Fluorography: essence, features, application
Fluorography is the simplest and most accessible screening method, which is used mainly for preventive examinations. It helps to identify:
- pathologies of the lungs, bronchi,
- tuberculosis,
- oncology in the chest area.
To conduct the study, a special apparatus with a fluorescent screen is used. X-rays are passed through the patient's chest. The image obtained due to the uneven absorption of rays by different tissues and organs is displayed on the screen and then photographed on film. The image is only 11x11 cm in size. It is then enlarged and examined by a radiologist, who makes a conclusion about the presence of pathologies.
The screen of a fluorographic apparatus is less sensitive compared to X-ray equipment, so the radiation dose for such an examination is higher. For example, when undergoing chest fluorography, the radiation dose is 0.8, and an x-ray of a diseased tooth can be taken with a beam of no more than 0.1 m3v. To avoid unnecessary exposure of the body, fluorography is recommended to be done only once a year.
The following categories of people should undergo fluorography every six months:
- patients with chronic diseases,
- people who have had tuberculosis (during the first 3 years),
- medical workers, teachers, educators, people employed in hazardous/harmful industries,
- persons with HIV,
- people living with pregnant women and newborn children,
- people released from prison (in the first 2 years).
Is X-ray examination of the OGK safe?
Trying to understand the difference between chest x-rays
and fluorography, it is worth knowing that in domestic clinics the radiation dose is several times higher than that permitted in more developed countries. The reason is that Russian clinics often use very old devices. In Europe, the annual dose of X-ray radiation is no more than 0.6 mSv, but in Russia it is more than twice as high - 1.5 mSv.
However, in the event of a threat to the patient’s life, for example from acute pneumonia, doctors will not have to choose whether to do a fluorography or an x-ray of the lungs; they will simply use the available equipment for a speedy diagnosis. Typically, in such a situation, an X-ray examination is performed directly and from the side, and often a targeted X-ray is also needed.
Radiography: main differences from fluorography
Classic radiography is carried out in a similar way - by illuminating a certain area of the body with X-rays. But unlike fluorography, this equipment does not have a fluorescent screen. The photograph is taken immediately in full size. Because of this, it turns out to be clearer and more detailed, which allows you to identify any pathological changes, determine the size, contours, localization of foci of inflammation, the presence of cavities and much more. Thus, it becomes clear that fluorography can always be replaced with x-rays , but it is very difficult to replace x-rays with fluorography.
Using X-ray equipment, you can examine not only the chest, but also other parts of the body. Such an examination is not carried out for preventive purposes; radiography is prescribed only if it is necessary to clarify or make the correct diagnosis.
It is not necessary to irradiate the entire person during the examination. Special protective aprons, collars, skirts, and caps with a lead layer reliably protect those parts of the body that do not need examination. This is especially important for children and other categories of patients.
At the KIT multidisciplinary medical center, we perform radiography using modern digital equipment . The radiation dose is minimal and similar to the dose you might receive from short periods of direct sunlight. Digital radiography is used to diagnose diseases and pathologies of the respiratory, cardiovascular systems, musculoskeletal system, as well as various injuries to the chest.
Digital X-rays are considered less dangerous to human health than examinations using film equipment or FLG. It is allowed to take x-rays several times a year if this is necessary to make a diagnosis and the radiation dose will not exceed the maximum permissible. Our specialists do not prescribe unnecessary procedures and carefully monitor compliance with safe standards.
How is an x-ray taken for pneumonia?
For pneumonia, an X-ray of the lungs is usually taken, regardless of the cause of the disease. Before the study, it is necessary to remove everything that could distort the results: metal objects, jewelry, long hair, etc. X-ray of the lungs
done in a vertical position, having first undressed to the waist and stood in front of the machine as the radiologist says. At the doctor’s command, the patient draws air into his lungs and holds his breath, while the device takes a picture.
Which is better: x-ray or fluorography?
Compared to digital radiography, fluorographic examination is considered simpler and cheaper, but at the same time an outdated screening method. Let us note the main differences between these 2 survey options:
- Accuracy. Fluorography is a superficial study. From such an image, the doctor can only determine the presence of pathology or signs of an advanced disease. An X-ray is more accurate and detailed. It allows you to get a clear picture of the current state of internal organs, bones, tissues, notice pathologies and diseases in the early stages of development, begin treatment faster, and record the dynamics of changes. For comparison, we note that the shadows on an x-ray image can be about 2 millimeters, while on a fluorographic image they occupy as much as 5 centimeters, which significantly complicates decoding.
