In recent decades, there has been a steady increase in the number of patients with thyroid pathology. Studies conducted both in our country and abroad show that there has been no true increase in the incidence of endocrine diseases, the quality of their diagnosis has simply improved. Now every patient can perform an ultrasound examination or take a test to determine thyroid hormones. Often, an ultrasound of the thyroid gland is performed on patients simply “at the same time” as the examination of other organs. Improved diagnostics are yielding results: according to statistics, every second or third resident of our country has signs of thyroid disease. Meanwhile, no increase in mortality from thyroid diseases has been noted in recent decades.
Thyroid nodules are the most common type of pathology of this organ. A nodule is an area that differs in density or color on ultrasound from the rest of the thyroid tissue and has clear boundaries. If we feel the gland and feel a compaction with clear boundaries in it, this is a node. If we do an ultrasound and see a light or dark spot against the background of the rest of the gland tissue, this is also a node. An increase in the volume of the thyroid gland, as well as the presence of nodes in it, is designated by the term “goiter”. Diffuse goiter is said to occur when the gland tissue is evenly enlarged and does not contain any compactions. Nodular goiter is a situation accompanied by the appearance of nodes in the gland tissue. According to modern data, ultrasound examination can reveal nodules in the thyroid tissue of 30-67% of Russian residents. In the vast majority of cases (95%), these nodes are benign, and only in 5% of patients they are malignant tumors. With age, the frequency of detection of nodes increases. Thyroid nodules are rare in children, while up to 80% of people aged 60 years and older have nodules. But in children and men, malignant nodes are detected 2 times more often than in adults and women, respectively. The ratio of men to women is approximately 1:10.
Nodules can be either benign (colloid nodes, follicular adenomas, cysts and inflammatory diseases of the thyroid gland) or malignant (thyroid cancer - papillary, follicular, B-cell, medullary, anaplastic, etc.).
Causes of knots
It is currently believed that the main cause of thyroid nodules is a chronic lack of iodine in the diet. The iodine supply of the population affects the number of benign thyroid nodules (so-called colloid nodules). Some nodes, mainly represented by tumors, arise after exposure to a flow of ionizing radiation on the human body. Heredity also plays a certain role. It is known that in relatives of patients with thyroid diseases, the likelihood of detecting nodules is increased.
Mechanism of appearance of nodes
According to the mechanism of appearance, thyroid nodules can be divided into two main groups - tumors and “non-tumors”. Tumor nodes appear due to the occurrence of a mutation in one of the thyroid cells (A, B, or C-type). The cause of mutation is damage to the genetic material of the cell located in its nucleus. This damage can be caused by radiation, exposure to certain chemicals (such as heavy metals). In some cases, such mutations can be inherited. Benign tumors, as they grow, push apart the surrounding thyroid tissue. An enlarged tumor leads to atrophy of the gland tissue due to compression by the tumor tissue. Benign cells do not acquire the ability for infiltrative growth, i.e. penetration between thyroid cells. The main property of malignant tumors is the possibility of infiltrative growth. The tumor can grow not only into the thyroid gland, but also into surrounding organs - the trachea, esophagus, muscles, and blood vessels.
Metastasis occurs by hematogenous and lymphogenous routes. The properties of the tumor directly depend on the type of cell in which the mutation occurred. A cells are the source of follicular adenomas and carcinomas, papillary carcinoma, anaplastic cancer, B cells (Hurthle cells) give rise to Hurthle cell adenomas and carcinomas, and C cells give rise to medullary thyroid carcinoma.
Treat or remove?
Often, cysts form on the ovaries of fairly young women due to the accumulation of secretory fluid in the tissue. Typically, a cyst has the appearance of a bubble, which includes one or more chambers where fluid is located. If it is transparent and resembles water in appearance, then it is a serous cyst; when the content is closer in consistency to mush, then such a cyst is called dermoid. Often, the dermoid cyst is congenital, and the serous cyst is acquired. The contents of the cystic vesicle are determined using a puncture.
