Chronic lymphocytic leukemia is a malignant lymphoproliferative disease in which the tumor cells are pathological B lymphocytes that can accumulate in the bone marrow, peripheral blood and lymph nodes. Normally, B lymphocytes during their life transform into an immunoglobulin-secreting cell, which provides acquired immunity. Tumor B-lymphocytes are deprived of this function, and, thus, the patient’s immunity suffers and the risk of infectious diseases increases. In addition, as the disease progresses, the production of red blood cells, neutrophils and platelets is impaired, and autoimmune processes may develop. Finally, chronic lymphocytic leukemia can transform into B-cell prolymphocytic leukemia, into well-differentiated non-Hodgkin lymphoma, in particular into diffuse large B-cell lymphoma.
- Reasons for the development of lymphocytic leukemia
- Symptoms
- Diagnosis of chronic lymphocytic leukemia
- Stages of the disease
- Treatment
- Evaluation of treatment effectiveness
- Forecast
Reasons for the development of lymphocytic leukemia
Chronic leukemia is the most common type of leukemia, accounting for up to 30% of the total incidence structure. The incidence rate is 4 cases per 100 thousand population; in persons over 80 years of age, the frequency is more than 30 cases per 100 thousand population.
Risk factors for the development of chronic lymphocytic leukemia are:
- Elderly age. Up to 70% of all identified cases occur in people over 60 years of age,
- Male gender. Men get sick twice as often as women,
- Exposure to ionizing radiation,
- Contact with benzene and gasoline.
Leukemia
Iron deficiency
Pyelonephritis
Angina
24264 June 11
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Leukemia: causes, symptoms, diagnosis and treatment methods.
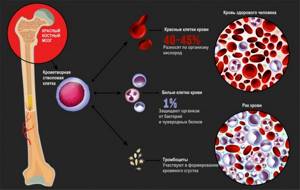
Definition
Leukemia is a large group of diseases of the hematopoietic system. Hematopoiesis (hematopoiesis) is a multi-stage process of formation of formed blood elements in specialized hematopoietic organs. The formed elements of blood include leukocytes (white blood cells), which participate in innate and acquired immunity, erythrocytes (red blood cells), which transport oxygen and carbon dioxide, and platelets, which ensure blood clotting.
All blood cells have one common “ancestor” - a pluripotent stem cell. The term "pluripotent" means that such a cell can develop into various types of mature cells.
The main organ where pluripotent stem cells are located is the bone marrow, which is precisely what is affected in leukemia.
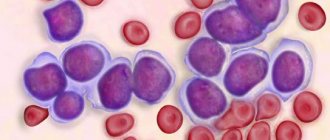
As a result of damage (mutation) in the genetic material of a pluripotent stem progenitor cell, the process of cell maturation is disrupted. In acute leukemia, a large number of immature (blast) cells appear, from which a tumor is formed, grows in the bone marrow, replaces normal hematopoietic germs and tends to metastasize - spread through the blood or lymph flow to healthy organs. In chronic leukemia, the disease lasts for years, there is a partial delay in cell maturation and the tumor is formed from maturing and mature cells.
Causes of leukemia
Risk factors for developing leukemia include:
- ionizing radiation: radiation therapy for other tumors, workplace exposure, ultraviolet radiation;
- exposure to chemical carcinogenic substances on the body;
- some viruses: HTLV (human T-lymphotropic virus);
- household factors: food additives, smoking, poor environmental conditions;
- hereditary predisposition to cancer.
Classification of leukemia
Leukemia is divided into acute and chronic, and according to the type of damage to the hematopoietic germ - into lymphoid and myeloid. Acute leukemia never becomes chronic, and chronic leukemia cannot become acute (but its development can go into the blast crisis stage).
Depending on the predominance of certain tumor cells, blast, cytic and undifferentiated leukemias are distinguished.