- Radiation dose . Digital X-ray is safer for the patient, since the device operates with less radiation exposure. Especially considering that many public clinics still use old film FLG equipment.
- The area of fluorography examination is limited only to the chest, while x-rays are carried out in relation to almost any area of the body (limbs, head, teeth, etc.).
- Price . Fluorography is cheaper than x-rays, and this is the only reason why it is still used. It is worth considering the fact that if any pathologies are detected on the FLG, the patient may be referred for radiography to obtain a more accurate result and confirm the diagnosis.
X-ray of the lungs: preparation, technique, meaning, how to read, problems in the images
All information is provided for informational purposes only and does not constitute medical advice. The system, methods, methods of treatment, necessary medications can only be prescribed by your attending physician.
Chest X-ray (X-ray) is a simple, effective test that has remained relevant for over 100 years in helping to see any abnormalities in the chest cavity.
The value of the method is that it can show almost all serious pathologies at an early stage, suitable for emergency diagnosis and treatment monitoring. Therefore, it is a frequently performed method and can be performed on an outpatient basis or in a department using a stationary or portable X-ray machine.
Snapshot of healthy lungs

In a healthy person, the R-image clearly shows the fields of the lungs located on the sides of the spine. They do not block X-rays, so they look uniform and have no spots.
There is a heart in the center; on the right side its shadow should protrude no more than one centimeter. The collarbone is visible at the top. The dome-shaped diaphragm is clearly visible in the lower part. Normally, one half of it is raised relative to the other. Horizontal shadows are edges.
The bronchi are usually not visible. Their appearance indicates “smoker’s lungs” or chronic diseases (bronchiectasis or cavitary formations in them).
Also, the vascular pattern should not be visible; its strengthening indicates a violation of blood circulation, an increase in pressure in them, which is typical for cardiac pathology. Normally, the vessels are visible only near the roots in the central part. The roots should be clearly visible, have a standard size, and not be expanded. The trachea should be centrally located.
Important
If the radiologist sees a similar picture (without disturbances in blood supply, cavitary and cystic formations, signs of stagnation), then in the description protocol he will write a conclusion: the pulmonary pattern is not changed, has a clear shape, no pathological formations have been identified.
When required
Radiography, unlike fluorography, is a more informative method. Allows you to resolve doubts that arose after FLG. Therefore, doctors often refer for x-rays if strange “findings” are detected on fluorography. In these cases, you cannot do without an overview photo.
It is also preferable if a person works in hazardous work or has contact with a patient with tuberculosis.
X-rays are required in the following conditions:
- difficulty breathing, shortness of breath;
- prolonged coughing;
- chest injury and pain;
- elevated temperature of unknown origin;
- severe sweating;
- monitoring the effectiveness of treatment of various pulmonary diseases, such as pneumonia, cancer;
- the presence of blood or pus in the sputum;
- chest pain for no apparent reason;
- after an accident with multiple bruises.
What diseases does it detect?
Pathologies
- Chronic obstructive diseases (COPD) - emphysema and chronic bronchitis.
- Air outside the lungs (in the pleural cavity). The pathology is called pneumothorax.
- Infection (pneumonia).
- An abscess is a ring-shaped shadow that indicates a cavity.
- Fluid in an organ, which is a sign of heart failure
- Fluid around (pleural effusion).
- Blackouts (cancer, tuberculosis infection).
- Edema.
Chest bone problems:
- Chest contusion.
- Rib fractures.
- Clavicle fracture.
Heart problems:
- Dilated and enlarged (cardiomegaly) indicates heart failure, problems with the valves.
- Abnormal position of the heart (dextrocardia), when it is located in the right half of the chest
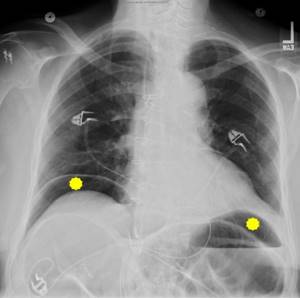
- To monitor the operation of pacemakers and the position of catheters
- Fluid around the heart (pericardial effusion) is pericarditis.
- Salt deposits - calcifications of the heart or blood vessels.
- Dilation or narrowing of the arteries, which suggests an increase in blood pressure in the pulmonary arteries, indicates pathology of the right side of the heart.
Aperture problems:
- Lowering or raising its dome.
- Protrusion (hernia).
- Wall sealing.
- The presence of gas or liquid under the diaphragm dome.
