The text is presented for informational purposes only. We strongly urge you not to self-medicate. When the first symptoms appear, consult a doctor. We recommend reading: “Why you can’t self-medicate?”
One of the indicators of digestive disorders is the detection of starch in feces. In medicine, this condition is called amilorrhea. During normal digestion, starch must be broken down into simple substances.
In childhood, starch in feces does not always indicate pathology due to the general immaturity of the body and the digestive system in particular.
Medical products (drugs, medicines, vitamins, dietary supplements) are mentioned for informational purposes only. We strongly do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
Causes of increased starch
An increased content of starch grains in feces is called amilorrhea. There are several reasons for the occurrence of this disease:
- the presence of an inflammatory process on the intestinal walls;
- gastritis;
- pancreatitis;
- disturbances in the functioning of the pancreas;
- dyspepsia.
Improper absorption of starch by the body, in most cases, is associated with problems in the pancreas or diseases of the small intestine.
Thus, starch, which can be found in a child’s feces, simply does not have time to be digested.
If the disease appeared in a child under one year old?
In infants (up to one year), amilorrhea is not necessarily associated with the presence of any disease.
If the child is breastfed, then there should be no starch in principle. The presence of starch in the feces of babies is considered normal, since the secretory glands at this age are not yet sufficiently developed.
Amilorrhea goes away on its own as it gets older. The only thing you can do is adjust your diet.
It is recommended to reduce the consumption of potatoes, pears, bananas and other starchy foods. If the problem cannot be solved in this way, then the child must be shown to a gastroenterologist, remember this for the future.
Diagnosis of the cause
The doctor orders laboratory tests.
The most reliable analysis is a coprogram, with the help of which the following information is obtained:

- level of activity of digestive enzymes;
- level of excretory function of the gastrointestinal tract;
- activity of intestinal microflora;
- the presence of an inflammatory process in the gastrointestinal tract;
- presence of helminthic infestations.
During the examination of stool, the shape of feces, color shade, smell, the presence of food debris, and other inclusions (parasites, eggs, mucus, blood, etc.) are taken into account.
For example, if there are remains of undigested food in biological material, we can indirectly say that intestinal motor function is increased and there is a deficiency of digestive enzymes produced by the pancreas.
Stool analysis (coprogram) normally gives the following results:

- stool is brown in color and has a dense consistency;
- any incomprehensible inclusions, mucus, lumps of a different color, blood are absent;
- there is no foul odor, proteins and starch, bilirubin, and leukocyte cells are not detected;
- The normal volume of water in stool is 80%.
To ensure the reliability of the results, it is recommended to study the rules for collecting biological material and preparing for the study:
- 2 days before collecting stool, they begin to adhere to proper nutrition, excluding from the diet foods containing protein, as well as foods that affect the color change of stool and urine (beets, etc.);
- if diagnostics are required for a breastfed child, the nursing woman should follow the diet;
- the container in which biological material is collected is thoroughly washed and disinfected beforehand;
- the study is carried out on the same day on which the material was collected (ideally in the first 5-7 hours after collecting the biopsy);
- before collecting the child’s stool, it is necessary to wash it, otherwise the analysis will show false results (there may be the presence in the masses of chemical compounds, uncharacteristic bacterial microorganisms, epithelial cells and other inclusions that should not be present);
- the optimal volume of biological material is 1 tsp. (this quantity is sufficient to conduct all studies);
It is not recommended to take a biopsy sample from a baby's diaper: in this case, tissue fibers may remain in the stool).
Elevated levels at 1 year
In a one-year-old child, the presence of starch grains in the feces is explained by the fact that the fragile body cannot cope with the volume of this enzyme entering the body. It is during this period that new (which the baby has not tried before) foods containing starch begin to be added to the child’s diet.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
In this case, amilorrhea can be dealt with, again, by adjusting the diet. You should consult a doctor if your child regularly experiences stomach upsets, manifested by diarrhea and vomiting. Perhaps the baby is already suffering from some kind of gastrointestinal disease.
If the baby with bad tests is 2 years old?
In a two-year-old child, the increased content of starch in the feces is explained, in most cases, by a malfunction of the small intestine, for example, by its increased peristalsis.
If the baby is not bothered by any problems associated with gastrointestinal disorders (frequent loose stools, regular indigestion), then there is no need for drug treatment.
In this case, you can get by with a special diet prescribed by a pediatric gastroenterologist. If, during a repeated general stool analysis, starch is present again, then a more detailed examination is necessary, for which the treating pediatrician will issue a referral.