Acute lymphoblastic leukemia (ALL) is diagnosed in people of any age, from infancy to the elderly, but the peak incidence occurs in childhood (60% of patients with ALL are younger than 20 years). Acute lymphoblastic leukemia is the most common tumor of hematopoietic tissue in children, accounting for 30% of all malignant tumors of childhood. The incidence of ALL in elderly patients is steadily increasing: thus, the annual incidence of ALL increases from 0.39 cases per 100 thousand population aged 35–39 years, to 2.1 cases per 100 thousand population aged ≥85 years. In addition, approximately 30% of ALL are diagnosed at age ≥60 years.
Acute myeloid leukemia (AML) affects an average of 3-5 people per 100 thousand population per year. The incidence increases sharply over the age of 60 years and amounts to 12–13 cases per 100 thousand population in people over 80 years of age.
Chronic lymphoblastic leukemia (CLL) is the most common type of leukemia in adults, while this type of tumor is not registered in children. In European countries, its frequency is 4 cases per 100 thousand population per year and is directly related to age. In people over 80 years of age, it is more than 30 cases per 100 thousand per year.
Chronic myeloid leukemia (CML) is a rare disease: 0.7 per 100 thousand adults, the peak incidence occurs at 50-59 years of age, but up to 33% of patients with AML are people under 40 years of age.
Symptoms of leukemia
Acute leukemia in most cases debuts abruptly - the temperature suddenly rises, chills, pain in the throat, pain in the joints appear, and pronounced weakness is noted. Less commonly, acute leukemia may present with bleeding. Sometimes acute leukemia begins with a gradual deterioration of the patient’s condition, the appearance of unexpressed pain in the joints and bones, and bleeding. In isolated cases, asymptomatic onset of the disease is possible. In many patients, the lymph nodes and spleen are enlarged.
With chronic leukemia at the initial stage, which lasts from one to three years, patients may not complain about anything. Sometimes you are worried about weakness, sweating, frequent colds, and you may experience dull, aching pain in the bones.
The symptoms of leukemia depend on which hematopoietic lineage is affected.
When the erythroid sprout, which produces red blood cells, is suppressed, anemia and hemic hypoxia occur (decreased amount of oxygen in the blood). In this case, patients note weakness, fatigue, and pale skin.
When the megakaryocyte lineage is damaged, the number of platelets drops, causing bleeding of the gums, nasal mucosa, and digestive tract, bruising, and hemorrhages in various organs. As leukemia progresses, massive bleeding may develop as a result of DIC syndrome (disseminated intravascular coagulation syndrome).
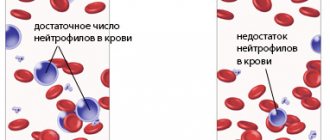
As a result of a lack of leukocytes and decreased immunity, infectious complications of varying severity develop, most often manifested by fever.
Ulcerative-necrotizing tonsillitis, peritonsillar abscesses, necrotizing gingivitis, stomatitis, pyoderma, pararectal abscesses, pneumonia, pyelonephritis may occur. There is a significant risk of severe infectious complications, including the development of sepsis.
With the flow of blood and lymph, tumor cells enter healthy organs, disrupting their structure and function - the liver, spleen, and lymph nodes are most susceptible to metastatic processes, but metastases can affect the skin, meninges, kidneys, and lungs.
The main causes of mortality in patients with leukemia are related to the fact that complications can provoke the development of sepsis, multiple organ failure, and hemorrhages in various organs. Untreated acute leukemia is fatal within weeks or months.
Diagnosis of leukemia
Diagnosis of leukemia is based on assessment of the morphological characteristics of bone marrow and peripheral blood cells. Therefore, all patients with suspected leukemia are prescribed a general blood test with a leukocyte count and platelet count.
