An inguinal hernia is a pathological condition in which complete or partial protrusion of the abdominal organs occurs through weakened tissue of the inguinal canal.
- Classification
- Causes of inguinal hernia in men
- Diagnosis of the disease
- How to prepare for inguinal hernia removal
- Preparation immediately before surgery
- Indications and contraindications for surgery
- Information about the types of operations to remove hernias and their features
- Laparoscopic surgery
- Treatment without surgery
- Postoperative period
- Possible complications
- Forecast
Classification
Depending on the period of occurrence, congenital and acquired inguinal hernias are distinguished. Congenital hernias occur when the testicle descends from the abdominal cavity into the scrotum. Normally, at the end of this process, fusion of the gonadal layer of the peritoneum should occur, which will cover the inguinal canal. If this does not happen, a defect is formed through which internal organs can lobby. Acquired hernias form throughout life due to thinning or weakening of the muscular aponeurotic apparatus under the influence of provoking factors.
The second classification is based on the anatomical features of the hernia. Here they highlight:
- Indirect hernias - the entrance gate is the internal inguinal ring. In this case, the hernial sac is located next to the spermatic cord.
- Direct hernias - the hernial orifice is the medial fossa located opposite the external inguinal ring. Neither the inguinal canal nor the spermatic cord are affected.
- Combined hernias. This is a complex formation, which includes both oblique and direct hernias, but they do not communicate with each other.
Why do they arise?
There are areas of potential weakness in the abdominal wall. The areas where hernias most often develop are the navel, groin areas, and where there has been an incision in the abdominal wall (after surgery).
In male patients, blood vessels and the spermatic cord pass through the inguinal rings. This creates a weak area where an inguinal hernia can develop. Tension of the abdominal muscles (heavy lifting, chronic coughing, constipation) can enlarge this weak spot and force the abdominal organs to protrude through it under the skin, leading to the development of a hernia. Inguinal hernias can also occur in women, although less frequently. The round ligament of the uterus passes through the inguinal rings.
Other causes include incisions from old surgeries, which can weaken the abdominal wall if they do not heal properly. The strength of the muscle wall deteriorates with age, as well as with low physical activity.
Causes of inguinal hernia in men
In adult men, the formation of inguinal hernias is facilitated by the anatomical features of the inguinal canal - it is wider, shorter and not as well strengthened by muscles and tendons as in women. However, anatomical features alone are not enough; provoking factors are also needed:
- Age-related changes that lead to weakening of muscle tone and connective tissue structures.
- Systemic diseases leading to disruption of muscle function.
- Frequent increase in intra-abdominal pressure. This condition is typical for constipation, chronic cough, obesity, etc.
The insidiousness of intervertebral hernia
An intervertebral hernia is a pathological protrusion of part of the fibrous ring. In the vast majority of cases, it forms in the lumbar spine, somewhat less often in the cervical, and only sometimes in the thoracic.
It is not able to regress on its own, and even complex, extremely well-chosen conservative therapy does not always lead to significant positive changes. Over time, the hernial formation increases and can:
- compress the nerve roots, which causes severe pain, and subsequently leads to paresis - loss of motor ability of the upper or lower extremities;
- provoke strokes at a young age;
- cause severe disruption of the functioning of the intestines and pelvic organs, which is accompanied by uncontrolled separation of urine and stool.
Often, a spinal hernia is formed against the background of osteochondrosis, which today affects more than 90% of the Russian population, i.e., almost every person of working age. Progressive degenerative changes provoke the formation of a minor hernia, which is easiest to treat. But since at this stage the disease does not manifest itself in any way, it often remains undiagnosed until pronounced symptoms appear.
According to a recent experiment, out of 100 randomly selected people, 30 were found to have mild or moderate disc herniation. At the same time, almost none of the subjects even admitted the thought of its presence, although many admitted that they regularly experienced pain in the lower back and neck.
Diagnosis of the disease
Diagnosis of the disease is made on the basis of complaints, physical examination data and instrumental research methods.
Complaints
The main complaint with an inguinal hernia is a tumor-like formation in the inguinal fold, which increases with straining and disappears (or at least decreases) in the supine position. Periodically, a dull aching pain of varying degrees of intensity occurs in this place, which can radiate to the sacrum.

Physical examination
Physical examination is carried out in two positions - horizontal and vertical. At the same time, the size of the formation, its pain, shape, as well as the possibility of reduction are assessed.
