Why is the research being conducted?
Lipids are complex organic substances. In the human body they perform very important functions:
⦁ are an element of cell membranes; ⦁ serve as a powerful molecular source of energy; ⦁ participate in the synthesis of many hormones, vitamins, biologically active substances; ⦁ transport fat-soluble vitamins and medicinal substances.
Also, the indicator may increase during pregnancy, menopause, with alcohol intoxication, taking diuretics, hormonal drugs, corticosteroids, vitamin D2, and the predominance of cholesterol-rich foods in the diet - eggs, fatty meats.
Low values of the indicator may be the result of liver pathologies, severe acute inflammatory processes, malabsorption syndrome, and a lack of animal products in the diet.
Lipoproteins
Since cholesterol is insoluble in water, it is not able to “travel” throughout the body on its own. Its transport between organs and tissues is carried out by lipoproteins.
Lipoproteins are a complex of fatty acids and other lipids with proteins albumin or blood serum globulins
. Four types of these complex protein-lipid compounds can be found in the blood, but the most significant indicators of the lipid profile are high-density lipoproteins (HDL) and low-density lipoproteins (LDL), which in the popular literature are called “good” and “bad” cholesterol.
⦁ HDL - high-density lipoproteins (“good” cholesterol).
The main function of HDL is the transport of cholesterol from the cells of peripheral organs, blood vessels, and lymphatic vessels to the liver, where it is transformed into cholic acids and excreted from the body. HDL removes excess cholesterol from the body, thereby preventing the formation of atherosclerotic plaques in blood vessels. In this regard, a sufficient level of the indicator is considered as a factor that reduces the likelihood of atherosclerosis and heart pathologies.
Reference values of the indicator are 0.91-1.56 mmol/l. When assessing the likelihood of developing cardiovascular disease, a value of > 1.0 mmol/L in men and > 1.2 mmol/L in women indicates a low risk.
⦁ LDL - low-density lipoproteins (“bad” cholesterol).
Complex proteins that are the main carriers of cholesterol into tissues. It is LDL that delivers endogenous and exogenous cholesterol to the cells of organs and tissues, and elevated levels of these substances cause the formation of atherosclerotic plaques in blood vessels. In this regard, a high concentration of LDL in the blood is a more reliable marker of the development of atherosclerosis, myocardial infarction, and stroke than an increased level of total cholesterol in the blood. Reference values of the indicator are 0-4.12 mmol/l.
Lipid profile indicators. How to take the test correctly and what affects the result?
Laboratory diagnostics doctor of the clinical diagnostic laboratory Kapustina E.V.
When going for any research or analysis, we all want to get the correct and most reliable result, and in the case of a lipidogram , as with other analyses, you need to know and follow some rules so as not to distort the indicators.
The blood lipid spectrum is very sensitive to external conditions. This doesn't just apply to food intake. The results can be affected by anxiety, excessive exercise, taking medications, having recently had other tests, drinking alcohol the night before the test, infections, etc., so all these factors need to be kept in mind.
It is recommended to take blood samples for lipid levels in the morning, on an empty stomach, at least 12-14 hours after the last meal. Half an hour before the test, you should exclude physical activity and psycho-emotional experiences, as well as smoking.
Before drawing blood, you must maintain your normal diet for 2 weeks.
Key lipid profile indicators:
- Total cholesterol (TC)
- Triglycerides (neutral fat) (TG)
- High-density lipoprotein cholesterol (HDL-cholesterol, or HDL-cholesterol)
- Low-density lipoprotein cholesterol (LDL-cholesterol, or LDL-cholesterol)
- Very low density lipoprotein cholesterol (VLDL-C)
- Atherogenic coefficient (AC)
- Apolipoproteins (apo-A, apo-B)
How to decipher the analysis?
Many people know that cholesterol is the most important indicator of fat metabolism, so its increase is always a cause for concern. However, this indicator alone is not enough for correct conclusions, because cholesterol can increase in absolutely healthy individuals without provoking atherosclerosis. At the same time, normal and low cholesterol levels do not always indicate well-being. To assess fat metabolism, it is important to establish the ratio of individual lipid fractions, the fluctuations of which are more characteristic of pathology or normality.