Symptoms
Chronic lymphocytic leukemia is characterized by a long asymptomatic course; The main reason for visiting a doctor is changes in a general blood test taken as part of a preventive examination or for another disease. The patient may not present active complaints at the time of the initial examination, but often even in this situation an enlargement of the lymph nodes and a change in their consistency to a doughy consistency are already detected. The lymph nodes themselves are not compacted and remain mobile relative to the surrounding tissues. In case of infection, the lymph nodes become significantly enlarged; As chronic lymphocytic leukemia progresses, lymph nodes—primarily those of the abdominal cavity—are capable of forming conglomerates.
The first complaints that arise are usually not specific: increased fatigue, weakness, severe sweating. As the disease progresses, autoimmune manifestations may occur, firstly very hemolytic anemia (in 10-25% of cases) and thrombocytopenia (in 2-3% of cases). Hemolytic anemia develops due to the destruction of red blood cells by the body itself; Most often, like chronic lymphocytic leukemia itself, it develops gradually, but it can also manifest as an acute crisis - with an increase in temperature, the appearance of jaundice, and darkening of the urine. Thrombocytopenia can be a much more dangerous condition due to the development of bleeding, including life-threatening bleeding (for example, cerebral hemorrhage).
In addition, since B lymphocytes belong to the cells that provide immunity, the addition of infectious complications, including opportunistic ones, that is, caused by microorganisms that are constantly present in the human body and do not manifest themselves with an adequate immune response, is typical. Most often, opportunistic infections affect the lungs.
Lymphocytic leukemia
Lymphocytic leukemia is a malignant disease in which the bone marrow produces a large number of immature lymphocytes that are unable to perform their functions. Lymphocytes are a type of white blood cell and are responsible for immunity. Malignant leukocytes do not cope with the protective function, while suppressing the formation of normal blood cells and disrupting the functioning of other organs.
There are many varieties of this disease. Lymphocytic leukemia is divided depending on the speed of development of the pathological process, the degree of maturity of lymphocytes, and the type of damaged lymphocytes (T- and B-lymphocytes). However, most often there are 2 main types: acute lymphoblastic leukemia and chronic lymphocytic leukemia.
Treatment of leukemia is usually complex. At the moment, there are several treatment options, and every year new, increasingly effective methods for treating lymphocytic leukemia appear. The prognosis for acute lymphocytic leukemia is favorable - 95% of patients are completely cured. The prognosis for chronic lymphocytic leukemia depends on the speed of development of the disease and associated pathologies; it progresses steadily, but appropriate treatment often leads to remission and significant improvement in the patient’s condition.
Synonyms Russian
Acute lymphocytic leukemia, acute lymphocytic leukemia, acute lymphoblastic leukemia, chronic lymphocytic leukemia, chronic lymphocytic leukemia.
English synonyms
Pediatric acute lymphoblastic leukemia, childhood acute lymphoblastic leukemia, acute lymphocytic leukemia, ALL, chronic lymphocytic leukemia, CLL.
Symptoms
Acute lymphoblastic leukemia develops quite quickly - usually within a few weeks. Its symptoms are:
- fever,
- weakness, malaise,
- bleeding gums, frequent nosebleeds,
- stomach ache,
- bone pain,
- headache,
- enlarged lymph nodes in the neck, axillary and groin areas,
- pallor.
Chronic lymphocytic leukemia usually does not manifest itself in any way at the initial stage. It develops over years, and the following symptoms gradually appear:
- frequent infectious diseases,
- increased sweating, especially at night,
- hemorrhages in the skin and mucous membranes,
- heaviness in the stomach,
- weakness, malaise,
- causeless weight loss,
- pallor,
- dyspnea.
General information about the disease
Lymphocytes are a type of white blood cell. Like all other blood cells, lymphocytes are formed from a single stem cell, which is found in the bone marrow and gives rise to lymphoid and myeloid stem cells. Lymphocytes come from the lymphoid stem cell, and other types of leukocytes, erythrocytes and platelets come from the myeloid stem cell.
