What you need to know about the infection?
Syphilis is a sexually transmitted disease known since ancient times. The incubation period is considered to be the period from infection to the formation of chancre. Its average duration is considered to be 21 days, although in practice there are known options of 10 and 90 days.
The most common method of infection is sexual. The infection is also transmitted:
- due to contact with blood - its traces on a razor, syringe, manicure accessories;
- in utero from mother to fetus;
- household method (minimum percentage of infection).
In international medical practice, specialists use the categories of congenital, early, late syphilis, and its unspecified forms. In specialized literature, authors operate with the concepts of primary, secondary, tertiary and latent syphilis:
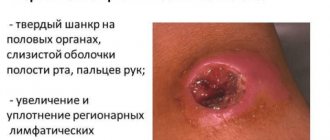
- Primary syphilis is the period from the formation of a hard chancre (ulcer) at the point of penetration of the bacterium (usually on the genitals) to a rash on the skin. At this time, the lymph nodes usually become enlarged. The chancre disappears within 2-6 weeks. At this stage of the disease, there are no antibodies to syphilis in the patient’s blood, so the test does not detect infection.
- Secondary syphilis is a stage of the disease that begins 4-8 weeks after the appearance of chancre. The patient feels a general malaise, his body temperature rises, a headache occurs, and a characteristic rash appears on the skin. Symptoms may vary in severity.
- The latent form of the disease may be asymptomatic. Signs of syphilis disappear, but since the pathogen is still in the body, relapses in an acute form are possible. If the patient is not treated, severe systemic damage to the skin, bones, joints, nervous and cardiovascular systems should be expected.
The likelihood of infection with syphilis increases in the presence of other infections transmitted through sexual contact - chlamydia, genital herpes, papillomavirus. The risk of infection during anal sexual intercourse, especially if there is damage to the mucous membranes, is significantly higher than during protected vaginal sex.
A sick person can infect a healthy person at any stage of the disease. The most dangerous are primary and secondary syphilis, when the dermis and mucous membranes suffer from active manifestations of the disease. The bacterium Treponema pallidum enters the body through microscopic damage to the skin and mucous membranes. Soon it affects the lymphatic system, then all organs, found in saliva, semen, and breast milk.
Late forms of syphilis: current state of the problem
Syphilis occupies an important place in the structure of sexually transmitted infections (STIs) and is a socially significant disease, since it not only causes great damage to the health and reproductive function of the patient, but also poses a threat to the economic and social potential of the country [1–7]. 1990s in the Russian Federation were marked by a real epidemic of syphilis, comparable in terms of indicators only to the distant pre-penicillin era. Currently, the situation has stabilized, however, against the backdrop of a constant decrease in overall morbidity, there is a noticeable upward trend in the number of patients with late forms [1, 8–10]. In the Republic of Tatarstan, the proportion of patients with late syphilis increased from 1991 to 2014 by 120 times.
In late forms of syphilis, the few treponema pallidum preserved in the tissues gradually lose their antigenic properties and the leading role passes to the reactions of cellular immunity. Against the background of a decrease in humoral immunity, the intensity of the humoral response decreases and the number of specific antibodies decreases, which is accompanied by the negativity of serological tests, primarily non-treponemal tests, of which the microprecipitation reaction (MPR) is currently used [8, 11–13]. Our analysis of the incidence of late syphilis from 1991 to 2013. (901 patients) found that most of these patients (68.8%) were identified in the period from 2005 to 2014 after the introduction in 2005 of serological testing using enzyme-linked immunosorbent assay (ELISA) and passive hemagglutination test (RPHA). At the same time, the MCI result of the observed patients was negative in 65.7% of cases. Almost all patients were infected during the syphilis epidemic in the 90s. XX century. The lengthening of the diagnostic route in the vast majority of cases was caused by antibiotic therapy, the reasons for which were prescribed were quite diverse. In 5.0% of cases, patients received preventive treatment in the past (always with durable penicillin drugs) as contacts of syphilis, in 7.3% they were treated for other STIs, in 13.4% they self-medicated or turned to medical professionals, in 17.8% - antibiotics were prescribed as therapy for intercurrent diseases. 22.8% had previously suffered syphilis, of which 85.0% of patients received treatment with durant drugs. And finally, a small part (4.1%) was observed by dermatovenerologists with a diagnosis of “false-positive serological reactions.” Only a third (29.6%) of patients had never had syphilis or been treated with antibiotics before they were diagnosed with a late form of syphilitic infection. It is noteworthy that before the diagnosis was made, a third of the patients in the observed group (35.6%) were tested using MRP methods and a complex of serological reactions (SSR) from once in a lifetime to several times a year with a negative result.