As far as we know, nature abhors emptiness. And since the cyst is a pathological void, the female body quickly fills it with some liquid content. The walls of the cyst are thin, but they consist of cells that are very productive, that is, they produce fluid that fills the cyst. Thanks to this remaining fluid, the cyst itself continues to develop. When the development is not rapid, then the formation itself does not in any way affect the general state of women's health, then such a cyst can be removed in no hurry. In this case, it will be quite enough to be under regular supervision of a gynecologist.
In the case when the size of the cyst increases continuously, which negatively affects neighboring healthy organs, then surgical intervention is inevitable. Doctors motivate the removal of such cysts for the following reasons:
- often the presence of a cyst is the main cause of a woman’s infertility;
- the cyst may become infected;
- certain types of cysts may become malignant in the future;
- the cyst will not “resolve” spontaneously, it can only increase in size.
When is an anechoic formation in the ovary
detected in a woman who has already crossed the fifty-year age barrier, then in most situations we are talking about the presence of cancer, and prolonged reflection often becomes simply dangerous.
Modern diagnostic methods
A. Examination: examination reveals an enlargement of the thyroid gland, asymmetry in the size of the lobes, characteristic of the presence of nodes, enlarged lymph nodes, as well as a number of other signs important for diagnosis (nervousness and fussiness of the patient, exophthalmos, shine in the eyes characteristic of thyrotoxicosis, etc.) . Information about the rapid growth of the identified node, the appearance of hoarseness, cough, and problems with swallowing and breathing is important.
B. Ultrasound examination (US) is the next step in the diagnostic process. During the study, it is possible to identify areas of heterogeneity in the thyroid tissue measuring 2-3 mm. The sensitivity of ultrasound significantly exceeds the capabilities of palpation. It is known that in 20-50% of patients with a single node identified by palpation, ultrasound can identify additional nodes. It is important to perform a Doppler study when performing an ultrasound, i.e. study of the intensity of blood flow inside the node. The main purpose of ultrasound when examining patients with nodes is to identify those who need TAB. According to modern concepts, formations smaller than 1 cm in size do not need to be subjected to further research. All nodes with a diameter of 1 cm or more are subject to a study of the cellular composition of the node - fine-needle aspiration biopsy (FNA). No other research methods, except biopsy, can reliably exclude malignancy of the node.
B. Fine needle aspiration biopsy. The research methodology is as follows. Under ultrasound guidance, the doctor performs a puncture (injection) into the thyroid nodule of the thyroid gland with a thin needle connected to an empty syringe. After the tip of the needle is inside the node, the doctor aspirates (sucks in) the contents of the node several times with a syringe. The needle is then removed and the contents of the node are applied to laboratory glass. Most often, 2-3 injections are made in different parts of the node to obtain a sufficient amount of biological material and eliminate the possibility of error. The entire procedure takes no more than 1 minute and is well tolerated by all patients. A sterile sticker is glued to the injection site and after 5-10 minutes the patient can go about his business. 2 hours after the biopsy, you can wash, exercise, etc. The result of FNA is to obtain a cytological report describing the nature of the node. Currently, according to modern classifications, almost all cytological conclusions are reduced to 5 main options: 1. "Colloidal node". A punctate node is a benign non-tumor formation. There are no signs of cancer, and there is no likelihood of the node “degenerating” into a malignant tumor.2. “Hashimoto’s thyroiditis” (“Autoimmune thyroiditis”. The punctured formation is an area of inflammatory changes in the tissue of the thyroid gland. There are no signs of malignant growth, the situation is completely favorable. 3. “Follicular tumor”. The situation is suspicious regarding the presence of a malignant process in the punctured node. It is known that among follicular tumors 85% are represented by adenomas (i.e. they are benign), and 15% are carcinomas 4. “Papillary carcinoma”, “Medullary arcinoma”, “Squamous cell carcinoma”, “Anaplastic carcinoma”, “Lymphoma”. the node is a malignant tumor. 5. “the material is uninformative.” Such answers make up 4-5% of the conclusions. A repeat study is carried out.