In order for a lymphoid stem cell to develop into mature T and B lymphocytes, it must go through a series of successive divisions. First, lymphoblasts are formed from a lymphoid stem cell, which then give rise to 2 types of cells - T-lymphocyte precursors and B-lymphocyte precursors. As cells divide, they become more mature and specialized. The last stages of lymphocyte maturation no longer take place in the bone marrow, but in the lymphoid organs: the thymus, lymph nodes and spleen. As a result, mature T and B lymphocytes are formed.
Lymphocytes are essentially immune cells. This means that they are involved in the recognition and destruction of foreign bodies (viruses, bacteria) or pathologically altered tissues of one’s own body (for example, tumor cells). T and B lymphocytes do this differently. B lymphocytes fight foreign cells (antigens) with the help of immunoglobulins - proteins that bind antigens and trigger the process of their destruction by special proteins. T lymphocytes recognize antigens, destroy them independently or in interaction with other blood cells, and activate the production of immunoglobulins by B lymphocytes.
In lymphocytic leukemia, the formation of lymphocytes is disrupted. A large number of immature cells appear that are not able to do their job. This leads to serious immune failures. A person becomes more susceptible to infectious diseases such as tuberculosis and candidiasis. Serious complications from routine vaccinations can occur. So-called autoimmune reactions often appear - that is, the immune system fights normal cells of the body, such as red blood cells. The result is anemia.
Malignant lymphocytes penetrate the lymph nodes and spleen, causing them to enlarge, and can damage the liver, lungs, brain, and bones.
In acute lymphocytic leukemia, lymphoblasts predominate in the bone marrow. They divide very quickly, displace other cells from the bone marrow and blood, and actively populate the lymph nodes and spleen. The most common are acute B-cell leukemias, which produce a large number of immature B-lymphocytes. Acute B-cell leukemia is the most common type of leukemia among children.
In chronic lymphocytic leukemia, more mature forms of lymphocytes are found in the blood, which are able to perform their functions for some time. This type of leukemia is typical for people over 50-55 years old.
Who is at risk?
In case of acute lymphocytic leukemia at risk:
- people exposed to radioactive radiation,
- people who have undergone chemotherapy or radiation therapy for another form of cancer,
- patients with Down syndrome and other genetic disorders,
- people whose siblings have been diagnosed with acute lymphocytic leukemia.
In case of chronic lymphocytic leukemia at risk:
- representatives of the Caucasian race,
- people over 60 years old,
- people whose relatives have had cases of leukemia.
Diagnostics
- Complete blood count (without leukocyte formula and ESR) with leukocyte formula. This study provides the doctor with information about the quantity, ratio and degree of maturity of blood elements.
- Leukocytes. In acute lymphocytic leukemia, leukocytes may be increased, normal, or decreased. The leukocyte formula (the ratio of individual types of leukocytes) is determined from a blood smear. To do this, a thin smear is applied to a glass slide, stained with special dyes, and then examined under a microscope. In this way, the doctor can not only determine the ratio of leukocytes, but also identify pathological, immature cells that differ in appearance from normal ones. In acute lymphocytic leukemia, lymphocytes of varying degrees of maturity can be found in the blood - from lymphoblasts to mature cells.
- In chronic lymphocytic leukemia, lymphoblasts are usually absent. A characteristic sign of chronic leukemia is the detection of Botkin-Gumprecht cells (or shadows). They are the remains of destroyed limata
Diagnosis of chronic lymphocytic leukemia
The diagnosis of chronic lymphocytic leukemia can be suspected when assessing the results of a routine clinical blood test - an increase in the absolute number of lymphocytes and leukocytes attracts attention. The main diagnostic criterion is the absolute number of lymphocytes, exceeding 5 × 10 9 \l and progressively increasing as lymphocytic leukemia develops, reaching numbers of 100-500 × 10 9 \ l. It is important to pay attention not only to the absolute number - if at the beginning of the disease lymphocytes make up up to 60-70% of the total number of leukocytes, then with its further development they can make up 95-99%. Other blood parameters, such as hemoglobin and platelets, may be normal, but as the disease progresses, they may decrease. The absolute criterion for establishing a diagnosis of chronic lymphocytic leukemia is the detection of more than 5000 clonal B lymphocytes in 1 μl of peripheral blood.