According to our data, of all clinical variants of late syphilis, the latent form currently prevails (83.0%). Late syphilis with symptoms most often manifests itself as damage to the nervous (13.6%) and cardiovascular (2.7%) systems. Late lesions of the nervous system are mainly diagnosed as a pathological process in the blood vessels of the brain, which is accompanied by epileptoid seizures, sensory and speech disorders, and ischemic strokes. Proliferative changes and gummas in the tissue of the brain or spinal cord occur in episodes. Cardiovascular late syphilis is often defined as uncomplicated syphilitic aortitis or syphilitic aortitis complicated by stenosis of the coronary artery ostia and aortic valve insufficiency.
Patients diagnosed with “other symptoms of late syphilis” or the more familiar terminology “tertiary syphilis” are now extremely rare. Tertiary syphilis (syphilis III tertiaria), called by A. Fournier “the most unfortunate station where the most important and severe manifestations of the disease occur,” at the end of the 19th century occupied 59.4–87.0% of all its forms [4, 9, 14]. In 1911, its share in Russian cities was 29.6%, in villages - 55.9%, in 1921 - from 33.0 to 77.0% in various regions of the RSFSR [1]. After the introduction of arsenic drugs into the arsenal of antisyphilitic therapy, and then antibiotics, the registration of the tertiary form began to decrease noticeably in the 70–80s. last century accounted for only 3.2% of the total incidence of syphilis [4, 9, 15]. Currently, tertiary syphilides are rare, since treatment with penicillin in early forms prevents the post-epidemic increase in later manifestations. No less significant reasons for the decline are active dispensary work and mass screening events carried out in the USSR after the outbreak of syphilitic infection in the 1970s, as well as the widespread and uncontrolled use of antibiotics by the population [4, 15–17]. In the Russian Federation, 5 cases of gummous syphilis were diagnosed in 2007, and none in 2008. However, after the introduction of durable penicillin drugs into practice, an increase in late forms with clinical symptoms is expected, as has already been reported in the domestic and foreign literature. The return of gummous syphilis, tabes dorsalis and progressive paralysis can also be caused by the association of Treponema pallidum with pathogens of other STIs, especially with the human immunodeficiency virus (HIV), which is confirmed by N. S. Potekaev (2004), who observed an HIV-infected patient with diffuse gummous meningoencephalitis [10, 18–22]. In the Republic of Tatarstan, the last registration of the gummous form was in 1960. However, in 2009, 2 cases of this clinical variant of the infection were diagnosed.
Clinical manifestations of late syphilis are destructive lesions of the skin, bones, joints, internal organs and nervous system (Fig. 1–3). The human psyche also changes significantly. Patients become “strange”, suffer from mental instability, and may experience hallucinatory delusions [1, 14, 20]. On the skin and mucous membranes, syphilides appear as tubercles or gummas. Lesions of the musculoskeletal system are severe and are accompanied by destructive changes, mainly in the bones of the legs, skull, sternum, clavicle, ulna, nasal bones, etc. Late syphilis of the bones manifests itself in the form of osteoperiostitis or osteomyelitis. Osteoperiostitis can be limited and diffuse. Limited osteoperiostitis develops more often and is a gumma, which in its development either ossifies or disintegrates and turns into a typical gummous ulcer. After some time, sequestration appears; less often, the bone gum becomes ossified. Healing ends with the formation of a deep retracted scar. Diffuse osteoperiostitis is a consequence of diffuse gummous infiltration. It usually ends with ossification with the formation of calluses. With diffuse gummous osteoperiostitis, the changes are similar to a limited process, but more widespread, in the form of a fusiform, tuberous thickening. They are especially noticeable in the middle part of the crest of the tibia and ulna. With osteomyelitis, the gumma either ossifies or a sequester forms in it. Patients complain of pain that worsens at night and when the affected bones are tapped. Sometimes sequestration leads to the development of a gummous ulcer. The process involves the periosteum, cortical, spongy and medulla with destruction of the central part of the lesion and the occurrence of reactive osteosclerosis along the periphery. Subsequently, the cortical layer of the bone, periosteum, and soft tissues are affected, a deep ulcer is formed, bone sequesters are released, the bone becomes fragile, and a pathological fracture may occur. The radiograph shows a combination of osteoporosis and osteosclerosis. Morphologically, productive necrotic inflammation is observed with the formation of tubercles, gummas (syphilitic granuloma) and gummous infiltrates. Gumma and tubercular syphilide are infectious granulomas, accompanied by pronounced changes in the blood vessels. Gumma is an extensive area of coagulative necrosis, the edges of which consist of large fibroblasts, reminiscent of epithelioid cells in tuberculosis. There is an inflammatory mononuclear infiltrate of plasma cells and a small number of lymphocytes around. Langhans giant cells are very rare. In gummous infiltrates, a typical picture is observed with the formation of perivascular inflammatory couplings. In vessels, especially large ones, proliferation of the endothelium is noted, up to their obliteration. Sometimes in the neighborhood there are microscopic granulomas, which in their structure are practically no different from tuberculous and sarcoid granulomas.
