestines of humans and make up a significant part of all microorganisms inhabiting the gastrointestinal tract. The permissible amount of eubacteria in the stool of healthy people: in children of the first year - 106-107 CFU/g; in children over one year old and adults, including the elderly - 109-1010 CFU/g.
Approximately half of the species of eubacteria living in the human body can participate in the development of inflammation of the oral cavity, the formation of purulent processes in the pleura and lungs, infective endocarditis, arthritis, infections of the genitourinary system, bacterial vaginosis, sepsis, abscesses of the brain and rectum, and postoperative complications.
An increased content of eubacteria is found in the feces of patients with colon polyposis. Eubacteria are rarely found in breastfed children, but in bottle-fed children they can be detected in quantities corresponding to the norm for an adult.
Peptostreptococci
Peptostreptococci belong to the normal human microflora. The normal content in feces in children under one year of age is <105, in children over one year of age and adults - 109 - 1010. In the body of a healthy person, peptostreptococci live in the intestines (mainly in the colon), oral cavity, vagina, and respiratory tract. Typically, peptostreptococci are causative agents of mixed infections, manifesting themselves in associations with other microorganisms.
Clostridia
Opportunistic bacteria, representatives of putrefactive and gas-forming flora, the number of which depends on the state of local intestinal immunity. The main habitat in the human body is the large intestine. The permissible amount of clostridia in children under one year of age is no more than 103, and in adults - up to 105 CFU/mg.
In combination with other opportunistic flora, clostridia can cause stool liquefaction, diarrhea, and increased gas formation, which, along with the rotten smell of feces (symptoms of putrefactive dyspepsia), is an indirect sign of increased numbers and activity of these bacteria. Under certain conditions, they can cause necrotic enteritis and cause foodborne illness, accompanied by watery diarrhea, nausea, abdominal cramps, and sometimes fever.
When taken with certain antibiotics, clostridia can cause antibiotic-associated diarrhea or pseudomembranous colitis. In addition to intestinal problems, clostridia can cause diseases of the human genitourinary organs, in particular acute prostatitis. The symptoms of inflammation caused by clostridia in the vagina are similar to the symptoms of candidal vaginitis (“thrush”).
E.coli typical (Eschechiria, E. coli typical) , i.e. with normal enzymatic activity
Opportunistic microorganisms, which, together with bifidobacteria and lactobacilli, belong to the group of protective intestinal microflora. This bacillus prevents the colonization of the intestinal wall by foreign microorganisms, creates comfortable conditions for other important intestinal bacteria, for example, absorbs oxygen, which is a poison for bifidobacteria. This is the main “vitamin factory” in the body.
Normally, the total content of E. coli is 107-108 CFU/mg (which corresponds to 300-400 million/g). Elevated levels of E. coli in the intestines can cause inflammation, accompanied by stool problems and abdominal pain. And its penetration from the intestines into other ecological niches of the body (urinary tract, nasopharynx, etc.) is the cause of cystitis, kidney diseases, etc.
A decrease in this indicator is a signal of a high level of intoxication in the body. A strong decrease in the number of typical E. coli (up to 105 CFU/mg and below) is an indirect sign of the presence of parasites (for example, worms or parasitic protozoa - Giardia, blastocysts, amoebas, etc.). In addition to parasites, among the most likely reasons for a decrease in E. coli levels are the existence of foci of chronic infection in the body, increased allergization, dysfunction or diseases of various organs, primarily the liver, kidneys, pancreas and thyroid glands. To avoid misdiagnosis and, accordingly, incorrect treatment, it is recommended to first exclude parasitic infection.
Escherichia coli with reduced enzymatic activity (E.coli lactose-negative).
The content rate is no more than 105 CFU/g. This is an inferior variety of E. coli, which usually does not pose a direct danger. But this stick is a parasite. It takes the place of full-fledged E.coli, without performing the beneficial functions inherent in full-fledged E.coli. As a result, the body does not receive enough vitamins, enzymes and other beneficial substances synthesized by full-fledged Escherichia, which ultimately can lead to serious metabolic disorders and even inflammatory diseases. The presence of this bacillus in quantities above the permissible norm is always a sign of incipient dysbiosis and, along with a decrease in the total amount of E. coli, can be an indirect indicator of the presence of parasitic protozoa or worms in the intestines.
E. coli hemolytic (hemolytic Escherichia coli)
Pathogenic variant of Escherichia coli. Normally it should be absent. Its presence requires immunocorrection. May cause allergic reactions and various intestinal problems, especially in young children and those with weakened immune systems. It often forms pathogenic associations with Staphylococcus aureus, but unlike it, it is practically not found in breast milk.