A biochemical blood test may reveal a decrease in total protein and the amount of immunoglobulins, but this is typical for later stages of the disease. A mandatory step in the diagnostic search is a bone marrow biopsy. Histological examination of the obtained punctate in the early stages of the disease, as well as in a general blood test, reveals a small content of lymphocytes (40–50%), but with high leukocytosis, lymphocytes can make up 95–98% of the bone marrow elements.
Since changes in the bone marrow are nonspecific, the final diagnosis of chronic lymphocytic leukemia is established on the basis of immunohistochemical studies. The characteristic immunophenotype of chronic lymphocytic leukemia includes the expression of antigens CD19, CD5, CD20, CD23; there is also weak expression on the cell surface of immunoglobulins IgM (often simultaneously with IgD) and antigens CD20 and CD22. The main cytogenetic marker that directly influences the choice of therapy is the 17p deletion. It is advisable to perform an analysis aimed at identifying this deletion before starting treatment, since its identification leads to a change in patient management tactics. In addition to a bone marrow biopsy, in the case of significant enlargement of individual lymph nodes, puncture of them is indicated in order to exclude lymphoma.
Instrumental diagnostic methods include chest x-ray and ultrasound of the most commonly affected groups of lymph nodes and abdominal organs - primarily the liver and spleen, since these organs are most often affected by chronic lymphocytic leukemia.

Chronic lymphocytic leukemia
At the initial stage, the pathology is asymptomatic and can only be detected by blood tests. Over the course of several months or years, a patient with chronic lymphocytic leukemia exhibits lymphocytosis of 40-50%. The number of leukocytes is close to the upper limit of normal. In the normal state, peripheral and visceral lymph nodes are not enlarged. During infectious diseases, lymph nodes may temporarily enlarge, and after recovery they may decrease again. The first sign of progression of chronic lymphocytic leukemia is a stable enlargement of lymph nodes, often in combination with hepatomegaly and splenomegaly.
First, the cervical and axillary lymph nodes are affected, then the nodes in the mediastinum and abdominal cavity, then in the groin area. Palpation reveals mobile, painless, densely elastic formations that are not fused to the skin and nearby tissues. The diameter of nodes in chronic lymphocytic leukemia can range from 0.5 to 5 or more centimeters. Large peripheral lymph nodes may bulge with the formation of a visible cosmetic defect. With a significant enlargement of the liver, spleen and visceral lymph nodes, compression of the internal organs may be observed, accompanied by various functional disorders.
Patients with chronic lymphocytic leukemia complain of weakness, unreasonable fatigue and decreased ability to work. Blood tests show an increase in lymphocytosis to 80-90%. The number of red blood cells and platelets usually remains within normal limits; some patients exhibit slight thrombocytopenia. In the later stages of chronic lymphocytic leukemia, weight loss, night sweats and an increase in temperature to low-grade levels are noted. Immune disorders are characteristic. Patients often suffer from colds, cystitis and urethritis. There is a tendency for wounds to suppurate and frequent formation of ulcers in the subcutaneous fatty tissue.
The cause of death in chronic lymphocytic leukemia is often severe infectious diseases. Inflammation of the lungs is possible, accompanied by collapse of lung tissue and severe ventilation disturbances. Some patients develop exudative pleurisy, which may be complicated by rupture or compression of the thoracic lymphatic duct. Another common manifestation of advanced chronic lymphocytic leukemia is herpes zoster, which in severe cases becomes generalized, affecting the entire surface of the skin and sometimes the mucous membranes. Similar lesions can be observed with herpes and chickenpox.