Instrumental diagnostics
For differential diagnosis, herniography and ultrasound examination are performed. If necessary, additional research methods are prescribed.
How to prepare for inguinal hernia removal
To prepare for inguinal hernia repair, it is necessary to undergo a standard examination, which is carried out for all surgical interventions. This includes:
- General clinical tests - blood, urine, biochemistry.
- Blood test for infections - syphilis, HIV, hepatitis B and C.
- Coagulogram is an analysis that reflects the functioning of the blood clotting system.
- Determination of blood group and Rh factor.
- Blood pressure measurement.
- Chest fluorography (not older than one year).
- ECG.
In addition, as part of the preoperative examination, irrigoscopy, examination by a gynecologist, cystoscopy, and computed tomography may be prescribed according to indications. As a rule, such an extensive diagnosis is required for large hernias involving the internal organs of the small pelvis.
Are traditional techniques no longer needed?
The availability of minimally invasive laparoscopic techniques does not mean a complete abandonment of traditional surgical approaches in herniology. Sometimes an open access operation may be more preferable (see contraindications to laparoscopic hernioplasty), and technically such operations are an order of magnitude higher.
But behind TAPP, TEP and other laparoscopic treatment methods there is, if not the present, then definitely the future.
Bibliography
- Egiev V.N. Atlas of operative surgery of hernias./Egiev V.N., Lyadov K.V., Voskresensky P.K. // MEDPRACTIKA-M, 2003. - 109 p.
- Protasov A.V. Practical aspects of modern hernioplasty / A.V. Protasov, D.Yu. Bogdanov, R.Kh. Magomadov. - M.: RUSAKI, 2011. - 207 p.
- Features of preoperative examination of hernia patients / A.V. Fedoseev [etc.] // Science of the Young -ERUDITIO JUVENIUM. - 2014. - No. 1. - pp. 81-85.
- Complications and recurrences associated with laparoscopic repair of groin hernias. A multi-institutional retrospective analysis / C. Tetik // Surg Endosc. — 1994. — No. 1316. — 22 p.
- Schmedt CG Comparison of endoscopic procedures vs Lichtenstein and other open mesh techniques for inguinal hernia repair: a meta-analysis of randomized controlled trials / CG Schmedt, S. Sauerland, R. Bittner // SurgEndosc. -2005. — No. 188. — 99 p.
- Transabdominal pre-peritoneal (TAPP) vs totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair / BL Wake // Cochrane Database Syst Rev. — 2005. -No. 4703. — 43 p.
Preparation immediately before surgery
In patients with large hernias, displacement of internal organs is often observed. When they are adjusted, the level of intra-abdominal pressure changes, which can affect the activity of the cardiovascular and respiratory systems. To prepare the patient for such changes in advance, it is recommended to reduce the hernia (if possible) with the application of a compression bandage for several hours. This will allow it to adapt to changing conditions.
On the eve of the operation, it is necessary to shave the hair in the groin and pubic area. Colon cleansing is also carried out. On the day of surgery, you should not drink or eat.
Book a consultation 24 hours a day
+7+7+78
Indications and contraindications for surgery
The indication for planned removal of inguinal hernias is an uncomplicated disease. When choosing a surgical technique, the patient’s condition, age and medical history are taken into account. Risks must be assessed.
Planned surgery may be denied in the following cases:
- Giant inguinal hernias in patients over 70 years of age with decompensated disorders of the cardiovascular system.
- Liver cirrhosis, complicated by ascites, enlarged spleen, dilated esophageal veins.
- Decompensated diabetes mellitus.
- Inguinal hernias that occurred after palliative operations, for example, in the treatment of malignant neoplasms.
Emergency operations are performed when there is a threat to the patient's life. For example, if a hernia is strangulated or intestinal obstruction occurs as a result of it. There are no contraindications as such in this case, even if the patient’s condition is serious or he is very advanced in age, when the risk of complications is quite high.
Information about the types of operations to remove hernias and their features
All currently available methods for removing hernias involve the following steps:
- An incision is made at the site of protrusion of the hernial sac.
- Repositioning of internal organs into the abdominal cavity.
- Plastic surgery of hernial orifices.