Verification of syphilitic organ damage in the late period presents certain difficulties, since clinical manifestations are scarce, and serological reactions are informative only in 65–70% of cases. In addition, doctors often make diagnostic errors, while patients receive a variety of treatments, including surgical ones, which are contraindicated for them and do not give the desired effect.
As an example, we give our own observation.
Patient L., born in 1967 (46 years old), single, promiscuous, alcohol abuser, in 2006 (7 years ago) consulted a local physician with complaints of weakness in the knee and elbow joints, headache, dizziness. At the local clinic, after carrying out the express examination for syphilis recommended by the standards, a positive result was obtained, and therefore the patient was sent to the regional dermatovenerological dispensary (DVT). Upon examination, no manifestations of syphilis were found on the skin and mucous membranes. At the same time, the patient had objective neurological symptoms, which did not attract the attention of a dermatovenerologist. A diagnosis was made: latent early syphilis, treatment was carried out with medium-duration penicillin (Bicillin-3). After completing the course of specific therapy, L. was under clinical and serological control for a year, which he interrupted on his own. Until the fall of 2013, I did not test for syphilis. Despite pronounced changes in the joints and nasal septum, he did not seek medical help. Only in September 2013, when applying for a job, was he examined serologically with a positive result of all tests (MRP 3+, ELISA Pol., RPGA 4+ from 09/06/13). Pre-hospital examination at the regional hospital allowed us to suspect late syphilitic damage to the nervous system and musculoskeletal system in L. The patient was hospitalized in the inpatient department of the hospital.
Upon admission: visible skin and mucous membranes are pale, without rashes. Peripheral lymph nodes are not enlarged. Facial muscles are hypotrophic. The range of motion in the cervical spine is sharply limited - head rotation in both directions is no more than 10 degrees. Movements in the shoulder, elbow and knee joints are severely limited, the joints are deformed and thickened. The muscles of the limbs are hypotrophic. Proprioreflexes are increased, d = s, except for the Achilles, which are decreased, d ≤ s, sensitivity is not changed.
Complete blood count: erythrocytes 2,190,000, hemoglobin 60 g/l, color index 0.82, leukocytes 7,600, eosinophils 1%, band leukocytes 2%, segmented leukocytes 80%, lymphocytes 12%, monocytes 5%, ESR 65 mm /h.
General urine test and biochemical blood test are within normal limits.
Serological examination: blood MCI 4+, ELISA positive, RPGA 4+; CSF MRP is negative, ELISA is positive, RPGA 4+, RIF-200 4+.
X-ray of the elbow and knee joints: on both sides - a sharp narrowing of the joint spaces, sclerosis and massive ecostoses of the articulated surfaces, gummous periostitis of the anterior surface of the ulna, destruction of the bone tissue of the humerus. Conclusion: syphilitic lesion of both elbow and knee joints (periostitis, osteomyelitis, arthritis).
Consultation with an ophthalmologist: retinosclerosis.
Consultation with an otorhinolaryngologist: extensive perforation of the nasal septum.
Consultation with a therapist: severe hypochromic anemia of unspecified origin.
Consultation with a neurologist: neurosyphilis with bulbar manifestations of pyramidal insufficiency.
Based on these data, a diagnosis was made: late neurosyphilis with symptoms A52.1.
Other symptoms of late syphilis (bone syphilis, gumma, synovial syphilis) A52.7.
The patient received 2 courses of specific therapy: benzylpenicillin sodium salt crystalline, 12 million units intravenously, 2 times a day, 20 days, break 2 weeks. During treatment, general health improved, headaches and joint weakness decreased.
This observation indicates that insufficient awareness of specialists about the clinical features of syphilitic infection in its late manifestations can have very dangerous consequences. It is especially depressing that the lengthening of the diagnostic route was due to the fault of the dermatovenerologist. The patient’s negative attitude towards his own health, possibly provoked by the disease, and the inadequate actions of the attending physician led to a severe, crippling outcome.