Stages of the disease
Currently, staging is carried out according to the classification proposed by Binet:
- A - hemoglobin content more than 100 g\l, platelets - more than 100 × 10 9\l, less than three lymphatic areas are affected (these include: cervical lymph nodes, axillary lymph nodes, inguinal lymph nodes, liver, spleen),
- B - hemoglobin content more than 100 g\l, platelets - more than 100 × 10 9\l, more than three lymphatic areas are affected,
- C - hemoglobin content less than 100 g\ or platelets - less than 100 × 10 9\l.
In addition to the Binet classification, the Rai classification is used, mainly used in the USA. According to it, there are four stages of the disease:
- 0 - clinical manifestations include only an increase in lymphocytes of more than 15 × 10 9 in the peripheral blood and more than 40% in the bone marrow,
- I - the number of lymphocytes is increased, enlarged lymph nodes are diagnosed,
- II - the number of lymphocytes is increased, an enlargement of the liver and/or spleen is diagnosed, regardless of the enlargement of the lymph nodes,
- III - there is an increase in the number of lymphocytes and a decrease in hemoglobin level of less than 110 g/l, regardless of the enlargement of the spleen, liver and lymph nodes,
- IV - there is an increase in the number of lymphocytes and a decrease in the number of platelets less than 100 × 10 9, regardless of the level of hemoglobin, enlargement of organs and lymph nodes.
Stage 0 is characterized by a favorable prognosis, stage I and II - intermediate, stage III and IV - unfavorable.
General analysis
It is one of the basic tests required when visiting many specialists.
General analysis among specialists may also be referred to as “clinical”, or bear the abbreviation KLA. It is a whole set of tests aimed at determining both the quantity and parameters (size, etc.) of various blood cells.
The test allows blood sampling from both a vein and a finger (capillary).
Indications for use, preparation for the study
This is one of the most common laboratory tests performed to assess the general health of a patient. Prescribed for routine medical examinations, preparation for surgery, and included in the medical commission.
Symptoms for which a doctor may prescribe OAC: complaints of fatigue, weakness, apathy, signs of an infectious disease or inflammation, and elevated body temperature. A timely test allows you to diagnose and promptly treat a whole range of serious diseases.
The results of your analysis will be as reliable as possible if, before taking it, you:
- the day before your visit to the clinic, exclude alcohol and medications from your diet (in consultation with your doctor);
- You will not take it for 8 hours before the test (you can drink still water);
- Half an hour before donating blood, it is advisable not to overexert yourself physically and emotionally. Try not to smoke either.
General blood test indicators
The blood test includes a number of parameters. First of all, this is the calculation of the number of red blood cells (oxygen transport), leukocytes (ensure the fight against bacteria and viruses), platelets (blood clotting) per microliter or liter of blood. This also includes other indicators that describe the shape, volume and other characteristics of the cells being studied.
The basic table with blood sampling results includes:
- hemoglobin level
- hematocrit
- average red blood cell volume
- average hemoglobin content in an erythrocyte
- average hemoglobin concentration in erythrocytes
- platelets
- white blood cell count
- red blood cell count
In addition to basic indicators, the doctor may prescribe a leukocyte formula (the ratio of different forms of leukocytes as a percentage) and a calculation of the erythrocyte sedimentation rate (ESR). Professionals call such a comprehensive study a “clinical blood test.”
Treatment
Currently, chronic lymphocytic leukemia is highly treatable thanks to a wide range of chemotherapy drugs. It is important to note that current guidelines do not recommend starting aggressive treatment immediately after diagnosis - in cases where clinical manifestations are minimal, active follow-up is possible until indications for specific treatment arise, which include:
- The emergence or increase of intoxication, which is manifested by a loss of body weight by more than 10% over six months, a deterioration in general condition; the appearance of fever, low-grade fever, night sweats.