D. Blood test for hormone levels. To resolve the issue of the state of thyroid function, it is sufficient to determine the level of thyroid-stimulating hormone (TSH) in the blood. If the TSH level deviates beyond the established norm, the patient is recommended to conduct a study of the level of free fractions of the hormones T3 (triiodothyronine) and T4 (thyroxine) to clarify the diagnosis. The titer of antibodies to thyroid tissue - antibodies to thyroid peroxidase (Ab to TPO) is also determined. An increased titer of antibodies indicates the presence of an autoimmune reaction in the patient and allows us to identify some diseases of the thyroid gland - autoimmune thyroiditis. An increase in calcitonin levels strongly indicates the presence of medullary carcinoma in a person. Determination of antibodies to the TSH hormone receptor - a high level indicates the presence of diffuse toxic goiter in a person.
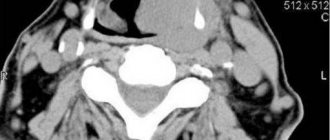
D. Additional methods include scintigraphy of the thyroid gland with isotopes of iodine or technetium. The study helps determine the level of accumulation of drugs in the thyroid tissue and nodes, and thereby identify areas that do not accumulate the drug, and therefore do not produce hormones, and others that intensively accumulate isotopes, and therefore are hormonally active. X-ray of the esophagus with barium contrast allows you to see the contour of the esophagus, which can be deviated when compressed by a large node. CT and MRI of the neck - study the spread of an enlarged gland into the chest when identifying a retrosternal goiter, lymphadenopathy of the chest cavity, show compression of the esophagus or trachea.
Terminology
During ultrasound examinations of the internal genital organs, patients have the maximum number of questions regarding anechoic formations of the ovary. If you break this word into several components, you get literally the following: an - translated as negation, absence; echo is sound; genetic - educated, born. If you combine all this, then it turns out: some kind of formation (inclusion, tissue) that does not reflect sound. Usually liquids cannot reflect sound. Thus, an anechoic formation in the ovary is often represented by either the corpus luteum of the ovary or a follicular cyst. However, anechoic formations cannot in any case be considered a diagnosis, since this is only a description of the ultrasound examination that the woman underwent.
Surgical treatment of patients with benign nodes is carried out in the following cases
- if the node has reached such a size that it begins to compress the organs of the neck and cause a feeling of suffocation, disrupt the swallowing process, or cause the patient to feel a “foreign body”.
- with a cosmetic defect, deforming the front surface of the neck.
- during the formation of an autonomous or toxic node (causing the appearance of thyrotoxicosis).
Surgical treatment is indicated for all patients who have received a cytological conclusion about the presence of thyroid cancer in the test node or if the presence of a malignant tumor is suspected, i.e. with the cytological picture of a follicular tumor (at present there are no methods that allow one to clearly determine the nature of such nodes).
Patients suffering from diffuse toxic goiter (Graves disease) also need radical treatment if thyrotoxicosis relapses 1.5-2 years after a course of drug therapy with thyreostatics. In some cases, surgery is prescribed earlier: the volume of the thyroid gland is more than 40 ml, drug intolerance, pregnancy planning.
In case of autoimmune thyroiditis, surgical treatment is required for patients with a hypertrophic form of thyroiditis (Hashimoto's goiter), in which there is a significant increase in the volume of the thyroid gland, i.e. with the development of compression syndrome - impaired swallowing and breathing.
Corpus luteum
In addition, ultrasound examination can detect another anechoic formation of the ovary
in women - the so-called corpus luteum, which is an endocrine gland that appears cyclically (during ovulation). Its function is to produce the main female hormones: estrogen and progesterone. Both the corpus luteum itself on the ovary and the cyst that can sometimes form on it do not reflect sound. Such a cyst poses absolutely no threat. Even more: the absence of pregnancy in the early stages is even considered an unfavorable factor, which indicates the presence of hormonal deficiency in a woman.
isoechoic ovarian formation