When determining the causes of damage to internal organs and the central nervous system, a correctly collected anamnesis is invaluable, which must include the following information.
- Syphilis suffered in the past.
- Any options for antibacterial therapy.
- Results of previous syphilis testing, if performed.
- Other past illnesses.
- Dispensary observation by specialists of other profiles.
- In women: the presence of inflammatory processes in the reproductive organ system; and the number and outcome of previous pregnancies.
- Typical complaints.
- Results of special studies and consultations of related specialists, if any.
Particular caution should be exercised in relation to patients under 40 years of age who have not recently suffered from any somatic diseases. We remind you that any clinical variant of late syphilitic infection is an indication for cerebrospinal fluid examination!
All of the above allows us to conclude: today the problem of syphilis remains as relevant as it was many centuries ago. Nowadays, the clinical manifestations of late syphilis are as diverse as in the pre-penicillin era. Underdiagnosis of late forms sometimes leads to quite severe and sometimes tragic consequences. It is noteworthy that many doctors continue to emphasize and verify syphilis only based on the results of serological tests. Insufficient awareness of specialists about the clinical features of syphilitic infection in its late manifestations makes it necessary to change the direction of organizational work with them, as well as more active intervention of dermatovenerologists in the diagnostic process. The introduction of serological methods such as ELISA and RPGA into laboratory examination makes it possible to optimize the diagnosis of syphilis not only in its early but also late manifestations. The increase in the incidence of latent, visceral forms, congenital and neurosyphilis indicates the undoubted relevance of the problem and determines the control of syphilitic infection as a priority in global health. Under these conditions, a scientifically based approach is needed to analyze the constantly changing situation of the spread of syphilitic infection in different age and professional groups and different regions.
Literature
- Dmitriev G. A., Dolya O. V., Vasilyeva T. I. Syphilis: phenomenon, evolution, innovation. M.: Binom. 2010. P. 367.
- Kubanova A. A., Lesnaya I. N., Kubanov A. A. et al. Development of a new strategy for controlling the spread of sexually transmitted infections in the Russian Federation // Bulletin of Dermatology and Venereology. 2009. No. 3. P. 4–12.
- Kubanova A. A., Melekhina L. E., Kubanov A. A. et al. Incidence of congenital syphilis in the Russian Federation for the period 2002–2012. // Bulletin of dermatology and venereology. 2013. No. 6. pp. 24–32.
- Milich M.V. Evolution of syphilis. M.: Medicine, 1987. 159 p.
- Chebotarev V.V. Syphilis. Monograph. Stavropol. 2010. P. 444.
- Department of Health and Human Services, Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines // MMWR. 2006. Vol 55. 94 p.
- Lewis DA, Young H. Syphilis // Sex Transm. Infect. 2006. 82 (Suppl IV). R. 13–15.
- Katunin G.L., Frigo N.V., Rotanov S.V. et al. Analysis of the incidence and quality of laboratory diagnostics of neurosyphilis in the Russian Federation // Bulletin of Dermatology and Venereology. 2011. No. 3. pp. 18–26.
- Mavlyutova G.I., Yusupova L.A. Damage to internal organs in early and late forms of syphilitic infection. Training manual for doctors. Kazan: Alfa-K LLC, 2014. 55 p.
- Moskvin I.P., Brzhozovskaya M.G., Lukina Yu.S. Gumma of the spine as a manifestation of tertiary syphilis // Bulletin of Dermatology and Venereology. 2007. No. 1. pp. 33–36.
- Runina A.V., Khairullin R.F., Rog K.V. et al. New recombinant antigens Treponema pallidum Tr0453 and Tr0319 in the diagnosis of syphilis // Bulletin of Dermatology and Venereology. 2014. No. 3. pp. 72–79.
- Frigo N.V., Manukyan T.E., Rotanov S.V. et al. Diagnosis of early forms of syphilis by immunochemiluminescence // Bulletin of Dermatology and Venereology. 2013. No. 3. pp. 66–73.
- Herring A., Ballard R., Mabey D., Peeling RW WHO/TDR Sexually Transmitted Diseases Diagnostics Initiative. Evaluation of rapid diagnostic tests: syphilis // Nat Rev Microbiol. 2006. 4 (12 Suppl). R. 33–40.
- Ge A.G. Course of venereal diseases. Kazan, 1903. 598 p.
- Mavlyutova G.I., Yusupova L.A., Minullin I.K. Practical aspects of the evolution of clinical markers of syphilitic infection. Training manual for doctors. Kazan: Medok, 2013. 36 p.