- Increasing symptoms of anemia and/or thrombocytopenia;
- Autoimmune anemia and/or thrombocytopenia - if the condition is not corrected with prednisone;
- Significant size of the spleen - the lower edge is at a distance of >6 cm or more below the costal arch;
- The size of the affected lymph nodes is more than 10 cm or its progressive increase;
- Increase in the number of lymphocytes by more than 50% in 2 months, or doubled in 6 months.
The main treatment method for chronic lymphocytic leukemia at the moment is chemotherapy. One of the first chemotherapeutic agents that showed its effectiveness in the treatment of chronic lymphocytic leukemia, chlorambucil, is still used today, albeit to a limited extent. Over time, cyclophosphamide has been used instead of chlorambucil, in combination with other drugs, and appropriate regimens (eg, CHOP, COP, CAP) are currently used in young patients with good physical status.
First introduced into clinical practice in the 80s of the last century, fludarabine showed effectiveness in achieving stable remission, exceeding the effectiveness of chlorambucil, especially in combination with cyclophosphamide. It is important to note that this regimen is effective even in the event of a relapse of the disease. The last word in the treatment of chronic leukemia is currently the use of immunotherapeutic agents - drugs from the group of monoclonal bodies. Rituximab has become firmly established in routine clinical practice. This drug interacts with the CD20 antigen, which is limitedly expressed in chronic lymphocytic leukemia, so effective treatment requires a combination of rituximab with one of the accepted chemotherapy regimens, most often with fludarabine or COP. Rituximab alone can be used as maintenance therapy in case of partial response to treatment.
The use of the drug alemtuzumab, which interacts with the CD52 antigen, looks promising. It is also used both alone and in combination with fludarabine.
Separately, I would like to mention chronic lymphocytic leukemia with 17p deletion. This subtype of lymphocytic leukemia is often resistant to standard chemotherapy regimens.
Some success in the treatment of this subtype of lymphocytic leukemia has been achieved through the use of the above-mentioned alemtuzumab. In addition, ibrutinib is a promising drug in this situation. Currently, this drug is used in monotherapy; its combination with various chemotherapy regimens is being studied; A regimen including ibrutinib, another monoclonal body, rituximab, and bendamustine, showed a certain advantage.
Radiation therapy, which a century ago was practically the only treatment option for such patients, has not lost its relevance to this day: it is recommended that it be carried out as part of an integrated approach to the area of the affected lymph nodes if their continued growth is observed against the background of stabilization of other manifestations of the disease. In this case, the required total dose is 20-30 Gy. Also, the radiation method can be used for relapses of the disease.
In the treatment of chronic lymphocytic leukemia, a surgical method has also found its place, which consists in removing the affected spleen. Indications for this intervention are:
- Enlarged spleen in combination with severe anemia and/or thrombocytopenia, especially if chemoresistance is observed,
- Massive enlargement of the spleen in the absence of response to chemotherapy,
- Severe autoimmune anemia and/or thrombocytopenia with resistance to drug treatment.
If resistance to previously used chemotherapy agents develops or if there is rapid progression after treatment, bone marrow transplantation may be performed. Bone marrow transplantation is indicated in first remission for high-risk patients, young patients in the absence of treatment effect, and patients with 17p deletion/TP53 mutation in the presence of disease progression. It is important to note that after transplantation, the use of rituximab and lenalidomide as maintenance therapy is recommended to prevent relapse.
Finally, patients require maintenance therapy, which includes:
- Transfusion of red blood cells for anemia;
- Platelet transfusion for bleeding caused by thrombocytopenia;
- Antimicrobial agents in case of bacterial, fungal or viral infection, as well as for its prevention;
- Use of prednisolone at a dose of 1-2 mg/kg in the development of autoimmune processes.
In the event of a relapse of the disease, treatment tactics depend on a number of factors, such as: previously administered therapy, the timing of the relapse, and the clinical picture. In case of early (that is, occurring within 24 months or earlier) relapse, the main drug is ibrutinib. It is used both independently and as part of the above-mentioned treatment regimen (ibrutinib + rituximab + bendamustine).