The last point is key, since it is what should prevent relapse of the disease. All types of hernia repair are divided into two large groups:
Tension hernioplasty - the hernia gate is sutured with its own tissues. In this case, the inguinal canal narrows to a normal size - 0.6-0.8 cm. The disadvantage of this operation is the high risk of relapses, long-term pain in the postoperative period and rather long rehabilitation. In this regard, in economically developed countries this method is practically not used, with the exception of the treatment of children under 16 years of age.

Tension-free hernioplasty - artificial implants are used to strengthen the hernial orifice (as a rule, they have the form of a mesh made of inert synthetic materials). The implant not only takes on the load that occurs when pressure increases, but also strengthens the tissues, preventing them from stretching and the reverse formation of a hernial protrusion. The use of implants allows you to preserve the anatomy of the inguinal canal and avoid tissue tension. This will ensure an easier recovery period.
Modern methods of surgical treatment of hernias of the anterior abdominal wall
Surgery is an art, and, as such, it most of all requires creativity and least of all tolerates a pattern.
Vikenty Vikentievich Veresaev, doctor and writer
Modern approaches to surgical treatment of hernias of the anterior abdominal wall should implement the following principles as much as possible:
The reliability of the operation is to operate in such a way that the hernia does not occur again. It is based on the principle of stitching tissue without tension and using prosthetic techniques.
Less traumatic - the less tissue traumatization during surgery, the less surgical trauma - less pain, less need to stay in the hospital, less time to spend on recovery, faster you can get back to work and the normal rhythm of life. All this is achieved using modern minimally invasive, endoscopic techniques using modern low-traumatic methods of tissue fixation, reducing the time of the operation itself.
The safety of the operation is directly related to the use of modern approaches and techniques in the treatment of hernias, the use of biocompatible materials - modern composite implants, as well as the preparedness of surgeons and anesthesiologists performing this operation.
Functionality is the achievement of surgical restoration of the physiological function of the anterior abdominal wall, which can significantly improve the patient’s quality of life.
Aesthetics – restoration and improvement of the contours of the anterior abdominal wall, using modern approaches and principles of plastic and minimally invasive surgery.
All these requirements are met by the surgical techniques and modern materials I use in the treatment of hernias of varying locations and degrees of complexity.
Method of preperitoneal repair of inguinal and femoral hernia ONSTEP.
This method is a minimally invasive and tension-free version of surgical intervention, which is performed through a small incision (3-4 cm) remote from the main nerves, reducing the risk of long-term postoperative pain. Special “self-expanding” Onflex or PolySoft implants are used, installed preperitoneally and partially intramuscularly, which allows you to reliably close all potentially “weak” areas of the groin area and prevent the further development of other hernias in this area. In addition, fixation of the implant with sutures is not required, which reduces damage to the patient’s tissues and reduces the time of the operation itself. This technique is an alternative to laparoscopic hernioplasty.
The technique has proven itself well in the surgical treatment of recurrent inguinal hernias, including those arising after repair with mesh implants.
Photos of the stages of inguinal hernia repair using the ONSTEP method.
Advantages of the technique:
- Minimal, unnoticeable incision. (cosmetic effect).
- Possibility of quick recovery, shorter and less painful postoperative period.
- Possibility of use for surgical interventions for recurrent inguinal and femoral hernias.
Photos of patients after hernia repair using the ONSTEP method.
The use of self-fixing implants ADHESIX (Adgesix) in the treatment of inguinal hernias.
A special feature of the use of this type of implant is its ability to self-fix (glue) to tissues. In these implants, a biocompatible “self-adhesive” gel is applied to macroporous lightweight polypropylene, providing quick, easy and reliable fixation of the implant without the use of additional fixing sutures. This significantly reduces the amount of “surgical trauma” during surgery, which is very important for some groups of patients (for example, those taking anticoagulant therapy for pathologies of the cardiovascular system, patients who have had a heart attack and thrombophlebitis). Reducing tissue damage significantly reduces postoperative pain.

View of the Adhesix implant before installation

View of the posterior wall of the inguinal canal with the Adgesix implant installed)
Inguinal hernia repair using the Lichtenstein method using the self-fixing Adhesix implant from Bard.
About 25% of all operations for hernias of the anterior abdominal wall are operations for postoperative ventral hernias and primary ventral hernias with large hernial orifices. In all these cases, the edges of the hernia defect cannot be compared without tension.
Solutions to this problem exist today.
- Bridging
- Separation of the components of the anterior abdominal wall
- Temporary chemical denervation
Bridging (English: Bridge) is a device designed to combine segments.