Cholesterol “travels” through blood vessels not alone, but in combination with proteins, forming globules (balls) of different sizes and densities, which are called lipoproteins . The proteins found in lipoproteins are called apolipoproteins . The more protein a lipoprotein contains, the higher its density. Hence, high-density lipoproteins (HDL), intermediate-density lipoproteins (LDL), low-density lipoproteins (LDL), and very low-density lipoproteins (VLDL), as well as chylomicrons (CM) are isolated. Chylomicrons are formed in the intestinal wall, they transport neutral fat (triglycerides) obtained from food. Cholesterol and lipoproteins are formed in the liver and perform different tasks.
Cholesterol is an integral component of cell membranes; it is part of bile, necessary for proper digestion, and is a precursor of sex hormones, without which development, puberty and functioning of the adult body do not occur.
But on the other hand, cholesterol can cause various troubles:
One of the main negative features of cholesterol is its direct participation in the formation of atherosclerotic plaques on the walls of arterial vessels. This “task” is performed by the so-called atherogenic cholesterols in low and very low density lipoproteins (LDL and VLDL), which account for 2/3 of the total amount of cholesterol in the blood plasma. They are endowed with the ability to “stick” to the walls of blood vessels and participate in the formation of cholesterol plaque with subsequent narrowing of the lumen of the vessel. True, anti-atherogenic high-density lipoproteins (HDL), which protect the vascular wall, try to counteract “bad” cholesterol, but there are 2 times less of them (1/3 of the total).
The level of cholesterol in the blood should not exceed 5.2 mmol/l, however, even a concentration value approaching 5.0 cannot give complete confidence that everything is fine in a person, since the content of total cholesterol is not an absolutely reliable sign of well-being. Therefore, it is important to determine the ratio of atherogenic (VLDL and LDL) and antiatherogenic (HDL) lipoproteins, which more subtly reflects the state of lipid metabolism and the course of atherosclerosis.
Low-density lipoprotein cholesterol (LDL-cholesterol, or LDL-cholesterol) in a healthy person makes up 60-65% of the total and does not exceed 3.5 mmol/l. In those who have already been affected by atherosclerosis, LDL-C values may increase markedly, that is, this indicator is more informative regarding atherosclerosis than the level of total cholesterol in the blood.
Normally, high-density lipoprotein cholesterol (HDL cholesterol or HDL cholesterol) in women should be greater than 1.2 mmol/l (in men the lower limit is different – 1.0 mmol/l). If the level of HDL cholesterol becomes less than acceptable values, they cannot fully protect the blood vessels. The number of HDL particles increases with exercise in the fresh air.
Triglycerides are important as a source of energy. They are carried in very low density lipoproteins and chylomicrons. Their number increases sharply after eating fatty foods.
It has been established that TGs increase with atherosclerosis, diabetes mellitus, excess weight, hypertension and play an important role in the development of coronary heart disease and vascular changes in the brain.
An indicator such as atherogenicity coefficient , which indicates the degree of development of the atherosclerotic process, but is not the main diagnostic criterion, is calculated mathematically using special formulas; its normal values range from 2-3.
The atherogenicity coefficient can also serve as a prognostic indicator. If it is below three, then the risk of atherosclerosis and vascular lesions is minimized. A coefficient level of 3-4 may indicate an increased risk of atherosclerosis, and with a value of 5 or higher, patients usually already have certain manifestations of atherosclerosis - coronary heart disease, cerebrovascular accident, kidney pathology, impaired blood flow in the extremities. With such numbers, vascular complications are quite likely.
Apolipoproteins are relatively new, modern indicators of lipid metabolism; they complement the main indicators of the lipid profile. ApoB is found in low-density lipoproteins and increases the atherogenic properties of the blood. ApoA is associated with high-density lipoproteins and increases their antiatherogenicity.
When deciphering a lipid profile in adults, the doctor assesses whether there are deviations in the numbers of specific indicators. It is believed that the risk of atherosclerosis is increased if total cholesterol, LDL-C, VLDL-C, apoB and TG exceed normal values. Pathology is also indicated by an atherogenic coefficient of more than three and a reduced content of high-density lipoproteins (HDL-C) and apoA.