Method for detecting starchy compounds in feces in adults
Stool analysis to detect undigested starch is a coprogram. Here the entire digestive function is assessed. The coprogram includes the following indicators:
- consistency and color of stool;
- undigested food particles;
- fat;
- number of starch grains;
- muscle fibers;
- bacteria, protozoa, helminth eggs.
Using a coprogram, you can detect many pathologies that occur with damage to the gastrointestinal tract.
The presence of starchy compounds can be determined by the appearance of stool. They become abundant and soft. The color is yellowish-gray, the surface is shiny. The stool looks greasy and sticks to the walls of the toilet. A sharp unpleasant odor appears.
What does increased starch mean in a 3-year-old child?
At the age of three years, amilorrhea in a child manifests itself for several reasons.
These can be both gastrointestinal diseases and unhealthy diet. Children from families where parents do not adhere to a healthy diet are at particular risk.
If, in addition to the presence of starch grains in the stool, the child is regularly bothered by pain in the abdomen, stomach, or loose stools, then a thorough examination of all digestive organs is necessary.
The cause of illness can be such serious diseases as gastritis and pancreatitis. In advanced cases, these diseases can lead to serious consequences.
Associated symptoms
If the cause of the appearance of starch in the feces is pathological changes in the digestive system, then the mother should pay attention to the accompanying symptoms:
- abdominal pain;
- rumbling along the intestines;
- stool disorders in the form of diarrhea, increased stool volume;
- nausea;
- vomit;
- flatulence;
- intestinal colic;
- the presence of other pathological impurities in the stool: blood, mucus, undigested muscle fibers;
- temperature increase.
What needs to be done?
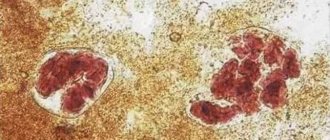
Examination of stool for the presence of starch grains is called coprogram . This analysis involves identifying the chemical and physical properties of feces, as well as identifying various impurities. Starch found in feces is divided into two types:
- Extracellular. The reason for its appearance is a malfunction of the pancreas or the lack of amylase in saliva.
- Intracellular. Starch appears due to the small intestine working too quickly. Products containing starch simply do not have time to be digested.
The child is prescribed either medication or diet. The choice of treatment depends on the cause of the appearance of starch and the age of the baby.
What is pathology?
Starch is a carbohydrate that is found in many foods consumed by humans, especially in plant foods: rice, wheat, corn, oats, potatoes, and legumes.

The process of digestion of starchy products and, directly, starch, begins in the oral cavity.
The food is mixed with saliva, which is rich in the digestive enzyme ptyalin (amylase). Digestion continues in the stomach .
After this, amylase is neutralized by hydrochloric acid contained in gastric juice. Next, the food passes into the intestinal environment, mixing with pancreatic juice, which contains amylase in a larger volume than saliva.
The completion of the digestive process is in the small intestine. The final product of starch breakdown is glucose, which is absorbed by the body.
If there are no diseases of the digestive system and the gastrointestinal tract is working at full capacity, the presence of starch in the stool is not diagnosed or is detected in scant quantities.
Large amounts of carbohydrate found in the form of intracellular and extracellular starch granules indicate pathology.
Effective Treatments
If the doctor decides to treat with medications, the child is prescribed probiotics .
These medications have a positive effect on the intestinal microflora, normalizing the functioning of the gastrointestinal tract. For example, Duphalac or Florin Forte.
In addition, the doctor prescribes a vitamin complex that helps normalize the functioning of the digestive system.
If the cause of the presence of starch grains in the feces is diseases such as gastritis or pancreatitis, then the child is prescribed additional examination , and treatment depends on its results. Parents should never self-medicate their child, as this can lead to the chronic form of certain gastrointestinal diseases.
Intestinal infections
Intestinal infections are quite common in infants. Even the most careful and clean parents cannot always avoid the development of an intestinal infection in their baby. The fact is that the protective functions of the intestines (acidity of gastric juice, local immune factors) in infants are not yet fully formed, and some pathogens that are not dangerous for adults can cause serious disorders in an infant.