Such a device, as a rule, is an implant that covers the defect and creates an additional supporting “frame” in the area of its installation. This refers to plastic surgery of the defect without covering it with aponeurotic tissue. These techniques are used mainly in cases where it is impossible or dangerous to reduce the edges of the hernial orifice due to the possibility of developing cardiopulmonary complications associated with a decrease in the volume of the abdominal cavity. The location of the implant can be different in relation to the layers of the anterior abdominal wall and depends on its quality characteristics, the method and complexity of its installation.
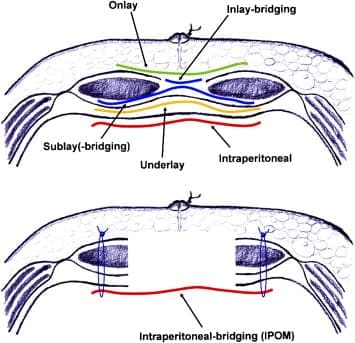
“inlay-bridging” – provides for the placement of the implant over the hernial orifice without suturing the edges of the aponeurosis.
“sublay-bridging” – the implant is located under the aponeurosis or under the muscles.
“intrapreritoneal (IPOM) – bridging” – the implant is located preperitoneally.
Intraperitoneal repair of ventral hernias using composite implants Ventralex, VentralexST, Ventrio, VentrioST.
Currently, taking into account the understanding of the mechanisms of integration of modern implantation systems in human tissue, special attention is paid to the spatial arrangement of the implant and the optimally simple, safe method of its installation.
The IPOM (intraperitoneal onlay mesh) hernia repair technique is an intraperitoneal position of the implant in the area of the hernial orifice directly on the peritoneum, that is, “inside the abdomen.”
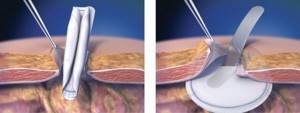
With this installation method, the implant is pressed against the anterior abdominal wall due to intra-abdominal pressure. In this case, you can get by with its rare fixation in the area of unchanged tissues or even not use it. There is no contact of the implant with subcutaneous fat, which eliminates the negative impact on the course of the wound process and allows you to avoid complications associated with the development of inflammatory reactions.
Installation of the implant can be performed through an incision (usually minimal) - open IPOM technique, or through separate punctures on the abdominal wall using laparoscopic technologies - closed IPOM technique. One of the options for the closed IPOM technique is the IPOM plus , in which the defect is eliminated using special transfascial sutures, and then an implant is installed.
The Ventralex implant from Bard (USA), which is a self-expanding, non-absorbable sterile prosthesis, consisting of a top layer of polypropylene mesh and a layer of ePTFE (stretched polytetrafluoethylene) with microscopic pores, which helps to minimize tissue adhesion, has proven well in practical use. VentralexST implants have a resorbable anti-adhesion barrier based on Sepra® Technology hydrogel applied to the inner surface.
Straightening and fixation of the endoprosthesis is carried out using an elastic ring integrated into the implant with shape memory, thanks to which during the operation there is no need to straighten the device after insertion, as well as fix it (with a thread or herniostapler), which significantly reduces the duration of the operation. This also affects the patient’s feelings after surgery - discomfort and pain are minor and pass relatively quickly.
The “memory ring” keeps the implant in a tensioned position, which prevents it from shrinking over time, thereby eliminating the possibility of relapse. The implant does not migrate while in the body.
Photos of the stages of hernia repair using the Ventralex implant
The use of Ventralex composite implants is effective, safe and technically simple. It makes it possible to reliably perform hernioplasty for umbilical and small ventral hernias and to close postoperative defects with a diameter of up to 8 cm. Moreover, it is possible to install them “through a puncture” using endoscopic or minimally invasive technology.
Hernia repair using the open intraperitoneal (IPOM intraperitoneal onlay mesh) technique for an umbilical hernia using the Ventralex composite implant.
Ventrio and Ventrio ST implants are used to close large defects (more than 8 cm), which usually arise after abdominal surgery or after recurrence of previously operated hernias. They are also equipped with shape memory rings and special positioning “pockets” to facilitate their installation. All of them are created using modern composite biocompatible materials, which make it possible to solve serious reconstructive problems of the anatomical integrity of the anterior abdominal wall with the restoration of its function without the use of complex combined traumatic interventions that produce a large number of relapses.