- Hama K., Ishigushi N., Tuji T. et al. Neurosyphilis with meziotemporal magnetic resonance imaging abnormalities // Intern med J. 2008. No. 47. R. 1813–1817.
- Young A., Mc Millan A. Syphilis and the endemic treponematoses. In: McMillan A., Young H., Ogilvie MM, Scott GR Clinical Practice In: Sexually Transmissible Infections. Elsevier Science Limited, London. 2002. R. 395–459
- Musher DM Syphilis, neurosiphilis, penicillin, and AIDS // J. Infect. Dis. 1991. V. 163 (6). P. 1201–1206.
- Norris SJ, Pope V., Johnson RE, Larsen SA Treponema and other human host-associated spirochetes. In Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, eds. Manual of Clinical Microbiology. Washington DC: American Society for Microbiology. 2003. R. 995-10-71.
- Parc S. E. Manifestations and treatment of ocular syphilis during an epidemic in France // Sex Transm Dis. 2007. V. 34, No. 8. P. 553–556.
- Young A., Mc Millan A. Syphilis and the endemic treponematoses. In: McMillan A., Young H., Ogilvie MM, Scott GR Clinical Practice In: Sexually Transmissible Infections. Elsevier Science Limited, London. 2002, pp. 395–459.
- Monteiro F., Julião B. Oral Manifestation of Tertiary Syphilis // Case Report. Braz. Dent. J. 1999. V. 10 (2). P. 117–121.
G. I. Mavlyutova1, Candidate of Medical Sciences L. A. Yusupova, Doctor of Medical Sciences, Professor A. G. Misbakhova, Candidate of Medical Sciences
GBOU DPO KSMA Ministry of Health of the Russian Federation, Kazan
1 Contact information
Description of the study
Serological tests are used to diagnose the disease. They are based on detecting antibodies in the patient’s blood. There are treponemal and non-treponemal tests.
Laboratory blood test "Syphilis RPR" refers to nonspecific antiphospholipid tests of the VDRL modification. RPR is a more modern version of the Wasserman reaction (RW), and is part of a group of non-treponemal screening tests. It detects IgG and IgM antibodies to lipoid, lipoprotein-like material released from damaged cells of a patient with syphilis. The RPR test, in accordance with the order of the Ministry of Health of the Russian Federation, is used for initial screening of patients and monitoring the process of treatment of syphilis.
Antibodies detected by laboratory blood tests are directed specifically against the bacterium Treponema pallidum. The study does not distinguish between the type of antibodies, but rather shows the overall response. They are present in 80% of patients with primary and almost 100% with early, latent and secondary syphilis. As a rule, a positive reaction to the test is detected 7-10 days after the formation of the primary chancre, that is, 3-5 weeks after the infection enters the human body.
The effectiveness of the RPR test is reduced in chronic patients. More than a third of cases of late syphilis are not diagnosed. The RPR titer reduced by 4 or more times within 1 year in treated patients indicates its effectiveness. After completion of therapy, the test is negative in 98-99 cases out of 100.
IMPORTANT:
A non-treponemal test may give a false positive result due to the presence of antibodies against cardiolipin in the blood caused by other diseases. A treponemal test can confirm or remove suspicion of syphilis.
Laboratory diagnosis of syphilis
KLD doctor of the highest category Zorich Anzhelika Anatolyevna
Antigenic structure of Treponema pallidum
The most studied antigens are:
— protein antigens of Treponema pallidum; contain a fraction common to pathogenic and non-pathogenic treponemas, in addition, there is a fraction specific only to pathogenic treponemas; antibodies against them appear in the body at the end of the incubation period or during the first week after the appearance of chancroid;
- antigens of polysaccharide nature; low immunogenic, because antibodies against them do not reach significant titers, so the role of these antibodies in the serodiagnosis of syphilis is insignificant;
— lipid antigens of Treponema pallidum; make up about 30% of the dry mass of the cell; in addition to Treponema pallidum lipids, a large number of substances of a lipid nature appear in the patient’s body as a result of the destruction of tissue cells, mainly mitochondrial membrane lipids; apparently, they have the same structure as the lipid antigens of Treponema pallidum and have the properties of autoantigens; Antibodies appear in the patient’s body approximately 5–6 weeks after infection.
Consequently, syphilitic antibodies can be nonspecific (reagin) and specific (antitreponemal). Reagins are directed against lipid antigens of Treponema pallidum and against autoantigens that arise as a result of the destruction of body cells. It should be borne in mind that reagins are also found in normal tissues, and their amount increases under various physiological and pathological conditions. These reagins may be the cause of so-called biological false-positive serological reactions to syphilis.