Normally, it has the shape of a slightly concave dome. Its right half should be higher than the left because of the liver. The difference is about 3 cm. Its outline should be smooth. A flattened (drooped) diaphragm is often seen in patients with chronic obstructive pulmonary disease (COPD) or pneumothorax.
Important
Chest X-ray allows you to practically make the correct diagnosis, start treatment in a timely manner and save a person’s life. It reveals the pathology of all organs of the chest, starting with the lungs and ending with the diaphragm. On an x-ray, shadows of 2 mm in size can be distinguished, and with fluorographic examination - at least 5 mm.
What kind of preparation
The study does not require special preparation. Smoking does not affect the diagnosis. It is advisable to reduce food intake, since with a full stomach the diaphragm moves slightly upward, therefore, the result may be distorted.
Pregnant women and children are of concern. Usually the attending physician decides on the need for x-rays in this category of patients.
Before the procedure, you should inform about the presence of a pacemaker or other implants. Leave jewelry at home, remove glasses, remove dentures.
Technique

X-rays are similar to photography. It is performed by a radiologist in a special room. The entire stage of implementation includes several mandatory steps:
- The patient is registered in the journal.
- Frees the upper half of the body from jewelry and clothing.
- If necessary, covers areas of the body that are not subject to examination with a lead apron.
- Placed between the film screen and the X-ray tube. Presses your chest or back tightly against the device.
- Takes a deep breath and holds it for a few seconds while the photo is taken.
At this time, the specialist is in another room and turns on the emitting device.
The procedure takes no more than five minutes and does not cause discomfort.
The examination can be performed in a standing, lying or sitting position. The radiologist begins the description immediately and gives the result to the patient. The image can then be shown to your doctor or any other specialists if necessary.
General radiography is usually done, but the direction may indicate the need for targeted R-graphy. It provides more information on a specific area, allowing a better study of the pathological area.
Why do you need x-rays in two projections?
There are two types of R-images - frontal and lateral projections. In a straight position, it is not always possible to see infiltrates of the upper lobe of the lung. A side shot allows you to study them in more detail. It also shows the paths to the roots better, indicating, for example, tuberculosis.
The direct position does not always “see” pneumonia, since the lung consists of segments, and in the direct projection they are layered on top of each other. Diagnostics from both sides allows you to better determine the size of the heart. To more accurately identify central and peripheral cancer.
Also, on lateral photographs, small foci of infiltration, abscesses, and cysts are more clearly visible; in this case, they are not covered by the sternum.
Are X-rays dangerous?
X-rays are a form of radiation such as light or radio waves. They pass well through most objects, including the body. Some patients are concerned that they are contributing to cancer.
The amount of radiation a person receives from a chest x-ray is much less than the natural radiation from the Earth that we are exposed to every day.
Radiation is dangerous if its total dose exceeds a threshold level (more than 1 millisievert in one session).
During FLG, the patient receives a dose of up to 0.8 mSv, and for one x-ray – 0.3 mSv. A 16-hour flight is equivalent to one x-ray.
The highest dose is received from a CT scan (computed tomography) - about 4 mSv, which is 30-40 times higher than the dose from an X-ray. So, CT scans must be done according to strict indications.
For life-threatening diseases, harm from radiation will be the least evil for the patient. The diagnosis has no contraindications, but there are age restrictions. It is not advisable to perform the procedure on children under 14 years of age and pregnant women.
How to “read” an R-image
To correctly describe an image, you need knowledge of various forms of diseases and extensive practical experience. It is difficult for the average person to “read” an x-ray. Even doctors sometimes disagree on the images they receive.
Still, some concepts are worth getting acquainted with. Various types of compactions, white spots (accumulation of air or liquid), shadows in the area of the lung fields are considered dangerous. They talk about pathological processes.
Different parts of the body transmit rays differently. Dense bone (ribs and spine) absorbs most of the radiation and appears white in the image, while soft tissue such as muscle, fat, and organs allows x-rays to pass through and absorbs less, so they appear darker.
As a result, on an x-ray we see bones as white, soft tissue as gray, and air as black.
Do not panic if a shadow is detected in the lung. It can indicate not only a dangerous disease, but also a defective film. The occurrence of shadows can be caused by many reasons and are not always life-threatening.
Radiologists have a whole classification of shadows according to size, degree of compaction, shape, and location. For example, a spot that is ominous for us may not cause alarm to a radiologist, and may be interpreted as residual effects of a killed infection. Distinguishing signs that seem insignificant at first glance will tell him about this.