Hernia repair using the open intraperitoneal (IPOM intraperitoneal onlay mesh) technique for a ventral hernia using the Ventrio composite implant.
I have accumulated extensive experience in using these operations and modern implants in the treatment of patients who are overweight, with diseases that reduce the reparative ability of tissues (diabetes mellitus, autoimmune diseases, oncopathology), the possibility of closing “complex” defects in lateral hernias, including hernias arising after placement of intestinal ostomies.
The practical application of low-traumatic technologies for installing these implants has proven to ensure reliable fixation of the endoprosthesis to the tissues of the anterior abdominal wall, avoids postoperative complications and relapses, and quickly restores daily activity and quality of life of patients.
Closed intraperitoneal repair (IPOM) of postoperative ventral hernias using implants with the ECHO PS positioning system.
The essence of this operation is that the intervention takes place without the use of traditional incisions. Everything is performed through small punctures on the anterior abdominal wall, and all adhesions caused by previous interventions are separated with minimal tissue damage. And most importantly: the hernia defect is closed from the inside with the Ventralight ST ECHO PS implant (Ventralite ST) from the American company Bard, coated with a special layer of hydrogel, which minimizes the formation of adhesions and adhesions. The implant is equipped with a special positioning system ECHO PS. This is a system of microtubules, which, when filled with air, unfolds the implant in the abdomen and allows it to be tightly aligned with the tissues from the inside. The implant is fixed using the SorbaFix hernia stapler, with special clips, which then completely dissolve. Upon completion of the installation and fastening of the implant, the “tubes” are deflated and then quickly and completely removed from the abdomen.
This technology helps maintain optimal implant deployment, eliminating some of the challenges of placement and positioning within the abdominal cavity, especially for larger defects. Simplifies the process of using an effective and high-tech method of treating hernias.
For the first time such an operation in the Samara region was performed by the author of this article on February 20, 2021.
Endoscopic surgery using the IPOM plus method using the Ventralight ST ECHO PS implant (Ventralite Sepra Technology ECHO PS) with a self-positioning system in the treatment of postoperative recurrent ventral hernia.
Separation plastic surgery of the anterior abdominal wall.
Based on the technique of separating the muscular-fascial components of the abdominal wall to increase the volume of the abdominal cavity. This allows suturing even large defects of the abdominal wall without tension, without provoking an intra-abdominal increase in pressure and the occurrence of abdominal compartment syndrome (small abdominal volume syndrome).
In this case, the division of the components of the abdominal wall into layers and the displacement of these layers relative to each other is carried out mostly in the so-called “sacred” layer (holyplane), located between the transverse and preperitoneal fascia. It is the junction of two embryonic layers and does not contain any vessels. A modern implant (Ventralight, BardSoftMesh...) is installed in the space between the layers.
There are several options for separation plastics:
The anterior option is plastic surgery according to the method of O.M. Ramirez.
Rear options: – plastic surgery using the AMCarbonell method;
– plastic surgery using the NWNovitsky method (TAR plastic surgery).
Indications for such an operation are: large hernias in which more than 20% of the internal organs are located outside the abdominal cavity, the so-called “loss of domain” situation, as well as hernia defects of more than 10 cm, when it is impossible to suture the posterior layers of the rectus abdominis sheath without tension.
The method makes it possible to eliminate hernias in several locations at once in one operation from one access without interaction with the abdominal organs.
Separation abdominal wall plasty is a modern and effective technology in the treatment of patients with large ventral and postoperative hernias.
The disadvantage of this technique is, to one degree or another, a violation of the biomechanics of the anterior abdominal wall.
Photos of the patient before and after reconstructive plastic surgery for a recurrent postoperative lateral ventral hernia using the separation technique and the use of the VentraLight ST implant.
Temporary chemical denervation
In the English-language literature, we can find this concept under the term “chemical separation of the components of the anterior abdominal wall.”
The technique is based on the use of botulinum toxin type A in preoperative preparation.
Botulinum toxin is injected into the muscles of the anterior abdominal wall under ultrasound control before surgery 1.5 months before surgery. Under its action, the muscles of the anterior abdominal wall relax, resulting in an increase in muscle length. This allows you to use implantation technology without bridging and not resort to separation plastics, reduce the size of the integrated implant and prevent the development of abdominal hypertension (small belly syndrome). Removing spasm and muscle contracture helps reduce the load on this implant and gives time for the formation of a reliable aponeurotic scar due to the prolonged action of botulinum toxin (4-6 months).