As a rule, the infection begins suddenly - with abdominal pain (the child cries, kicks his legs) and diarrhea (sometimes with inclusions of mucus, greens, blood and other impurities). Intestinal infections may be accompanied by a rise in temperature, but this does not always happen. If any of the described symptoms appear, be sure to call a doctor, and before he arrives, try to alleviate the child’s condition with the following measures:
- With loose stools, the child loses a lot of water and salts, and he may become dehydrated. To prevent this from happening, the baby must be given one of the saline solutions - for example, Oralite, Rehydron. The drug enterodez, in addition to salts, also contains activated carbon, which adsorbs toxins from the intestines. One of these drugs should be kept in your home medicine cabinet at all times. It is very important to completely replace the child with the volume of fluid that he loses through stool and vomiting (it is advisable to measure this volume). If the baby does not drink from a bottle, liquid can be given from a spoon or even from a pipette - small portions of liquid do not provoke vomiting as much as large ones. It is not advisable to give your child regular boiled water, since a lot of salts are lost with intestinal contents - if you give liquid without salts, this deficiency will worsen.
- In addition to fluid replenishment solutions, the child can be given adsorbents (smecta, polyphepan, enterosgel) - drugs that, like a sponge, absorb toxins contained in the intestines. But keep in mind that while these drugs absorb toxins, they do not destroy pathogenic bacteria. In large quantities they can lead to constipation.
- Should I feed my child in the midst of an intestinal infection? Yes, feed. But the amount of food per day should be reduced by 1/3-2/3 compared to normal (depending on the maximum amount of food that does not lead to vomiting). If the child is breastfed, then continue to feed him breast milk; in such situations, it is better to give artificial milk formulas to artificial babies. Feed more often, but in small portions. You can add 1/4 tablet of the enzyme preparation Mezim-Forte to each feeding. Here, perhaps, are all the measures that can be taken before the doctor arrives.
- Never give an infant antibiotics without a doctor's prescription: some of the antibiotics often used for intestinal infections in adults are contraindicated in newborns (for example, chloramphenicol). Great care should be taken when using drugs such as Imodium and other symptomatic drugs in infancy - be sure to consult your doctor.
How to protect a child from intestinal infections?
- First of all, you should pay attention to the dishes from which you feed your baby. It should be dry. Some mothers boil bottles for a long time, but then leave some of the moisture in them. Moisture promotes the growth of bacteria.
- Secondly, you should not often pour food from one dish to another - the less often you do this, the better. That is why modern breast pumps are immediately connected to a feeding bottle.
- Finally, avoid licking pacifiers, spoons, and other baby utensils. The germs in your mouth are not always safe for your baby (for example, Helicobacter, which causes peptic ulcers, or germs that cause tooth decay). Pathogenic bacteria are transmitted mainly from person to person, so it is better to simply rinse a pacifier that has fallen on the floor with water (at worst, not even wash it at all) than to lick it.
What diet is suitable?
Another treatment option is based on dietary nutrition . The patient is strictly contraindicated from consuming too fatty meat and fish broths, as well as any spicy, salty or smoked food.
The child must be given large quantities of mineral water without gas - this helps to wash out starch. If starch is detected in an infant, the woman’s diet should be reconsidered.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
It is also necessary to exclude (or significantly reduce) the consumption of potatoes from the diet. You can replace it with zucchini, and if this is impossible for some reason, then the potatoes must be cooked with preliminary soaking of the starch.
Treatment
Treatment of isolated amilorrhea should begin with diet therapy. If, upon repeated examination a month later, the results of the coprocytogram have not changed, then it is necessary to conduct an examination to identify the cause and initiate drug treatment of the underlying pathology.
Diet
The basic principles of diet therapy for a child who switches from breastfeeding to a common diet are:
- temporary restriction of plant foods;
- gradual introduction of new food products;
- mechanical and thermal processing of plant products.
In older age, it is necessary to direct nutrition to maximum unloading of the pancreas:
- limit the amount of sweets;
- avoid overeating (fractional meals in small portions 5-6 times a day);
- temporarily exclude fresh vegetables and fruits, fatty foods, and fried foods.
| Recommended Products | Not Recommended Products |
|
|
It is recommended to limit the consumption of cereals, as they contain a lot of starch and the load on the pancreas increases.
Drug therapy
If after a month of diet the tests have not improved, then after the examination the most often necessary groups of drugs are:
- Probiotics and prebiotics (Bifidumbacterin, Bifiform, Linex). Helps normalize microflora and improve peristalsis.
- Pancreatic enzymes (Creon, Pancreatin, Mikrasim). They are used as replacement therapy, allowing maximum relief of the pancreas for its restoration. The drugs are gradually withdrawn.
- Antidiarrheal drugs (Enterol, Bifiform). Allows you to normalize intestinal motility and improve digestion.
Specific treatment for the detected pathology is also prescribed: antibacterial therapy for intestinal infections, bacteriophages for dysbiosis, anthelmintic drugs for helminthiasis, and so on.