The table below presents a list of diagnoses with the corresponding x-ray pattern for each of them:
| Disease | Characteristic changes |
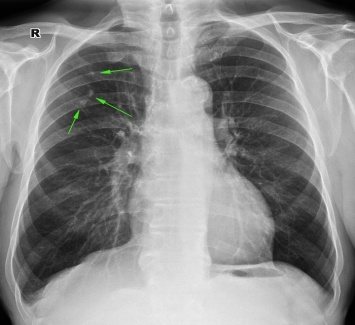
| Tuberculosis | A large number of small blackouts. A large, round shadow may indicate advanced tuberculosis. |
| Edema | Unevenly scattered shadows resembling flakes. |
| Exudative pleurisy | A thin dark line, usually along the lower edge of the costal arch. The trachea is displaced or stretched |
| Venous stagnation | The basal zones resemble the wings of a moth, which indicates stagnation of blood in the pulmonary circulation (or basal pneumonia). |
| Cancer | Round formations, different in size, having a strictly defined line along the contour. |
| Emphysema | Consolidation of the diaphragm, high airiness of the lung fields. |
| Peritonitis | Due to the concentration of gases in the peritoneal area, there is no clearing under the dome of the diaphragm. |
| Abscess | Ring shadow. |
| Atelectasis (collapsed lung) | Intense (black) uniform darkening of the entire lung, lobe or segment. On the affected side, the dome of the diaphragm is raised high. |
| Heart failure | The heart's shadow takes on a rounded shape on the right or left. With an enlarged right ventricle, darkening is visualized on the left |
| Silicosis (dust) | Finely scattered diffuse nodular opacities with relative sparing of the lower lung zones |
What diseases look like on R-images
| Problems: | |
| 1. Chronic obstructive pulmonary diseases (COPD) - emphysema and chronic bronchitis. The image shows flattening of the diaphragm, excessive clearing of the lung fields, and expansion of the roots. An x-ray will not show acute bronchitis. |
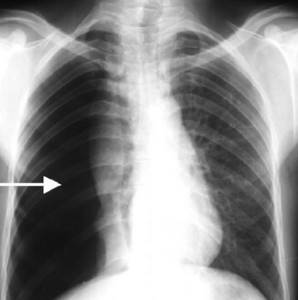
| 2. Air behind the lungs (in the pleural cavity). As a result of air entering the pleural cavity, we see partial or complete collapse. The pathology is called pneumothorax. |
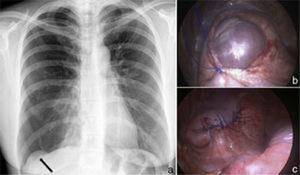
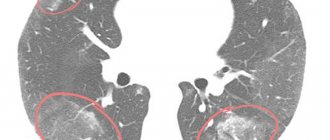
| 3. Infection (pneumonia). An area of clearing is visible. |
| 4. Abscess. A ring-shaped shadow indicates a cavity. | |
| 5. Fluid in the organ (heart failure). Bilateral pleural effusions are present in 70% of patients with congestive heart failure. | |
| 6. A lesion in the lungs (cancer, tuberculosis infection). We see a spot. | |
Chest bone problems: | |
| 1. Chest contusion. There are small inflammatory infiltrates in both lungs. | |
| 2. Rib fractures. |
| 3. Fracture of the collarbone. |
Heart problems: | |
| 1. Expansion. Enlarged (cardiomegaly). Occupies 50% of the size of the chest, an increase suggests its expansion (cardiomegaly) or pericardial effusion. |
| 2. Calcium deposits. Calcium deposits in the organ are most often associated with an old, cured infection. This nodule appears firm and white and has the same density as bone. |
Aperture problems: | |
| 1. Flattening, indicating dilated lungs, characteristic of COPD and emphysema. |
| 2. Right-sided pneumothorax without mediastinal displacement and diaphragmatic hernia (indicated by an arrow). |
| 3. Free air under the diaphragm (indicated in yellow) |
Types of R-visualization, their advantages
Most often, conventional film X-rays are used in medical institutions. For this, it is necessary to purchase film on which X-rays passing through the human body form an image of the lung.
Such a film requires development using harmful chemicals and exists in a single copy. The main disadvantage of analog X-rays is the higher radiation dose and the contact of medical personnel with harmful substances during the development process. Artifacts of the film itself due to pulsation of large vessels and movements during the act of breathing cannot be excluded.