Specific antitreponema antibodies, related to IgM and IgG, are directed against Treponema pallidum and, like Treponema antigens, can be group-specific and species-specific.
To determine antibodies in a patient’s blood serum, various serological reactions are used, differing from each other in sensitivity, specificity, complexity and cost. Considering that all serological reactions to syphilis under certain conditions can be false positive, they should be performed in combination and, if necessary, in dynamics.
Serological reactions, depending on the antibodies they detect, are divided into groups:
— lipid (reagin) reactions, nonspecific, non-treponemal:
microreactions on glass with lipid antigens - an express diagnostic method (precipitation microreactions - MRP, VDRL, CMF, RPR, etc.); complement fixation reaction (FFR) with lipid antigens - Wasserman reaction; sedimentary reactions (Cahn precipitation reaction, cytocholic Sachs-Vitebsky reaction, etc.);
— group treponemal reactions, group and species-specific:
depend on the antigens included in the set: RSC with Reiter protein antigen; immunofluorescence reaction (RIF); immune adherence reaction (IAR); treponema pallidum immobilization reaction (TRI); RIF Abs. and its variants (IgM FTA ABS, 19S IgM FTA ABS, etc.); indirect hemagglutination reaction of Treponema pallidum (IPHA); immunoblot IgM, IgG.
Various serological reactions are used for various practical purposes. During mass surveys of the population and when emergency detection of syphilis is necessary, selection reactions (VDRL, RPR, MRP, etc.) are used. To diagnose (confirm) syphilis in cardiological, psychoneurological, ophthalmological patients, as well as pregnant women, the determination of total antibodies IgM, IgG in any immunological reaction (today - ELISA). In order to monitor the effectiveness of therapy, quantitative VDRL or determination of IgM in an immunological reaction (ELISA) is recommended. As an examination reaction in cases of discrepancy in treponemal reactions, IgM, IgG immunoblot is used. The immunoblot uses 5 separated antigens: p15, p17, p22, p45 and p47. Of these, 4 proteins are specific, p22 is nonspecific. Therefore, the presence of the p22 band is of fundamental importance and in some cases explains the presence of a false positive result. The presence of even one specific IgM band is regarded as a positive result, the presence of one specific IgG band is considered a doubtful result; a dynamic study and IgM immunoblot are recommended.
Direct treponemal tests
— dark-field microscopy: Treponema pallidum is poorly stained with traditional dyes, so a dark-field microscope is used. The material for research in primary syphilis is material from chancre, in secondary syphilis it is from erosive papules.
- PCR: - with primary syphilis, material from chancre can be examined, with secondary syphilis - from erosive papules. In early secondary syphilis, at the time of the first rash, DNA can be found in the venous blood. With a regular smear from the vagina, cervix, or urethra, the pale spirochete is not detected. This method is always recommended in case of negative dark-field microscopy data, taking systemic and local antibacterial and antiseptic drugs, or the presence of a mixed infection (especially herpes).
What is the dynamics of serological studies for syphilis?
Antilipid (nonspecific) antibodies are formed 7-14 days after chancre formation or 4-5 weeks after infection. Specific anti-treponemal IgM antibodies are detected at the end of the second week from the moment of infection. IgG to treponemal antigens appears approximately 4 weeks after exposure. Thus, by the time clinical symptoms of syphilis (formation of chancre) appear, both specific IgM and specific IgG (total antibodies) can be detected in the blood serum of patients. The parameters of the immune response may change as a result of treatment. Adequate treatment of early syphilis leads to a rapid decrease in titers of nonspecific antibodies and specific IgM, while specific IgG usually remains in the blood serum for a long period of time, and sometimes for life.
| RIBT floor | |||||||||||||||
| antitreponemal IgG sex. (ELISA, immunoblot) | |||||||||||||||
| antitreponemal IgM sex. (ELISA, immunoblot) | |||||||||||||||
| reagins (lgM + lgG) sex. MOP, RPR, VDRL | |||||||||||||||
| lymphadenitis | polyadenitis | ||||||||||||||
| inc. period | chancre | primary roseola | |||||||||||||
| weeks | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
False-positive serological reactions for syphilis
In cases of false-positive serological reactions, the blood serum of the examined people contains only reagins, but no specific antigens and antibodies.