The accumulated significant experience in surgical interventions for hernias of the anterior abdominal wall using modern prosthetic materials and surgical technologies makes it possible to most effectively resolve issues regarding the surgical treatment of this pathology with the possibility of performing other combined and corrective operations.

Always ready to help you!
Laparoscopic surgery
Laparoscopic surgery is a relatively new, minimally invasive method for removing an inguinal hernia. All manipulations are performed through several small punctures. This minimizes tissue damage. Accordingly, the patient experiences less pain and discomfort in the postoperative period. Working capacity is restored literally within a couple of days. During this intervention, a special technique is used: a laparoscope, which provides an overview of the surgical field, and trocars with miniature instruments, with the help of which the hernial protrusion is eliminated, a mesh implant is installed and fixed.
How is laparoscopic hernioplasty performed?
Laparoscopic tension-free hernioplasty is the latest method of hernia repair, with minimal trauma to the abdominal tissue.
The surgeon makes three to four punctures (no more than 1 cm in diameter) in the anterior abdominal wall, through which he inserts microsurgical instruments equipped with optics. The camera transmits a multiply enlarged image to the monitor, ensuring precise precision of each instrument movement. The doctor moves parts of the internal organs located in the hernial sac, returning them to their normal position. The next stage is closing the hernial orifice with a mesh implant, which is fixed with a special herniostapler, preventing the endoprosthesis from moving.
Laparoscopic tension-free hernioplasty is performed under general anesthesia. The latest generation endoscopic equipment allows you to make precise cuts of any depth. Removal of the hernial sac and damaged tissue takes a few minutes, after which the area of the hernial orifice is closed with a surgical mesh. For large hernias, a combination of open hernioplasty (at the stage of isolation and excision of the hernial sac) and endoscopic installation of a surgical mesh is possible.
A characteristic feature of laparoscopic hernioplasty is the almost complete absence of postoperative pain and the fastest healing of tissues, which makes this technique one of the most effective in the practice of treating hernias.
Postoperative period
Features of the operating period will vary for each type of hernioplasty. The longest and most painful stage of recovery after removal using the tension method. The period of incapacity for work can reach several weeks. Laparoscopic surgery is the easiest to tolerate because it involves a minimum of tissue intervention. Recovery after it occurs within several days.
Regardless of how the operation is performed, at first it is necessary to refrain from physical activity, especially those that lead to increased pressure in the abdominal cavity. It is also recommended to adjust your diet to avoid constipation. You can return to work and resume physical activity only after consulting a doctor.
Rehabilitation
The rehabilitation period when performing minimally invasive operations takes the shortest possible time. Within 1 day, the patient is in the clinic, where observation, wound dressing and anesthesia are carried out if necessary. Within 2 weeks (physical activity, thermal procedures, sexual activity are limited), complete recovery occurs.
Open operations require a longer (up to 1 month) recovery period. The patient remains in the medical center for up to 3 days for observation and dressings.
Forecast
If left untreated, an inguinal hernia will inevitably progress and become more complicated. Therefore, it is recommended to undergo surgery, and the earlier the operation is performed (there are no pronounced changes in the soft tissues yet), the greater the chances of a radical cure without subsequent relapses.
However, in any case, to avoid the problem returning, it is recommended to follow simple recommendations:
- Maintain a normal weight.
- Avoid heavy lifting.
- It is also necessary, if possible, to cure diseases that lead to a constant increase in intra-abdominal pressure, for example, chronic cough, impaired urine outflow, constipation, etc.
Book a consultation 24 hours a day
+7+7+78
What do we treat
In the surgical department of GMS Hospital, laparoscopic hernioplasty is used to treat:
- Inguinal hernia
- Femoral hernia
- Hiatal hernia
- Umbilical hernias
- Spigelian line hernias
- Postoperative hernias
- Hernia of the white line of the abdomen
- Diastasis of the rectus abdominis muscles
Endoscopic hernia repair with mesh provides excellent cosmetic results, and the patient can return to normal life in just 2 weeks.
Western standards of treatment (evidence-based medicine)
Continuous staff development
Regular interaction with leading Russian and foreign medical institutions
Modern medical equipment and advanced diagnostic and treatment methods
Unified standard of service
We work around the clock 24/7/365
Make an appointment We will be happy to answer any questions Coordinator Oksana