Digital X-ray is a completely different matter. Instead of film, a digital receiver is used, which converts the rays into an image on a computer. It can be copied, processed, sent electronically, and recorded on other digital media. The radiation dose on a digital device is 8-10 times less.
Recording an image on a digital medium provides a unique opportunity to view images over time (important for chronic diseases), make the required number of copies, highlight individual areas, enlarge and print the resulting image.
The method will be of great help to specialists in the therapeutic department, accurately detecting pneumonia, bronchitis, pleurisy, and tuberculosis. Cardiologists will show heart defects.
A gastroenterologist will help diagnose a diaphragmatic hernia, and a pediatrician will help diagnose spinal curvature. Endocrinologists using a digital device will be able to identify thyroid diseases at an early stage.
Important
Digital radiography increases the efficiency of research and has a low radiation dose. Due to the high resolution, the images are clearer and more contrasty, which allows you to better assess the nature of the compaction and identify the shadow. Diagnose a tumor in the initial stage of development.
In severe cases, when the patient is not transportable, it is possible to take an x-ray at home or in the ward. The procedure is performed on a portable mobile or portable X-ray device. The device runs on a battery. It is suitable for all radiographic procedures in emergency and intensive care wards, ideal for pediatric wards.
Another radiological method is fluoroscopy. It allows visualization of the organ in real time. You can examine the pathology in the breathing process and evaluate the mobility of the diaphragm. R-copy is used in case of loss of elasticity of the lungs and suspected bronchial obstruction.
In controversial and unclear situations, this additional examination method is used. The decision to conduct it remains with the attending physician.
What are the benefits and risks of R-graphy
Chest radiography greatly aids in diagnosis by providing general guidance as an initial diagnostic test and is particularly useful in diagnosing pneumonia, cancer, and chronic obstructive disease.
Advantages of the method:
- accessible and relatively safe;
- inexpensive, highly informative method;
- acts as a document important in resolving issues of disability;
- especially useful in emergency diagnosis;
- free of side effects in the typical diagnostic range;
- The equipment used is inexpensive and therefore available for emergency departments, doctors' offices, ambulatory care centers, and nursing homes.
At the same time, the risks are minimal, and the benefits significantly outweigh the harm. Don't be afraid of R-examination. It should be done in case of sudden complaints of shortness of breath, persistent cough with hemoptysis, chest pain associated with breathing, despite the fact that FLG or radiography was recently done.
Be attentive to yourself and your health, use this informative and safe diagnostic method in a timely manner.
Material prepared by: Maslikhova Lyubov Vasilievna
Last modified: 2021-08-12 Date of writing: 2019-11-22
What to choose: X-ray or fluorography
We have already talked about the advantages and disadvantages of each x-ray examination method, now let’s summarize. X-rays can easily replace conventional fluorography and give a more complete picture of your health, confirming the absence of pathologies and symptoms of diseases. Fluorography can only act as the simplest, most basic research method. It is not suitable for more accurate diagnosis and diagnosis. If it is necessary to clarify the data, the doctor will still send you for an x-ray.
If you intend to undergo a medical examination and make sure that everything is fine with you, then it is better to sign up for a chest x-ray. By modern standards, the study will cost a little more, but possible pathology can be detected at an earlier stage. The procedure takes only a few minutes, and is interpreted by an experienced radiologist at our medical center.
Contraindications to X-rays
X-rays should not be taken for pregnant women at any stage, as well as for children under 15 years of age. In some cases, the patient's condition may be an obstacle to conducting the study. A patient in a supine position cannot undergo the study due to the inability to assume an upright position. In an inadequate condition, when the patient cannot stand still, signs of pneumonia on an x-ray cannot be recorded properly.
How often can an x-ray be taken for pneumonia?
A confirmed diagnosis is an indication for regular x-ray examinations to monitor the course of the disease. Whether the treatment prescribed by the doctor helps will show what pneumonia looks like on an x-ray. In this regard, many patients are concerned about how often this procedure can be performed without harm to health. After the start of treatment, depending on the type of disease, an x-ray for pneumonia must be done after 6-10 days. If positive dynamics are noticed, treatment continues as it was started. The patient, who is considered to be cured, is subsequently re-examined after 1, 3 and 6 months. With favorable treatment, the patient receives a small dose of radiation, far from acceptable levels. This is possible thanks to the development of medical technologies and protective measures during the procedure.