In addition, low cholesterol levels are just as undesirable as high ones (if this is not associated with taking lipid-lowering drugs); it may indicate various pathologies: anemia, liver disease, increased thyroid function and even cancer.
The values of lipid spectrum indicators are considered optimal:
Total cholesterol – 3.1-5.2 mmol/l
Triglycerides up to 1.7 mmol/l;
HDL cholesterol – 1.03-1.55 mmol/l
LDL cholesterol - 2.32 -3.5 mmol/l
Atherogenic coefficient – 2 -3.0;
If a person is diagnosed with hypercholesterolemia (increased cholesterol levels), then it is customary to assess its degree:
- cholesterol level 5.2-6.2 mmol/l is considered borderline high
- 6.2-7.5 mmol/l – moderate hypercholesterolemia
- >7.8 mmol/l - severe hypercholesterolemia
Every adult over 20 years of age should know their cholesterol level and regularly, at least once a year, it is recommended to determine total cholesterol, and every 5 years to perform a complete study of the lipid spectrum
Some reasons for high cholesterol levels:
- poor nutrition;
- sedentary lifestyle;
- obesity;
- smoking,
- alcohol abuse;
- diabetes;
- arterial hypertension;
- liver diseases;
- hypothyroidism;
- hereditary disorder of lipid metabolism.
Atherogenic coefficient
A numerical value that reflects the degree of cholesterol metabolism disorder, i.e. an indicator reflecting the balance between the level of atherogenic and antiatherogenic lipids
. The atherogenic coefficient is determined using a special formula ⇊
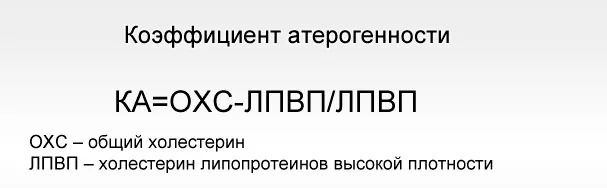
It is considered normal if the indicator is < 3.0-3.5.
Higher values indicate a higher risk of developing cardiovascular pathologies.
Relevance of the analysis
Specialists in our department prescribe a lipid profile if the following diseases are suspected:
- Atherosclerosis;
- Coronary vascular disease;
- Myocardial infarction;
- IHD (coronary heart disease);
- Vascular pathologies of the brain.
The study is prescribed for both diagnostic and preventive purposes, especially for patients at risk.
Fats are present in the blood of any person in certain concentrations. They are deposited in tissues and participate in metabolic processes that ensure the normal functioning of the body. Disorders of fat metabolism, such as increased cholesterol levels, can lead to the development of pathological processes. The main ones are atherosclerosis, ischemia, heart attacks and strokes.
The test may be part of a routine medical examination. Our specialists prescribe it to patients who are at risk according to certain criteria. If imbalances in fat levels are detected, your doctor may prescribe preventive therapy. It includes lifestyle correction - normalization and stabilization of body weight, diet, and physical exercise. In some situations, medications are prescribed.
Why do some people develop these diseases and others not?
In medicine there is a concept of risk. Risk is a group of factors whose presence increases the likelihood of developing a particular disease in each individual person. Cardiovascular risk factors include high blood pressure; diabetes; smoking; having close relatives who have suffered a heart attack or stroke; age over 55 years for women and 60 years for men; gender – after all, women under 50 years of age are protected from atherosclerosis by female sex hormones; disturbance in the blood lipid profile. As well as certain dietary habits: overeating, heavy consumption of food at night, increased content of the so-called. “bad” lipids or trans fats in the daily diet, consumption of sugar-sweetened drinks.
Every man over 40 years of age and every woman over 50 years of age should be examined by a doctor once a year to assess the presence of cardiovascular risk factors. Tables have been developed for such an assessment. Residents of our country, as well as the entire post-Soviet space, are assessed according to tables developed for countries with high cardiovascular risk. This is due to the great influence of sociocultural factors on cardiovascular mortality. To assess risk, gender, age, systolic blood pressure, total blood cholesterol level and smoking are taken into account.
You cannot change your gender or age, humanity dreams of learning how to influence heredity in the future, but today you can take control of other important risk factors for cardiovascular diseases. One such controllable factor is normal blood lipid levels.