Alemtuzumab may be an alternative drug of choice. While demonstrating comparable efficacy to ibrutinib, it, however, exhibits significantly greater toxicity.
Finally, in some patients, bone marrow transplantation can be performed for early relapse of chronic lymphocytic leukemia.
In case of late relapse (occurring more than 24 months after completion of treatment), the main selection criterion is the early therapy performed.
- If previous fludarabine-based therapy was not accompanied by significant toxicity, then you can return to this regimen and also supplement it with rituximab.
- If cytopenia is detected, it is possible to use rituximab in combination with high doses of glucocorticosteroids.
- In case of previous treatment with chlorambucil, the use of regimens with fludarabine or a combination of bendamustine and rituximab is indicated.
- Monotherapy with ibrutinib or its combination with one of the polychemotherapy regimens can also be effective in relapsed chronic lymphocytic leukemia.
Evaluation of treatment effectiveness
Diagnostic studies aimed at assessing the effect of the treatment are carried out no earlier than 2 months after the end of the last course of chemotherapy. The result can be assessed as follows:
- Complete remission: reduction to normal sizes of the liver, spleen, lymph nodes (their increase in size of no more than 1.5 cm is acceptable), reduction in the number of lymphocytes to less than 4 × 10 9 \l in the peripheral blood and less than 30% in the bone marrow, increase in the number platelets more than 100×10 9 \l, hemoglobin - more than 110 g/l, neutrophils - more than 1.54 × 10 9 \l.
- Partial remission: reduction in the size of the lymph nodes, liver and spleen by 50% or more, reduction in the number of lymphocytes in the peripheral blood by 50%, increase in the number of platelets more than 100×10 9 \l, hemoglobin - more than 110 g/l, neutrophils - more than 1, 54×10 9 \l or an increase in any of these parameters by more than 50% from the initial level.
- Signs of disease progression are, on the contrary, an increase in the size of the lymph nodes, liver and spleen by 50% or more, as well as a decrease in the number of platelets by 50% or more from the initial level and a decrease in the number of platelets by 20 g/l or more.
To establish complete remission, it is necessary to meet all of the listed criteria; partial - at least 2 criteria relating to the condition of internal organs, and at least one criterion relating to the cellular composition of the blood.
It should be taken into account that ibrutinib therapy can lead to a complete response in the lymph nodes and spleen, but with preservation of leukocytosis in the peripheral blood. This condition is referred to as partial response with lymphocytosis.
Forecast
Significant advances in the treatment of chronic lymphocytic leukemia have made it possible to make this disease potentially curable or to support a person’s life for a sufficiently long time without progression of the underlying disease while maintaining its quality.
On the contrary, without treatment, the disease slowly but steadily progresses, which can cause the death of the patient several years after the onset of the disease, so timely consultation with a doctor and initiation of adequate therapy are very important.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Clinical recommendations for examination and treatment of patients with chronic lymphocytic leukemia. Recommendations of the National Society of Hematology. 2014.
- Volkova M.A. Chronic lymphocytic leukemia and its treatment. Attending doctor. 2007, No. 4.
- Michael Hallek. Chronic lymphocytic leukemia. Oncohematology. 2010, volume 3, no. 1. pp. 181-182.
- Fedorov A.B. B-cell chronic lymphocytic leukemia. Clinical oncohematology. Basic research and clinical practice. 2008. P.275-277.
- Fiyya A.T., Frenkel B.I. Chronic lymphocytic leukemia: diagnosis and treatment. Journal of Grodno State Medical University. 2011. No. 4. P. 93-97.
- Nikitin E.A. Ibrutinib in the treatment of chronic lymphocytic leukemia. Clinical oncohematology. 2021. 10(3), p. 282-286.
- Kravchenko D.V., Svirnovsky A.I. Chronic lymphocytic leukemia: clinical picture, diagnosis, treatment. Practical guide for doctors. Gomel, 2021.