The Downside of CT Scanning
In addition to the important advantages, it is necessary to pay attention to the negative and sometimes dangerous aspects of computed tomography:
- High radiation dose . When undergoing a tomography, a patient may receive a dose 10-20 times greater than during a conventional x-ray examination.
- The effect of ionizing radiation is quite strong and can damage the DNA molecule . Over the years, these breakdowns accumulate. And if the body cannot restore them, oncology may develop. The most common cancers associated with radiation examinations are lung, thyroid and breast cancer.
- Use of X-ray contrast agents . They are used to improve visualization of blood vessels and internal organs. In the most common of them, the main component is iodine. These substances have many contraindications: diseases of the thyroid gland, liver, heart, etc.
- An allergic reaction may develop to X-ray contrast agents . Allergy to iodine is a fairly common phenomenon. It can be in the form of local manifestations: phlebitis, necrosis of soft tissue at the injection site. But there are also more dangerous, systemic manifestations in the form of urticaria, angioedema, toxic effects on the liver and kidneys, up to anaphylactic shock.
- Tomography is contraindicated for pregnant and lactating women .
- For children, computed tomography is performed only according to strict indications , and only under anesthesia. Anesthesia is necessary to ensure that the child does not move during the examination.
- Frequent computed tomography is not recommended for people with cancer . There is a high risk of relapse under the influence of X-rays.

X-ray radiation
In order to assess the degree of influence of ionizing radiation used in fluorography on the human body, it is necessary to distinguish between the following types of irradiation:
- physical;
- absorbed;
- equivalent;
- effective.
There are several types of radiation that are generated during the decay of radionuclides, the energy, quantity and penetrating ability of which have different effects on the body. The amount of damage caused to the body depends entirely on the amount of energy transferred to the tissues and is called the Radiation Dose (D). Physical exposure is the amount of energy emitted by an x-ray or other radionuclide that can ionize the air. The unit of measurement for physical exposure is the Roentgen (r).
Absorbed energy is the energy transferred to an organism under the influence of physical (exposure) radiation. The amount of absorbed energy is measured in Grays (Gp). With an irradiation intensity of 1p, its absorption by tissues will be 0.93 rad, that is, 1p = 0.93 rad, and 1 rad = 0.01Gp.
However, when using this calculation system, the type of radiation (α-, β- or γ-radiation) is not taken into account, the destructive ability of which varies significantly. To correctly assess the biological effect caused by each specific unit of radioactive substance, coefficients (K) are used. For β-, γ- and X-ray radiation, the coefficient is 1, and for α-radiation -20.
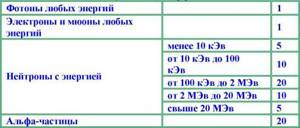
Coefficients used to calculate equivalent energy
Thus, the equivalent dose of absorbed energy is the amount of absorbed energy multiplied by a coefficient reflecting the destructive ability of a particular type of energy. Until 1979, this indicator was measured in rem (biological equivalent of x-rays). Today, the unit of measurement 3ivert (3v) is more often used, with 1 3v = 100 rem.
Effective exposure is a value that evaluates the risk of developing long-term consequences of exposure to radiation on any organs of the human body. This indicator is assessed based on the sensitivity of a particular organ to the effects of ionizing radiation, for example, with equal time and power of exposure to α-rays on the body, the risk of malignant degeneration of lung tissue is much higher than that of thyroid tissue.
A quantitative indicator of the total effective dose of radiation is obtained by adding the equivalent doses received by each organ of the human body, multiplied by the sensitivity factor for these organs. The unit of measurement for effective radiation dose is also 3ivert. To more fully reflect information about the rate of accumulation of the critical value of ionization of the body (radiation power), the unit of measurement 3v/T is used, where T is a time interval (second, hour, day or year).
Conclusions and recommendations
Of course, if we compare CT and fluorography, then CT can cause more harm to the body. Because the dose received during tomography is tens and sometimes hundreds of times higher than in fluorography. But we must not forget that, despite the dose, CT is a more informative method. And, sometimes, you can’t do without it.
To reduce the risk of negative consequences, doctors advise following the following recommendations:
- Perform X-ray examinations strictly according to indications .
- Remember that the benefits of the study must outweigh the risks . Those. if a tumor is suspected, then it is more important to find and remove it, and not to be afraid of the consequences of radiation.
- You can consult a doctor and replace the computed tomography with magnetic resonance imaging . If this does not interfere with the diagnosis and you have no contraindications to it.
- If a woman is breastfeeding and needs to undergo an x-ray examination, it is recommended to express milk in advance before the examination.