The following groups of conditions are distinguished:
- infectious diseases, the causative agents of which are antigenically similar to treponema pallidum (relapsing fever, yaws, bejel, pinta, leptospirosis, inflammatory processes caused by treponema, saprophytic in the oral cavity and on the genitals);
-physiological and pathological conditions leading to changes in metabolism, especially lipid metabolism (pregnancy, gout, typhus, malaria, pneumonia, leprosy, endocarditis, diffuse connective tissue diseases, myocardial infarction, concussion, artificial immunization, cancer, lead poisoning, phosphorus, chloroform, taking sodium sacylate, digitalis, etc.);
— technical errors when setting up reactions.
There are acute and chronic false-positive reactions. Acute false-positive reactions are not persistent and their spontaneous negativity occurs within 4 to 6 months. Chronic reactions remain positive for more than 6 months.
The causes of acute biological false-positive reactions are pregnancy (especially in the last weeks and in the first 10 days after birth), pneumonia, in particular mycoplasma etiology, measles, enterovirus infection, infectious mononucleosis, vaccination, drug addiction, alcoholism. They are less commonly observed in active tuberculosis, scarlet fever, viral pneumonia, brucellosis, rickettsiosis, leptospirosis, measles, lymphogranuloma venereum, malaria, and protein starvation.
In patients who stop taking drugs, false-positive serological reactions to syphilis persist for up to 14 months. Sometimes the causes of nonspecific serological reactions are extensive trauma, concussion, fractures, myocardial infarction, as well as technical errors in the formulation of reactions.
Chronic false-positive standard serological reactions can be observed in patients with leprosy, systemic lupus erythematosus, Hashimoto's thyroiditis, rheumatism, periarteritis nodosa, liver cirrhosis, sarcoidosis, generalized scleroderma, cryoglobulin purpura, malignant tumors, malaria, tuberculosis, brucellosis, leptospirosis, infectious mononucleosis, diabetes mellitus , blood diseases, hypertension, chronic alcoholism and drug addiction. With age, the number of false positive results increases. In women they are observed 4.5 times more often than in men. Sometimes the causes of false-positive reactions remain unclear (idiopathic reactions) or they occur spontaneously in some families.
Nonspecific serological reactions average 0.03 - 2.5%. More often they are weakly positive, and if positive, then with a low titer of syphilitic reagins. In some diseases (lymphomas, chronic lymphocytic leukemia, rheumatoid arthritis, liver cancer), their titer, however, can be high. Upon repeated examination, nonspecific reactions become negative or their severity decreases, while the serum titer of patients with syphilis remains the same or increases.
With nonspecific results, discrepancies in several reactions are observed. Sometimes there is a discrepancy in the results of reactions when it is performed with different antigens: positive results are obtained with one antigen, negative results with another. In case of a sharp discrepancy, the study must be repeated with a new portion of blood, but not earlier than a week later. The most reliable criterion for true syphilitic indications of classical serological reactions is the result obtained from a blood test using an IgM, IgG immunoblot.
Features of diagnosing syphilis at Euromed
Nonspecific reagins are determined by the RPR test with cardiolipin antigen with the addition of carbon particles. Manufacturer: HUMAN, Germany.
Serological diagnosis of syphilis is carried out by immunochemiluminescence, in which total IgM and IgG antibodies to specific treponemal antigens p15, p17, p47 are determined - this is such a total mini immunoblot! The sensitivity and specificity of the test system is more than 99%. Manufacturer: ABBOT, Germany.
Indications for analysis
There are many reasons to get tested for syphilis. They are rented out:
- people with an active sex life, intimate relationships with several partners;
- after unprotected sexual intercourse or rape;
- in preparation for surgery;
- when obtaining a medical record and permission to work;
- pregnant women and women planning pregnancy;
- donors;
- when lesions appear on the skin and mucous membranes of the genital organs;
- with pathological mucous discharge from the vagina, urethra;
- if rashes appear on the skin, which are accompanied by enlarged lymph nodes, especially in the groin;
- for pain in joints and bones.
The described symptoms give the doctor reason to refer the patient for a blood test for syphilis to confirm or remove the diagnosis. The examination results also provide a more accurate diagnosis of patients with other infectious diseases.
Comparison with other methods of testing for syphilis
In clinical practice, for screening (preliminary) examination for syphilis, a study of RMP or an improved version (IPR) is performed.
If the data are positive, a confirmatory treponemal test is performed - ELISA, RPGA, RIT (RIBT), RIF:
- RMP . Non-treponemal rapid test that detects antibodies to treponema, turnaround time: 24 hours. The microprecipitation reaction allows the detection of primary and secondary syphilis. The indication for the study is the presence of symptoms of the disease (rash on the skin, ulcers on the genitals, enlarged lymph nodes). The reliability of the test is about 80%;
- RPR. A modern analogue of the classic Wasserman analysis, it detects the anticardiolipin type of antibodies. The plasma reagin reaction is a modification of RMP; the difference between them lies in the technological features of its implementation. Reliability of RPR - 70% (primary form), 98% (secondary form);
- ELISA . The enzyme-linked immunosorbent test detects immunoglobulins G and M and is used as a confirmatory or preliminary test for syphilis. Gives a positive result from 8-10 weeks of infection, helps to assess the duration of the disease in patients with a hidden, asymptomatic, atypical clinical picture, and select effective individual therapy. The reliability of ELISA is 97-98%;
- RPGA . The passive hemagglutination test is used to determine any form of syphilis. The diagnostic value of RPHA for early diagnosis is 87%, for 2-3 years - 98-99%;
- RIT(RIBT) . The immobilization reaction of Treponema pallidum is based on the process of immobilization of the pathogen in contact with the test serum. The test gives a positive result 3 months after infection. The technique is sensitive and reliable, but technically it presents certain difficulties - it requires special equipment and takes a long time to complete. Reliability is 100% for late, early, secondary syphilis, 90-93% for atypical forms;
- REEF. Allows the determination of class A antibodies, inferior to RIT in specificity. The immunofluorescence reaction gives (+) for latent/secondary syphilis, shows 95% reliability for congenital/tertiary syphilis.
The main advantage of the immunoblot compared to other tests is that the antigen-antibody response does not require expensive technology and depends on the mass of the protein.

The second advantage is that the result is not affected by the lack of solubility or instability of antigens.
The analysis makes it possible to determine the reaction of immunoglobulins with several antigens.
This has great diagnostic value, especially in complex cases.
The test is quite simple to perform; if necessary, it allows you to detect IgM and IgG in isolation from each other.
Objectives of the study
The test for syphilis is used:
- in the primary diagnosis of the disease;
- to assess the effectiveness of prescribed therapy;
- in examining women planning pregnancy to remove suspicions of a latent course of the disease;
- to test pregnant women, since even an infected woman treated before 4 months of pregnancy can still give birth to a healthy baby.
Intrauterine infection of the fetus usually occurs from a mother who has been suffering from syphilis for several months to three years. Pregnancy of a woman with syphilis can cause:
- stillbirth;
- late (12-16 weeks) miscarriage;
- congenital early and late syphilis in a baby.
Most often, fetal damage occurs in the 5th month of pregnancy or during passage through the infected birth canal. The signs of congenital early disease are similar to the symptoms of secondary syphilis. They are diagnosed in the delivery room. Symptoms of a secondary congenital disease are similar to tertiary syphilis. They are usually recognized by the age of 5-17 years. Hutchinson's triad is considered an indisputable indicator of a congenital disease. It includes labyrinthine deafness of the child, the presence of parenchymal keratitis, supplemented by Hutchinson's teeth.
Symptoms of syphilis
When the incubation period passes, the following stages of infection occur:
1.Primary.
2.Secondary early and late.
3.Tertiary.
An unspecified STD may present differently depending on the stage. The first signs of syphilis, which should be addressed by a specialist, include:
- the appearance of hard chancre on the mucous membranes, in particular on the genitals;
- enlarged lymph nodes in the area affected by STDs;
- change in the nature of discharge in women (thick, with an unpleasant odor);
- itching in the vagina in women.
As for men, if there are no other infections, there are no symptoms of acute infection. Only a red ulcer may appear on the penis, which does not cause pain. Next, let's look at the symptoms of each stage.
Decoding the results
Antibodies in the blood serve as a marker confirming the presence of infection in the body. Interpretation of laboratory test data for syphilis depends on the type and amount of antibodies detected. The interpretation of the test results is made by the attending physician.
- Reference indicators, that is, values in the normative range, mean a negative result.
- A negative result does not provide a clear answer. It is possible both in the absence of syphilis and when the infection period is too short, when there are still no antibodies in the blood.
- When a child is born to an infected mother, a negative test does not exclude congenital syphilis, since antibodies may not have yet formed.
- A positive test result from a patient who previously tested negative confirms that they were recently infected. A significant increase in indicators in paired analyzes taken at a weekly interval is also interpreted.
- Antibodies in a newborn's blood tests indicate congenital syphilis.
- A positive test is grounds to assume latent or possible tertiary syphilis.
In St. Petersburg, the Unified Medical Center offers testing for syphilis. Make an appointment by phone or via the Internet service. The price is indicated on the website.